研究[1-2]显示骨性Ⅲ类错
目前,既往关于前方牵引的研究主要集中在牵引力大小和方向方面,鲜有针对不同牵引位置、前方牵引配合不同扩弓方式的研究,且何种牵引位置及扩弓方式能最大限度地促进上颌骨骨缝生长、不同的牵引位置及扩弓方式对上颌骨旋转存在何种影响尚无明确结论。基于此,本研究通过建立牙支持式快速扩弓、骨支抗式快速扩弓联合前方牵引的三维有限元模型并设置不同的牵引位置,对颅颌面骨缝应力的分布特征以及颅颌面骨骼点、颅颌面骨骼、上颌牙列的位移趋势进行分析,以期为临床中骨性Ⅲ类错
1 对象和方法
1.1 研究对象
选择一名处于替牙列期的骨性Ⅲ类错
1.2 模型构建
本研究使用锥形束计算机断层扫描(cone beam computed tomography,CBCT)技术对患者行头颅扫描,并将已保存的CBCT数据导入医学建模软件Mimics 21.0中,初步建立上颌复合体三维有限元模型。
而后,基于初步构建的上颌复合体模型中第一磨牙间牙弓宽度及牙列大小,并参考临床扩弓器与前方牵引矫治器的尺寸,本研究应用Solidworks 2021软件分别生成骨支抗式快速扩弓联合前方牵引、牙支持式快速扩弓联合前方牵引的三维有限元模型。其中,牙支持式快速扩弓联合前方牵引装置由扩弓器主体、导轨、前牵引钩和双侧上颌第一磨牙上的带环构成,骨支抗式快速扩弓联合前方牵引装置则在上述部件的基础上向扩弓器主体引入2颗微种植钉;同时,2种快速扩弓器的前牵引钩均由双侧上颌第一磨牙带环颊侧伸出。
最终,将上述2种快速扩弓联合前方牵引装置分别与上颌复合体模型进行组装,并导入Ansys workbench 2021软件中,以建立上颌复合体和骨支抗式快速扩弓联合前方牵引三维有限元模型(模型1)、上颌复合体和牙支持式快速扩弓联合前方牵引三维有限元模型(模型2)。
1.3 模型的条件设置
表1 模型1和模型2中各种材料的杨氏模量与泊松比
Tab 1
| Material | Young′s modulus/(N·mm-2) | Poisson′s ratio |
|---|---|---|
| Craniofacial bones | 13 400 | 0.30 |
| Sutures | 70 | 0.40 |
| Maxillary dentition | 20 700 | 0.30 |
| Expander | 190 000 | 0.33 |
| Microimplant | 113 000 | 0.33 |
依据既往文献[12],本研究对模型1和模型2的接触条件进行设置,即将皮质骨与骨缝间、牙与牙周膜间、牙周膜与上颌骨间、微种植钉与上颌骨间、带环与上颌第一磨牙间的界面设置为绑定接触,将导轨和扩弓器主体间设置为无摩擦,将相邻牙体间、前牵引钩与上颌牙列间的摩擦系数设置为0.2。
1.4 坐标系及上颌牙列的位移趋势设置
以腭中缝作为原点建立统一坐标系,X轴为水平向,以模型左侧为正、右侧为负;Y轴为矢状向,以模型后方为正、前方为负;Z轴为垂直向,以模型上方为正、下方为负。同时,本研究使用该统一坐标系来描述中切牙、第一磨牙的位移趋势,X、Y、Z轴正方向分别代表中切牙牙冠向近中、腭向、压低位移,第一磨牙牙冠向腭向、远中、压低位移;X、Y、Z轴负方向分别代表中切牙牙冠向远中、唇向、伸长位移,第一磨牙牙冠向颊向、近中、伸长位移。
