CKD的定义是肾脏结构或功能异常>3个月[1]。育龄期女性的慢性肾脏疾病范围广泛,常见的妊娠期CKD包括原发性肾小球疾病(IgA肾病、局灶节段性肾小球硬化、膜性肾病等)、继发性肾小球疾病(如狼疮肾炎和糖尿病肾病)、肾小管疾病、遗传性肾小球疾病(如Alport综合征)等[3]。但临床上很多孕妇未行肾穿刺,不能按照病理类型进行分类,只能根据临床症状和实验室检查进行诊断,如肾病综合征或慢性肾炎。孕期母体肾脏负担加重,CKD患者妊娠面临较大风险,如原有疾病的加重、原有肾脏病分期增加、尿蛋白升高、发生急性肾损伤(acute kidney injury,AKI);妊娠母体并发症风险如妊娠期高血压、子痫前期或子痫等,严重时可导致患者死亡;胎儿不良结局的风险如流产、早产、死胎、低出生体质量儿、小于孕龄儿、入住新生儿重症监护病房(neonatal intensive care unit,NICU)等[4]。CKD增加了不良母婴结局的风险,但有关CKD患者发生不良妊娠结局的危险因素研究,目前仍鲜见报道。
本研究拟对妊娠合并CKD患者的临床资料进行分析,以寻找导致不良妊娠结局的危险因素,为临床进行针对性的管理、改善母婴结局提供依据。
1 对象与方法
1.1 研究对象
纳入2017年1月1日—2021年12月31日在上海交通大学医学院附属仁济医院孕20周前规范建卡、产检并分娩的单胎妊娠合并CKD患者。
1.2 研究方法
收录患者的临床资料,包括人口学特征[年龄、孕产次、孕20周前体质量指数(body mass index,BMI)]、初次建卡的血压、妊娠20周前血化验指标(包括血常规、尿常规、24 h尿蛋白、血脂、肝功能、肾功能、甲状腺功能等)、既往病史(肾病类型)、孕前及妊娠期的用药情况(激素、免疫抑制剂、抗凝药物等)、分娩信息及妊娠结局。
不良妊娠结局包括孕20周后胎儿丢失、新生儿产后42 d内死亡、孕妇发生子痫前期或子痫、AKI、早产、低出生体质量儿、小于孕龄儿、新生儿7 d内入住NICU。
(1)子痫前期
① CKD孕妇孕前尿蛋白阴性,孕20周后新出现的血压升高[收缩压≥140 mmHg和(或)舒张压≥90 mmHg,1 mmHg=0.133 kPa],伴新出现的蛋白尿或其他靶器官功能受损。② CKD孕妇孕前已有蛋白尿,孕20周后新出现的血压升高或靶器官功能受损。③ CKD孕妇孕前已有慢性高血压和蛋白尿,孕20周后新出现靶器官功能受损[5]。
(2)子痫
发生其他原因不能解释的在子痫前期基础上的抽搐[6]。
(3) AKI
CKD患者48 h内血肌酐升高≥0.3 mg/dL(26.5 μmol/L),或7 d内升高达基线值的1.5倍[7]。
(4)早产
妊娠达到28周但不足37周分娩[8]。
(5)早期早产
妊娠达到28周但不足34周分娩[8]。
(6)低出生体质量儿
新生儿出生体质量不足2 500 g[9]。
(7)小于孕龄儿
出生体质量低于相应胎龄体质量第10百分位的新生儿[10]。
根据有无不良妊娠结局将研究对象分为不良妊娠结局组(研究组)与良好妊娠结局组(对照组),分析2组资料的差异以及与不良妊娠结局的相关性。
1.3 统计学方法
应用SPSS 26.0软件进行统计学分析。连续型变量符合正态分布的以x±s表示,2组均数比较采用独立样本t检验;非正态分布的以M(Q1,Q3)表示,2组间比较用Mann-Whitney U检验。定性变量以n(%)表示,比较采用χ2检验或Fisher精确概率法。将单因素分析有统计学意义的指标纳入多因素回归分析。P<0.05为差异具有统计学意义。
2 结果
2.1 妊娠合并CKD患者的妊娠结局
本研究共收集了359例孕产妇的临床资料,排除双胎妊娠6例,研究共纳入353例单胎妊娠合并CKD患者,其中慢性肾炎201例(56.94%)、IgA肾病99例(28.05%)、狼疮肾炎39例(11.05%)、肾病综合征14例(3.97%)。根据结局分为不良妊娠结局(研究组)123人,良好妊娠结局(对照组)230人。对上述4类妊娠合并CKD患者的不良妊娠结局及其发生率进行分析,具体数据见表1。
表1 妊娠合并CKD患者的不良妊娠结局及其发生率
Tab 1
| Item | Type of nephritis | |||
|---|---|---|---|---|
