弥漫性大B细胞淋巴瘤(diffuse large B-cell lymphoma,DLBCL)是一种常见的具有高度侵袭性的淋巴瘤,约占所有非霍奇金淋巴瘤病例的30%[1]。其常见的临床特征包括淋巴结肿大和淋巴结外器官受累等[2]。肾脏累及的DLBCL患者约占全部DLBCL患者的2%,中位发病年龄为55~65岁,5年生存率约为40%,在标准化学治疗(化疗)方案中添加利妥昔单克隆抗体(rituximab)可以使患者的5年生存率提高[3-4]。肾脏累及的DLBCL文献报道较少,发病机制尚不明确,增加了此类患者治疗的困难[3]。本研究回顾性分析149例肾脏累及DLBCL患者,分析其临床和病理特征、基因突变谱、治疗及预后情况等,旨在探究这类患者临床和预后特征,同时为相关的临床实践提供参考。
1 对象与方法
1.1 研究对象
纳入2005年7月—2021年11月于上海交通大学医学院附属瑞金医院诊断为DLBCL,且存在肾脏累及的患者共149例。纳入标准:① 均进行血常规、生化常规、心电图、骨髓穿刺、全身计算机断层扫描(computed tomography,CT)或正电子发射计算机断层扫描(positron emission tomography-CT,PET-CT)等检查。② 病理组织活检及免疫组织化学染色确诊,并根据2016年世界卫生组织(World Health Organization,WHO)淋巴瘤分类标准进行病理复核[5]。通过病理组织活检及免疫组织化学确诊患者为DLBCL,而肾脏是否累及主要依靠影像学检查(全身CT、PET-CT、增强CT等)判定。
患者一般信息包括性别、年龄、美国东部肿瘤协作组(Eastern Cooperative Oncology Group,ECOG)评分、Ann Arbor分期、根据淋巴瘤病理免疫组织化学分析评估的Hans分型、国际预后指数(international prognosis index,IPI)、血清乳酸脱氢酶(lactate dehydrogenase,LDH)、PET-CT检查报告、治疗方案、靶向测序等,并随访其疾病转归及生存情况。
1.2 治疗方案
149例患者中,共128例(85.9%)接受利妥昔单克隆抗体联合环磷酰胺、阿霉素、长春新碱及泼尼松(rituximab,cyclophosphamide,doxorubicin,vincristine,prednisone,R-CHOP)为基础的化疗方案4~6个周期。其余治疗方案包括环磷酰胺、阿霉素、长春新碱及泼尼松(cyclophosphamide,doxorubicin,vincristine,prednisone,CHOP)1例(0.7%),利妥昔单克隆抗体联合依托泊苷、地塞米松、长春新碱、环磷酰胺、多柔比星(dose-adjusted etoposide,dexamethasone,vincristine,cyclophosphamide,doxorubicin,rituximab,DA-EDOCH-R)4例(2.7%),布鲁顿酪氨酸激酶(Bruton′s tyrosine kinase,BTK)抑制剂联合来那度胺(lenalidomide)、利妥昔克隆抗体的治疗方案共13例(8.7%)。其余3例(2.0%)因基础条件差等原因未予抗肿瘤治疗,仅予对症支持治疗。
1.3 疗效评价及分期
治疗结束后进行评估,评估手段包括69例(46.3%)采用PET-CT,以及80例(53.6%)采用颈部、胸部、腹部、盆腔增强CT。采用2014年版卢加诺(Lugano)淋巴瘤疗效评价标准进行治疗效果评估[6],包括完全缓解(complete response,CR)、部分缓解(partial response,PR)、疾病稳定(stable disease,SD)、疾病进展(progressive disease,PD),客观缓解率(objective response rate,ORR)为CR和PR患者所占比例之和[6]。按照Ann Arbor分期标准进行临床分期,体能状态评分为ECOG评分,应用IPI进行患者危险分层[7]。
1.4 随访
采用门诊、电话及病历查阅方式进行随访,随访时间至2023年6月6日。总生存时间(overall survival,OS)是指从患者诊断之日起至因任何原因导致的死亡或随访终点的时间间隔;无进展生存时间(progression-free survival,PFS)是指从患者诊断之日起至第一次发现肿瘤进展或者患者死亡的时间间隔。
1.5 靶向测序鉴定基因突变