1.5 施加载荷
根据既往文献[13],本研究于模型1和模型2中的扩弓器两侧沿水平向分别施加0.25 mm的强制位移,并于快速扩弓联合前方牵引装置双侧的牵引钩处施加与
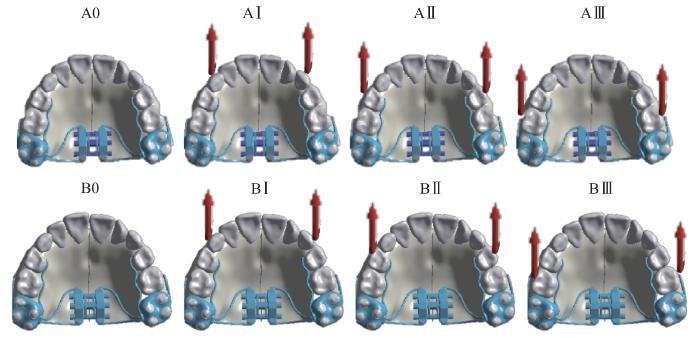
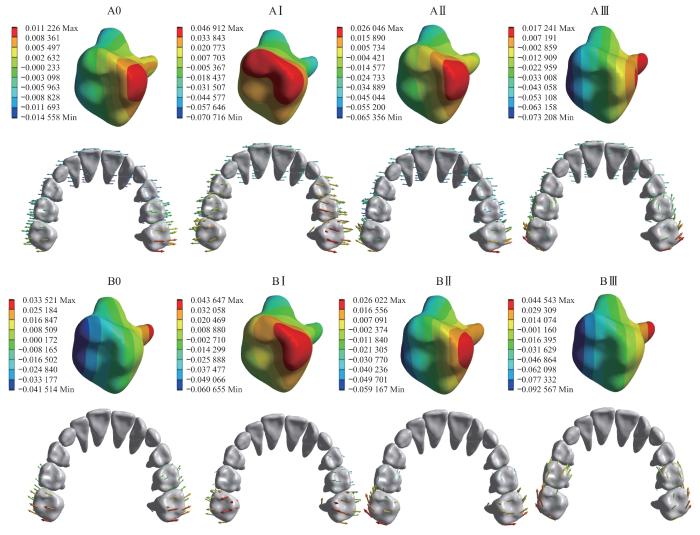
1.6 工况设置
基于快速扩弓方式的不同,将模型1设置为A组、模型2设置为B组;而后,考虑到牵引位置的不同,我们将A、B组继续分为3个亚组(记为试验组),即将牵引钩位于双侧尖牙颊侧记为Ⅰ组、位于双侧第一前磨牙颊侧记为Ⅱ组、位于双侧第二前磨牙颊侧记为Ⅲ组。同时,分别将A、B组中不联合前方牵引设置为对照组,即为A0组、B0组。最终,本研究共建立了8个工况,即工况1~8依次为A0、AⅠ、AⅡ、AⅢ、B0、BⅠ、BⅡ、BⅢ(图1)。
图1
图1
模型1和模型2的8个工况设置
Note: Red arrows represent traction sites and directions.
Fig 1
Eight conditions of Model 1 and Model 2
1.7 观察指标
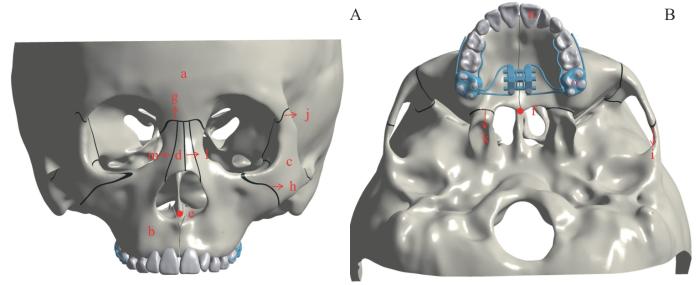
选取如下对象(图2)对模型1、模型2进行观察:① 颅颌面骨骼,包括额骨、上颌骨、颧骨、鼻骨。② 颅颌面骨骼点,包括后鼻嵴点(posterior nasal spine,PNS)、前鼻嵴点(anterior nasal spine,ANS)。③ 颅颌面骨缝,包括鼻额缝、颧颌缝、颧颞缝、颧额缝、翼突上颌缝、鼻中缝、鼻颌缝。④ 上颌牙列,包括上颌中切牙、第一磨牙。由于模型1、模型2为左右对称结构,因此仅对右侧模型进行测量,并对该2个模型的颅颌面骨缝应力分布特征(包括等效应变、最大主应变)以及颅颌面骨骼点、颅颌面骨骼、上颌牙列的位移趋势进行分析。
图2
图2
模型的观测对象的示意图
Note: A. Anterior aspect of the model. B. Inferior aspect of the model. a—frontal bone; b—maxilla; c—zygomatic bone; d—nasal bone; e—ANS; f—PNS; g—nasofrontal suture; h—zygomaticomaxillary suture; i—zygomatic temporal suture; j—zygomatic frontal suture; k—pterygomaxillary suture; l—nasal suture; m—nasomaxillary suture; n—maxillary central incisors; o—maxillary first molars.