| Chronic nephritis | IgA nephropathy | Lupus nephritis | Nephrotic syndrome | |
| Number of delivery/n(%) | 201 (56.94) | 99 (28.05) | 39 (11.05) | 14 (3.97) |
| Maternal outcome/n(%) | ||||
| PE | 43 (21.39) | 14 (14.14) | 11 (28.21) | 1 (7.14) |
| Severe PE | 24 (11.94) | 9 (9.09) | 9 (23.08) | 1 (7.14) |
| Acute kidney injury | 13 (6.50) | 10 (10.10) | 3 (7.69) | 3 (21.43) |
| Fetal outcome/n(%) | ||||
| Fetal loss after 20 weeks | 3 (1.49) | 3 (3.03) | 0 (0) | 1 (7.14) |
| Neonatal death | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Preterm birth | 28 (13.93) | 16 (16.16) | 22 (56.41) | 3 (21.43) |
| Preterm birth before 34weeks | 9 (4.48) | 7 (7.07) | 10 (25.64) | 3 (21.43) |
| LBWI | 18 (8.95) | 9 (9.09) | 17 (43.58) | 2 (14.29) |
| SGA | 16 (7.96) | 8 (8.08) | 8 (20.51) | 2 (14.29) |
| NICU | 19 (9.45) | 9 (9.09) | 11 (28.20) | 2 (14.29) |
2.2 2组临床特点比较
2组患者的年龄(P=0.723)、BMI(P=0.058)、孕次(P=0.268)、产次(P=0.630)、是否服用阿司匹林(P=0.653)差异均无统计学意义;研究组孕妇妊娠20周前收缩压、舒张压、平均动脉压均高于对照组(均P=0.000),是否有高血压病史的组间差异具有统计学意义(P=0.022);研究组中更多患者在孕20周前24 h尿蛋白≥0.3 g(56.91% vs 34.34%,P=0.000);更多孕妇在妊娠20周前服用免疫抑制剂(30.89% vs 14.35%,P=0.000);更多孕妇患有狼疮肾炎(19.51% vs 6.52%,P=0.000),而慢性肾炎、肾病综合征和IgA肾病的病例数在2组间的比例无统计学差异。具体数据见表2。
表2 2组妊娠20周前临床特点比较
Tab 2
| Item | Study group (n=123) | Control group (n=230) | P value |
|---|---|---|---|
| Age/year | 31.22±3.74 | 31.37±3.64 | 0.723 |
| BMI/(kg·m-2) | 22.74±3.57 | 21.92±2.89 | 0.058 |
| Pregnancy/n | 2 (1, 3) | 2 (1, 2) | 0.268 |
| Delivery/n | 0 | 0 | 0.630 |
| Chronic hypertension/n(%) | 20 (16.26) | 19 (8.26) | 0.022 |
| SBP/mmHg | 123 (115, 132) | 115 (108, 123) | 0.000 |
| DBP/mmHg | 79 (71, 86) | 71.5 (66, 80) | 0.000 |
| MAP/mmHg | 94 (86, 101) | 86 (80, 93) | 0.000 |
| Aspirin/n(%) | 109 (88.61) | 200 (86.96) | 0.653 |
| Immunosuppressant/n(%) | 38 (30.89) | 33 (14.35) | 0.000 |