应用组织基因组DNA(genomic DNA,gDNA)提取试剂盒(Promega,Madison,Wisconsin,USA)提取gDNA。取1 μg DNA制备目标基因区域DNA文库。使用PCR引物扩增目的基因(54个淋巴瘤相关基因),包括ARID1A、ATM、B2M、BCL6、BTG1、BTG2、CARD11、CCND3、CD58、CD70、CD79A、CD79B、CIITA、CREBBP、DDX3X、DTX1、DUSP2、EBF1、EP300、EZH2、FAS、FBXW7、GNA13、HIST1H1C、HIST1H1E、IRF4、IRF8、KMT2C、KMT2D、LYN、MAPK7、MPEG1、MTOR、MYC、MYD88、NFKBIE、NOTCH1、NOTCH2、PIM1、PRDM1、PTPN6、SGK1、SOCS1、STAT3、STAT6、TBL1XR1、TET2、TMSB4X、TNFAIP3、TNFRSF14、TP53、TSC2、ZFP36L1、ZNF608 [8]。将目标区域DNA富集后,采用Novaseq(Illumina,San Diego,USA)测序平台进行测序。测序后原始数据利用CCDS(Consensus Coding Sequences)数据库、人基因组数据库hg19、dbSNP数据库(Single Nucleotide Polymorphism Database)、1000 genomes数据库、COSMIC(Catalogue of Somatic Mutations in Cancer)数据库、PolyPhen (Polumorphism Phenotyping)数据库、SIFT(Sorting Intolerant From Tolerant)数据库等进行生物信息学分析,确定致病基因突变。
1.6 统计学分析
所有统计学分析均使用R语言4.3.1版本进行。定性资料以n(%)表示。应用Kaplan-Meier方法计算OS和PFS并绘制生存曲线;Cox回归模型构建首先进行单因素分析,将单因素分析中P<0.05的影响因素纳入Cox回归模型进行多因素分析;Mann-Whitney U检验用于分析基因突变的差异。P<0.05表示差异具有统计学意义。
2 结果
2.1 临床特征分析
本研究分析了149例肾脏累及的DLBCL患者的临床特征,包括年龄、Ann Arbor分期、ECOG评分、血清LDH变化情况、肿瘤淋巴结外受累情况、IPI评分、病理类型、Hans分型、是否MYC基因表达和BCL2(B-cell lymphoma-2)/BCL6双表达及临床疗效(表1)。
表1 肾脏累及的DLBCL患者临床特征分析[n(%), N=149]
Tab 1
| Chatacteristic | n (%) |
|---|---|
| Age of diagnose | |
| ≤60/years | 62 (41.6) |
| >60/years | 87 (58.4) |
| Ann Arbor stage | |
| Ⅰ‒Ⅱ | 28 (18.8) |
| Ⅲ‒Ⅳ | 121 (81.2) |
| ECOG | |
| 0‒1 score | 122 (81.9) |
| ≥2 score | 27 (18.1) |
| Serum LDH | |
| Normal | 28 (18.8) |
| Elevated | 121 (81.2) |
| Extranodal involvement | |
| 0‒1 | 38 (25.5) |
| ≥2 | 111 (74.5) |
| IPI | |
| 0‒1 score | 18 (12.1) |
| 2‒5 score | 131 (87.9) |
| Pathological subtype | |
| DLBCL, NOS | 145 (97.3) |
| HGBCL with MYC and BCL2/BCL6 rearrangement | 4 (2.7) |
| Hans classification | |
| GCB | 39 (26.2) |
| non-GCB | 90 (60.4) |
| Unknown | 20 (13.4) |
| MYC and BCL2 double expressor | |
| Yes | 36 (24.2) |
| No | 113 (75.8) |
| Outcome① | |
| CR | 87 (60.4) |
| PR | 11 (7.6) |
| SD/PD | 46 (31.9) |
| Unknown | 5 (3.4) |
2.2 疗效评估与生存分析
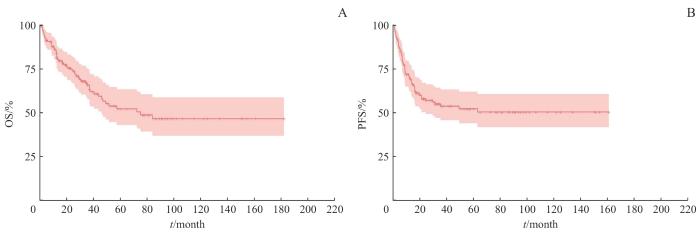
149例患者中共有144例患者(96.7%)可评估疗效,其中87例患者(60.4%)达到CR,11例患者(7.6%)达到PR,ORR为68.1%,46例患者(31.9%)病情稳定或疾病进展;另有5例患者(3.4%)疗效未知。Kaplan-Meier生存分析显示,肾脏累及的DLBCL患者中位随访时间为(55.8±8.3)月,5年OS率和5年PFS率分别为52.2%和50.4%(图1)。
图1
图1
肾脏累及的DLBCL患者的OS(A)和PFS(B)曲线
Note: A. OS curve in patients with kidney-involved DLBCL. B. PFS curve in patients with kidney-involved DLBCL.