Fig 2
Schematic diagram of observation objects of the model
2 结果
2.1 三维有限元模型的构建
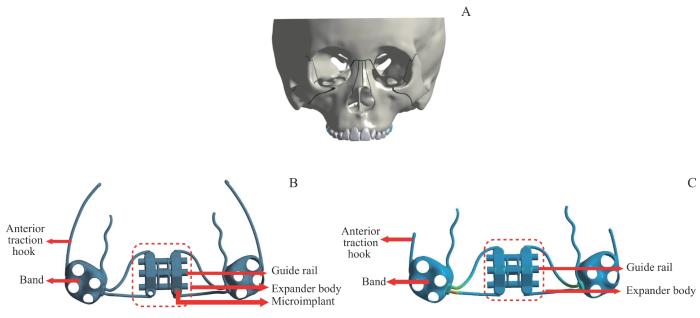
图3
图3
上颌复合体三维有限元模型和2种快速扩弓联合前方牵引三维有限元模型图示
Note: A. Three-dimensional finite element model of maxillary complex. B. Three-dimensional finite element model of bone-anchored rapid expansion with protraction. C. Three-dimensional finite element model of tooth-borne rapid expansion with protraction.
Fig 3
Diagram of the three-dimensional finite element model of maxillary complex and two rapid expanders with protraction
图4
2.2 颅颌面骨缝应力分布特征的分析
2.2.1 骨缝等效应变的分析
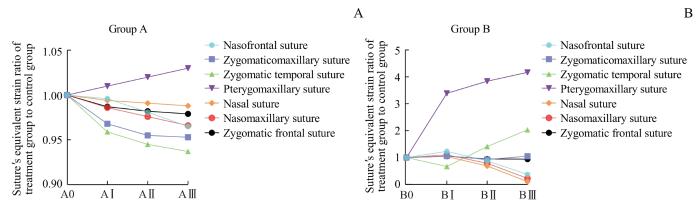
通过计算试验组等效应变与其对应的对照组等效应变的比值来描述骨缝等效应变的变化趋势,比值越大则骨缝等效应变越大。如图5所示,A、B组中翼突上颌缝等效应变最大,且随着牵引位置的后移其等效应变均逐渐增加。
图5
图5
骨支抗式扩弓联合前方牵引(A)和牙支持式扩弓联合前方牵引(B)的试验组与对照组骨缝等效应变的比值
Fig 5
Experimental group-to-control group ratio of sutures′ equivalent strain of bone-anchored rapid expander with protraction (A) and tooth-borne rapid expander with protraction (B)