| 24 h proteinuria≥0.3 g/n(%) | 70 (56.91) | 79 (34.35) | 0.000 |
| 24 h proteinuria≥2 g/n(%) | 57 (46.34) | 31 (13.48) | 0.000 |
| Types of nephritis/n(%) | |||
| Chronic nephritis | 68 (55.28) | 133 (57.83) | 0.646 |
| IgA nephropathy | 27 (21.95) | 72 (31.30) | 0.062 |
| Nephrotic syndrome | 4 (3.25) | 10 (4.35) | 0.615 |
| Lupus nephritis | 24 (19.51) | 15 (6.52) | 0.000 |
2.3 2组实验室指标分析
研究组与对照组的实验室指标比较见表3。2组孕妇妊娠20周前的白细胞计数(P=0.158)、血红蛋白水平(P=0.061)、血小板计数(P=0.990)、促甲状腺激素(P=0.092)差异均无统计学意义,但研究组妊娠20周前血肌酐和24 h尿蛋白水平明显高于对照组(均P=0.000)。
表3 2组妊娠20周前实验室指标比较
Tab 3
| Item | Study group (n=123) | Control group (n=230) | P value |
|---|---|---|---|
| WBC/(×109·L-1) | 9.57±2.62 | 9.19±2.29 | 0.158 |
| HB/(g·L-1) | 120.22±18.49 | 123.69±11.71 | 0.061 |
| PLT/(×109·L-1) | 237.97±66.47 | 238.05±54.92 | 0.990 |
| TSH/(mIU·mL-1) | 1.52 (0.71, 2.74) | 1.31 (0.53, 2.00) | 0.092 |
| Serum creatinine/(μmol·L-1) | 58.00 (44.00, 82.00) | 48.25 (42.77, 53.85) | 0.000 |
| Proteinuria/[mg·(24 h)-1] | 683 (326, 2 121) | 321 (177, 691) | 0.000 |
2.4 Logistic回归分析不良妊娠结局的独立危险因素
表4 单因素回归分析不良妊娠结局的影响因素
Tab 4
| Item | OR (95% CI) | P value |
|---|---|---|
| Chronic hypertension | 5.583 (2.124‒14.669) | 0.000 |
| Immunosuppressant | 2.669 (1.569‒4.540) | 0.000 |
| Serum creatinine >60 μmol/L | 5.136 (3.101‒8.507) | 0.000 |
| 24 h proteinuria | ||
| Proteinuria≥0.3 g | 2.656 (1.419‒4.971) | 0.002 |
| Proteinuria≥2 g | 8.033 (3.339‒19.331) | 0.000 |
| Types of nephritis | ||
| Lupus nephritis: chronic nephritis | 3.129 (1.541‒6.354) | 0.002 |
| IgA nephropathy: chronic nephritis | 0.733 (0.432‒1.246) | 0.252 |
| Nephrotic syndrome: chronic nephritis | 0.782 (0.237‒2.587) | 0.687 |
表5 多因素回归分析不良妊娠结局的独立危险因素
Tab 5
| Item | OR (95% CI) | P value |
|---|---|---|
| Chronic hypertension | 3.385 (1.115‒10.726) | 0.031 |