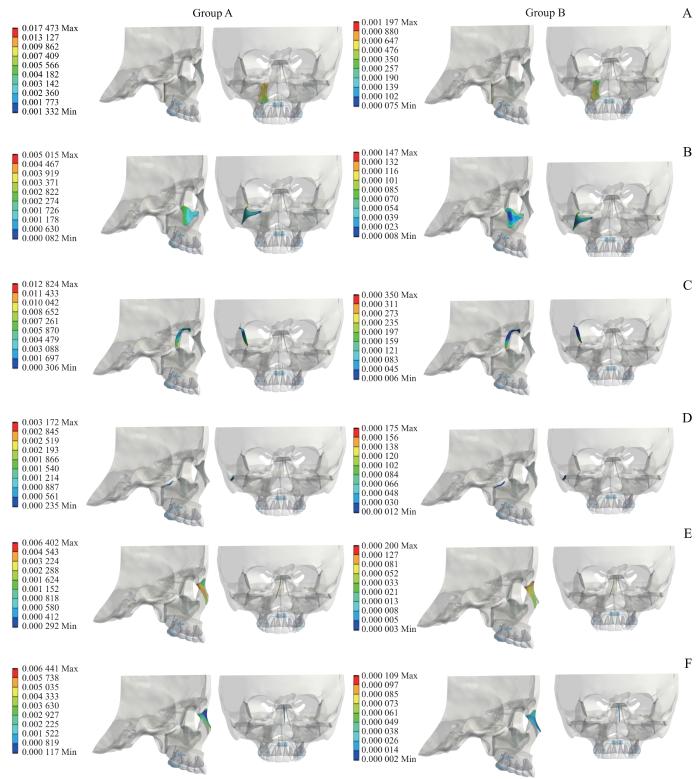
2.2.2 骨缝最大主应变的分析
在三维应力状态下,最大主应变力为材料中承受的最大拉伸应力或压缩应力。在本研究中最大主应变代表骨缝的拉伸情况,可提示潜在的应力集中区域。因此,我们以在Ⅰ处牵引(AⅠ、BⅠ)来代表A、B组的情况进行展示。图6为AⅠ、BⅠ组各骨缝的最大主应变示意图。通过图例上标尺的数量级可看出:AⅠ组各骨缝最大主应变均大于BⅠ组,翼突上颌缝的最大主应变均大于其他各骨缝,即AⅠ组各骨缝拉伸效应大于BⅠ组,翼突上颌缝的拉伸效应大于其余各骨缝。AⅠ组中翼突上颌缝的中上部分拉伸效应最大,即该部分成骨增加,进而出现上颌骨的顺时针旋转;BⅠ组中翼突上颌缝靠近模型下方的区域拉伸效应最明显,与AⅠ组结果相反,呈现上颌骨的逆时针旋转(图6A)。AⅠ组中鼻颌缝拉伸效应分布较均匀,最大值靠近模型后方;BⅠ组中鼻颌缝最大主应变的最大值出现在模型上方即鼻根附近(图6E)。与鼻颌缝相似,AⅠ组中鼻中缝拉伸效应集中在模型后方,BⅠ组中主要体现在鼻根附近(图6F)。
图6
图6
AⅠ、BⅠ组各骨缝的最大主应变图示(右视图及前视图)
Note: A. Pterygomaxillary suture. B. Zygomaticomaxillary suture. C. Zygomatic temporal suture. D. Zygomatic bone. E. Nasomaxillary suture. F. Nasofrontal suture. In scale label, positive value represents tensile stress, and negative value represents compressive stress. Based on the right and frontal views of the nasofrontal suture, which are represented as points and lines with relatively small values, no analysis was conducted on the nasofrontal suture in this area.
Fig 6
Diagram of sutures′ maximum principal strain of Group AⅠ and Group BⅠ (right view and front view)
2.3 颅颌面骨骼的三维方向位移趋势分析
2.3.1 颅颌面骨骼位移大小的总体变化
表2 颅颌面骨骼在 X 轴上的位移/mm
Tab 2
| Cranio-maxillofacial bone | Group A | Group B | ||||||
|---|---|---|---|---|---|---|---|---|
| A0 | AⅠ | AⅡ | AⅢ | B0 | BⅠ | BⅡ | BⅢ | |
| Frontal bone | -0.063 97 | -0.064 05 | -0.063 98 | -0.063 93 | -0.003 08 | -0.003 52 | -0.002 89 | -0.002 24 |
| Maxilla | -0.063 97 | -0.064 05 | -0.063 98 | -0.063 93 | -0.003 08 | -0.003 52 | -0.002 89 | -0.002 24 |
| Zygomatic bone | -0.045 22 | -0.045 16 | -0.045 05 | -0.044 98 | -0.001 53 | -0.001 67 | -0.001 33 | -0.000 99 |
| Nasal bone | -0.024 05 | -0.023 81 | -0.023 73 | -0.023 71 | -0.000 48 | -0.000 35 | -0.000 16 | -0.000 04 |
表3 颅颌面骨骼在 Y 轴上的位移/mm
Tab 3
| Cranio-maxillofacial bone | Group A | Group B | ||||||
|---|---|---|---|---|---|---|---|---|
| A0 | AⅠ | AⅡ | AⅢ | B0 | BⅠ | BⅡ | BⅢ | |
| Frontal bone | 0.027 70 | 0.027 40 | 0.027 30 | 0.027 30 | 0.001 00 | 0.000 77 | 0.000 63 | 0.000 62 |
| Maxilla | -0.008 59 | -0.009 51 | -0.009 81 | -0.010 00 | -0.000 61 | -0.003 45 | -0.003 89 | -0.004 34 |
| Zygomatic bone | -0.009 50 | -0.009 87 | -0.009 98 | -0.010 01 | -0.000 27 | -0.001 05 | -0.001 26 | -0.001 42 |
| Nasal bone | 0.024 60 | 0.024 40 | 0.024 25 | 0.024 21 | 0.000 93 | 0.000 77 | 0.000 56 | 0.000 37 |
表4 颅颌面骨骼在 Z 轴上的位移/mm
Tab 4
| Cranio-maxillofacial bone | Group A | Group B | ||||||
|---|---|---|---|---|---|---|---|---|
| A0 | AⅠ | AⅡ | AⅢ | B0 | BⅠ | BⅡ | BⅢ | |
| Frontal bone | 0.026 51 | 0.026 10 | 0.025 80 | 0.025 70 | 0.001 10 | 0.000 64 | 0.000 32 | 0.000 31 |