| Serum creatinine >60 μmol/L | 2.828 (1.439‒5.557) | 0.003 |
| 24 h proteinuria | ||
| Proteinuria≥0.3 g | 2.234 (1.122‒4.448) | 0.022 |
| Proteinuria≥2 g | 4.904 (1.808‒13.303) | 0.002 |
| Types of nephritis | ||
| Lupus nephritis: chronic nephritis | 4.917 (1.967‒12.290) | 0.001 |
| IgA nephropathy: chronic nephritis | 0.745 (0.375‒1.478) | 0.399 |
| Nephrotic syndrome: chronic nephritis | 0.764 (0.126‒4.624) | 0.769 |
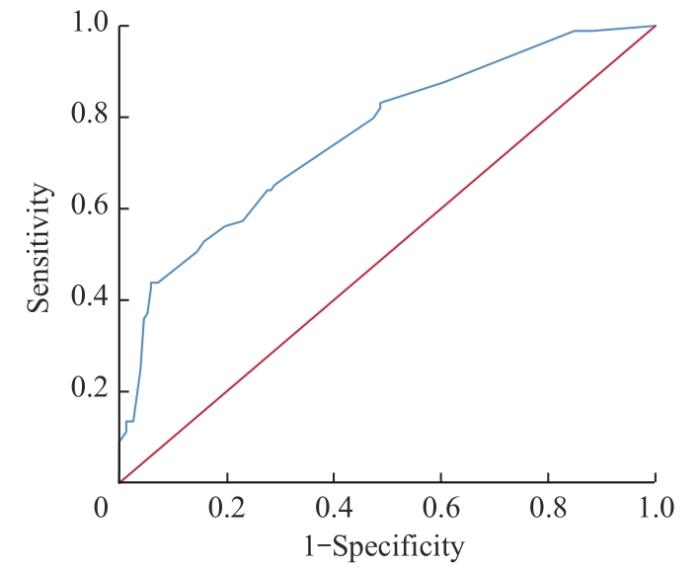
以发生不良妊娠结局为因变量,以上述多因素回归分析得到的独立危险因素为自变量,利用受试者操作特征曲线(receiver operator characteristic curve,ROC曲线)就联合指标对CKD患者并发不良妊娠结局的预测价值进行研究。如图1所示,联合指标预测不良妊娠结局ROC曲线下面积为0.759,敏感度为52.8%,特异度为84.2%。
图1
图1
联合指标对不良妊娠结局预测的ROC曲线
Fig 1
ROC curve of combined indicators for predicting adverse pregnancy outcomes
3 讨论
本研究中妊娠期最常见的CKD分类诊断依次为慢性肾炎、IgA肾病、狼疮肾炎以及肾病综合征,CKD患者妊娠20周前合并慢性高血压、血肌酐大于60 μmol/L、尿蛋白≥0.3 g/24 h、病理类型为狼疮肾炎是发生不良妊娠结局的独立危险因素;上述4个联合指标对于不良妊娠结局具有较高的临床预测价值。
本研究中多因素回归分析显示合并慢性高血压是CKD患者发生不良妊娠结局的独立危险因素,与既往研究结果基本一致。PICCOLI等[11]报道CKD1期患者中,合并高血压患者发生早产的风险升高3.42倍。IMBSCIATI等[12]在CKD3~5期妊娠女性的研究中发现,慢性高血压是孕34周前终止妊娠的最强预测因子。2017年我国《慢性肾脏病患者妊娠管理指南》[13]指出,CKD患者合并高血压对妊娠结局的影响较大,且血压控制的困难程度与发生不良妊娠结局的风险大小相关。高血压可能通过影响母体各脏器血液供应和胎盘血流灌注导致不良妊娠结局如早产、子痫前期、小于孕龄儿、新生儿入住NICU等的发生。临床上对合并高血压的CKD患者应积极降压治疗,控制血压的稳定以减少不良母婴结局的发生。
CKD患者常常伴有蛋白尿。PICCOLI等[11]的研究显示24 h蛋白尿大于1 g与不良妊娠结局相关。另一项研究[14]显示在CKD3a期患者中,蛋白尿小于1 g/24 h的患者产后6个月eGFR较早孕期无明显变化,而蛋白尿大于1 g/24 h,患者产后6个月eGFR较早孕期明显下降,且多因素回归分析显示24 h尿蛋白大于2 g是早产的独立危险因素。本研究采用了子痫前期和重度子痫前期中关于蛋白尿阳性的诊断标准,分别把CKD患者孕20周前24小时尿蛋白≥0.3 g和≥2 g进行不良妊娠结局的危险因素分析,结果发现,两者均是不良妊娠结局的独立危险因素,且当24 h尿蛋白≥2 g时,CKD患者发生不良妊娠结局的风险更高。本研究与既往研究结果基本一致,但本研究发现尿蛋白≥0.3 g/24 h已经是发生不良结局的危险因素,显示蛋白尿对不良结局的预测敏感性高。即便是轻度蛋白尿仍对妊娠结局有不良影响,临床医师也需加以警惕。蛋白持续通过肾脏漏出会诱导细胞凋亡,导致足细胞功能障碍,促进肾小管间质纤维化,加重肾脏损伤[15],引起低蛋白血症,最终导致孕妇肺水肿、胎儿生长受限、早产等的发生。