| Maxilla | 0.023 89 | 0.023 40 | 0.023 20 | 0.023 10 | 0.001 05 | 0.000 36 | 0.000 18 | 0.000 11 |
| Zygomatic bone | 0.021 34 | 0.020 90 | 0.020 80 | 0.020 70 | 0.000 70 | 0.000 36 | 0.000 20 | 0.000 10 |
| Nasal bone | -0.018 22 | -0.018 00 | -0.017 80 | -0.017 70 | -0.000 70 | -0.000 63 | -0.000 35 | -0.000 07 |
2.3.2 颅颌面骨骼位移大小随牵引位置改变的变化趋势
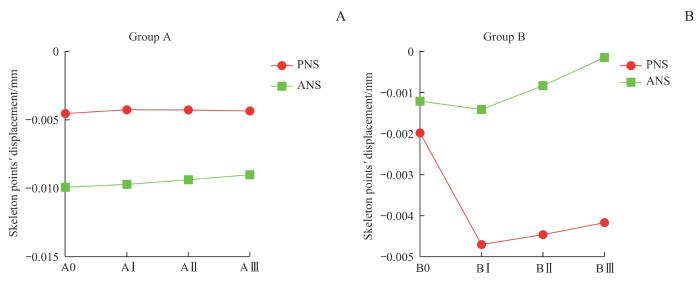
2.4 颅面骨骨骼点位移大小及其随牵引位置改变的变化趋势
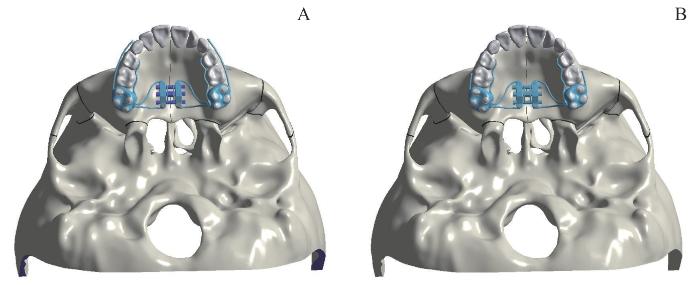
如图7所示,垂直向上(Z轴),ANS、PNS均产生向下的位移。A0组中,ANS的向下位移大于PNS即上颌平面(ANS-PNS平面)发生顺时针旋转,且随着牵引位置的后移,A组ANS的向下位移减少、PNS的向下位移增加,表明上颌平面顺时针旋转趋势减小;B0组中,ANS的向下位移小于PNS即上颌平面发生逆时针旋转,且随着牵引位置的后移,ANS和PNS的向下位移相差逐渐增大,即上颌平面逆时针旋转趋势更加明显。
图7
图7
A组(A)、B组(B)的各骨骼点(ANS、PNS)在垂直向上( Z 轴)的位移趋势
Fig 7
Displacement trend of each skeletal point (ANS, PNS) in Group A (A) and Group B (B) in the vertical direction (Z-axis)
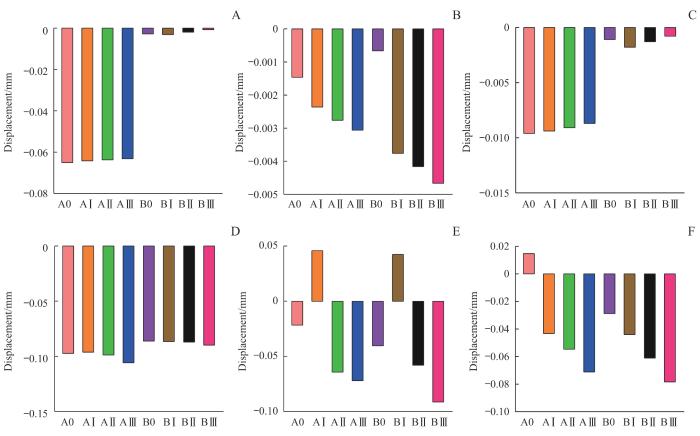
2.5 上颌牙列位移随牵引位置改变的变化趋势
2.5.1 上颌中切牙位移随牵引位置改变的变化趋势
如图8所示,A、B试验组上颌中切牙的位移趋势基本相同,即随着牵引位置的后移,水平向上上颌中切牙的远中位移趋势减小,矢状向上唇向位移趋势增加,垂直向上伸长位移趋势减小。
图8
图8
A、B组上颌中切牙和上颌第一磨牙的三维方向的位移分析
Note: A‒C. Displacement analysis of maxillary central incisor in the horizontal direction (A), sagittal direction (B) and vertical direction (C). D‒F. Displacement analysis of maxillary first molar in the horizontal direction (D) sagittal direction (E) and vertical direction (F).
Fig 8
Three-dimensional displacement analysis of maxillary central incisors and maxillary first molars in Group A and Group B
2.5.2 上颌第一磨牙位移随牵引位置改变的变化趋势
图9
图9
A、B组的上颌第一磨牙的位移趋势图示
Note: The color of the arrow represents the magnitude of displacement, and the direction of the arrow represents the direction of displacement.