由于妊娠期肾脏功能的生理变化,GFR的计算方法不适用于孕期[14]。目前尚无有效的公式可以有效评估妊娠期肾小球滤过率,临床上较难估计孕期新发现的CKD患者的CKD分期,因此血肌酐仍然是妊娠合并CKD患者肾功能的评估标准[16]。正常妊娠时由于GFR增加,血肌酐在孕期降低。加拿大一项243 534例孕妇的横断面分析显示:孕前、孕16~32周、产后1周的血清肌酐的第95百分位值分别为78、59、84 μmol/L——建议孕中期血清肌酐≥60 μmol/L应考虑肾功能受损[17]。一项有关慢性高血压患者基线肾功能与不良妊娠结局关系的研究[18]表明,基线肌酐水平超过66.3 μmol/L与早发型重度子痫前期的发生有关。DVOŘÁK等[19]研究也指出孕期较高的血清肌酐水平及蛋白尿与早产和低出生体质量儿的发生相关。本研究参考了HAREL等[17]的建议,将孕中期血清肌酐≥60 μmol/L作为肾功能受损的评估标准,发现当血肌酐超过60 μmol/L时,不良妊娠结局的发生率明显增加,且血肌酐超过60 μmol/L是发生不良妊娠结局的独立危险因素。本研究中以妊娠20周前血肌酐超过60 μmol/L为界,预测不良妊娠结局的假阳性率仅为15.2%、假阴性率为52%;提示孕中期血肌酐超过60 μmol/L可作为临床筛查指标,可敏感地预测CKD患者发生不良妊娠结局。
国外一项研究纳入126例肾小球肾炎、37例狼疮肾炎和33例IgA肾病,另外纳入1 418例健康孕妇作为对照,结果显示狼疮肾炎患者与非狼疮肾炎患者妊娠风险无显著差异,而IgA肾病与先兆子痫的发生显著相关[20]。本研究中,研究组患者中狼疮肾炎患者占比显著高于对照组,差异具有统计学意义。与慢性肾炎患者比较,狼疮肾炎患者发生不良妊娠结局的风险最高,IgA肾病患者发生不良妊娠结局的风险最低。该结果与国外的研究结果不同,与我国2017年指南[13]提出的在肾病病因中,系统性疾病如狼疮肾炎和糖尿病肾病对妊娠结局的影响最为显著较为一致。这可能与狼疮肾炎患者易并发高血压、蛋白尿等,易引起多脏器功能损害有关。目前尚缺乏大规模狼疮肾炎与IgA肾病妊娠结局的比较研究,临床上需要进一步论证。
本研究的优点:纳入研究对象的临床和实验室检验信息均在孕20周之前,所发现的危险因素对于CKD患者发生不良妊娠结局有很好的预测价值。在各个临床指标中筛选出妊娠20周前合并慢性高血压、24 h尿蛋白≥0.3 g、血肌酐超过60 μmol/L、病理类型为狼疮肾炎是发生不良妊娠结局的独立危险因素;首次提出联合4个指标对于不良妊娠结局具有较高的临床预测价值。
本研究亦有不足之处:① 本研究为回顾性分析,纳入的研究对象均为产科建卡患者,未包括部分早孕因病情严重行流产手术患者,可能存在偏倚。② 患者产前肾功能资料缺失,不能准确评估患者孕前的CKD分期,未以CKD分期为研究变量。③ 未对CKD患者产后进行随访,未评估CKD患者妊娠后的远期肾功能损害情况。
综上,本研究发现CKD患者孕20周前合并慢性高血压、尿蛋白≥0.3 g/24 h、血肌酐超过60 μmol/L、病例类型为狼疮肾炎是发生不良妊娠结局的独立危险因素,联合4个指标对于不良妊娠结局具有较高的临床预测价值。临床工作中需要对以上情况的CKD孕妇加强关注。CKD患者需要在做好孕前咨询的前提下备孕,同时应加强孕期监测,做好血压、尿蛋白水平、血肌酐水平的管理,对有狼疮肾炎的孕妇要尤为关注,以获得更好的妊娠结局。
作者贡献声明
李玉参与了研究设计、数据收集整理及分析、论文撰写及修改,张羽负责论文的设计及修改。所有作者均阅读并同意了最终稿件的提交。
AUTHOR's CONTRIBUTIONS
LI Yu participated in the study design, data collection and analysis, and paper writing and revision. Zhang Yu participated in the design and revision of the paper. Both authors have read the last version of paper and consented for submission.
利益冲突声明
所有作者声明不存在利益冲突。
COMPETING INTERESTS
All authors disclose no relevant conflict of interests.
参考文献