Fig 9
Diagram of the displacement trend of the maxillary first molar in Group A and Group B
3 讨论
3.1 骨缝等效应变
等效应变是指物体在受到外力作用时发生的形变,其与等效应力都可用来描述受力物体的形变大小。本研究发现,A、B组的各骨缝中翼突上颌缝的等效应变最大且A组均大于B组,提示骨支抗式快速扩弓联合前方牵引更有利于促进上颌骨的向前方生长;随着牵引位置的后移,2组翼突上颌缝等效应变均逐渐增大,且在Y轴上上颌骨向模型前方位移趋势也逐渐增大,由此推测翼突上颌缝等效应变与上颌骨向前方位移趋势变化可能呈正相关。
3.2 骨缝最大主应变
最大主应变可反映骨缝的拉伸效应。本研究发现:AⅠ组中颧颌缝、颧额缝、颧颞缝靠近模型后方拉伸明显,即与骨缝后方相连的骨骼生成量较大;BⅠ组中颧颌缝、颧额缝、颧颞缝拉伸效应均集中于靠近上颌后牙一侧,可能与牙支持式扩弓产生的牙性效应相关。在AⅠ组中,翼突上颌缝中上方拉伸效应明显,成骨增加,进而出现上颌骨的顺时针旋转;与AⅠ组相反,BⅠ组呈现了上颌骨的逆时针旋转。提示骨支抗式快速扩弓联合前方牵引会导致上颌平面发生顺时针旋转,牙支持式快速扩弓联合前方牵引可导致上颌平面发生逆时针旋转;鼻颌缝和鼻中缝在2组中均为后方拉伸效应明显,即鼻骨生长呈现楔形效应,四周鼻骨逐渐向前生长,中心鼻骨相对位移向后。
3.3 骨骼在三维方向的位移及位移趋势
骨性Ⅲ类错
3.4 骨骼点在三维方向的位移及位移趋势
根据骨骼点ANS、PNS在垂直向上(Z轴)的位移方向和大小可判断上颌平面的旋转方向[17]。本研究发现:A组中上颌平面发生了顺时针旋转,有利于开
3.5 上颌牙列在三维方向的位移及位移趋势
本研究发现:在矢状向上随着牵引位置的后移,A、B试验组第一磨牙从远中位移(AⅠ)转为近中位移(AⅡ、AⅢ),这可能是由于随着牵引钩位置的后移,第一磨牙受力的力臂逐渐减小,力矩也减小,导致其远中位移转为近中位移;同时,在Ⅰ处牵引时A组第一磨牙比B组发生远中位移的更多,在Ⅱ、Ⅲ处牵引时A组第一磨牙比B组发生近中位移的更少。这提示骨支抗式快速扩弓联合前方牵引有利于减少第一磨牙的近中位移,适合于后牙段存在拥挤的患者。此外,我们还发现A、B试验组中第一磨牙均表现为颊倾、伸长位移,因此临床上对于下颌平面角偏大的患者需谨慎使用骨支抗式和牙支持式快速扩弓矫治器,以防止第一磨牙进一步伸长、下颌平面角进一步增大,必要时需使用后牙
综上,本研究发现随着牵引位置向后移动,上颌骨向前位移量逐渐增加。同时,根据骨骼点ANS、PNS位移变化我们还发现,A组中上颌平面发生了顺时针旋转,有利于开
作者贡献声明
韩磊参与了研究设计、数据收集、统计分析和文章撰写;鲁桐和朱培香参与了数据收集、统计分析和文章撰写;李煌参与了研究设计和文章审阅。所有作者均阅读并同意了最终稿件的提交。
AUTHOR's CONTRIBUTIONS
HAN Lei participated in the research design, data collection, statistical analysis and manuscript writing. LU Tong and ZHU Peixiang participated in the data collection, statistical analysis and manuscript writing. LI Huang participated in the research design and manuscript review. All the authors have read the last version of paper and consented for submission.
利益冲突声明
所有作者声明不存在利益冲突。
COMPETING INTERESTS
All authors disclose no relevant conflict of interests.
参考文献
 畸形: 20例病例临床分析[J]. 口腔正畸学, 2000, 7(3): 118-122.
畸形: 20例病例临床分析[J]. 口腔正畸学, 2000, 7(3): 118-122.
 的疗效差异分析[J]. 中华口腔医学杂志, 2023, 58(4): 318-328.
的疗效差异分析[J]. 中华口腔医学杂志, 2023, 58(4): 318-328.
 平面水平向后牵引猴上颌骨矫形作用的三维有限元研究[J]. 华西口腔医学杂志, 2014, 32(2): 196-199.
平面水平向后牵引猴上颌骨矫形作用的三维有限元研究[J]. 华西口腔医学杂志, 2014, 32(2): 196-199.