Fig 1
The curves of OS (A) and PFS (B) in patients with kidney-involved DLBCL
2.3 预后因素分析
表2 肾脏累及的DLBCL患者预后的单因素分析
Tab 2
| Characteristic | OS | PFS | |||
|---|---|---|---|---|---|
| HR (95%CI) | P value | HR (95%CI) | P value | ||
| Age (>60 years) | 1.514 (0.914‒2.508) | 0.108 | 1.359 (0.821‒2.251) | 0.233 | |
| ECOG score (≥2 score) | 1.675 (0.939‒2.986) | 0.081 | 1.487 (0.809‒2.733) | 0.202 | |
| Ann Arbor (Ⅲ‒Ⅳ) | 1.119 (0.607‒2.060) | 0.719 | 1.257 (0.657‒2.046) | 0.489 | |
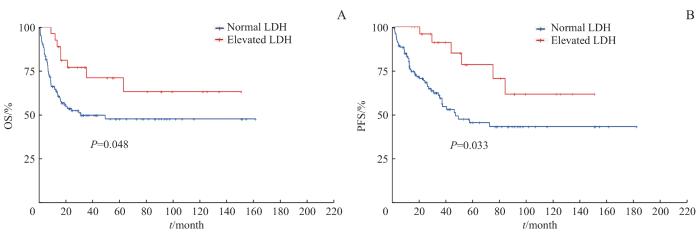
| Elevated serum LDH | 2.045 (1.018‒4.151) | 0.048 | 2.241 (1.067‒4.704) | 0.033 | |
| Extranodal involvement≥2 | 1.069 (0.621‒1.843) | 0.809 | 1.600 (0.871‒2.941) | 0.130 | |
| Hans (non-GCB) | 1.577 (0.969‒2.568) | 0.067 | 1.361 (0.834‒2.220) | 0.217 | |
| MYC and BCL2 double expressor | 1.210 (0.574‒2.552) | 0.616 | 1.073 (0.543‒2.121) | 0.839 | |
图2
图2
肾脏累及的DLBCL患者LDH水平与OS(A)和PFS(B)的关系
Note: A. Relationship between LDH level and OS in patients with kidney-involved DLBCL. B. Relationship between LDH level and PFS in patients with kidney-involved DLBCL.
Fig 2
The relationship between LDH level and OS (A) or PFS (B) in patients with kidney-involved DLBCL
2.4 基因突变分析
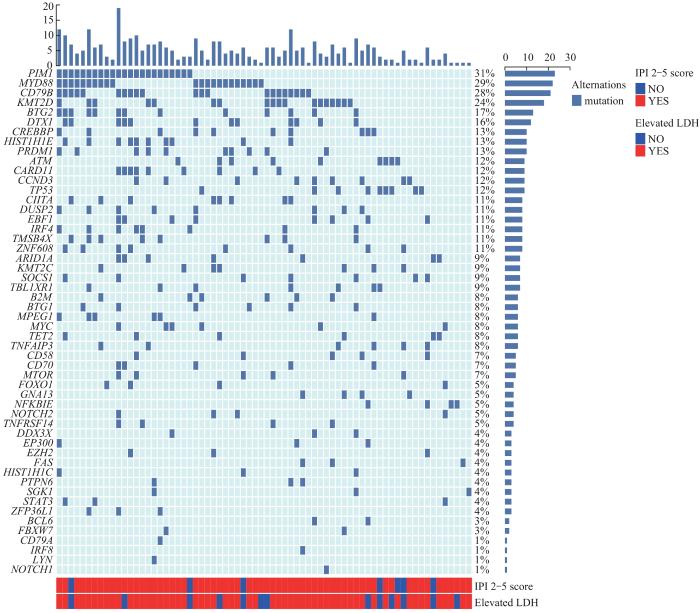
在149例患者中,有75例患者进行了靶向基因测序,共检测出52个基因的突变。其中,突变率大于20%的基因有PIM1(n=23,31%)、MYD88(n=22,
图3
图3
肾脏累及的DLBCL患者的基因突变图谱
Fig 3
Gene mutation profiles in patients with kidney-involved DLBCL
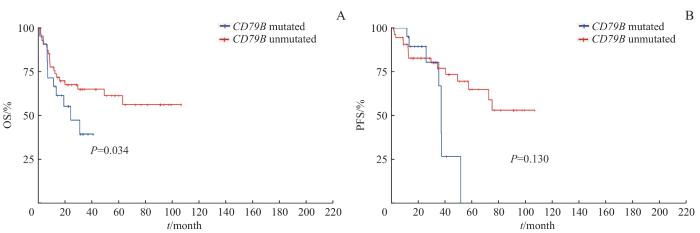
图4
图4
肾脏累及的DLBCL患者 CD79B 基因的突变状态与OS(A)和PFS(B)的关系
Note: A. Relationship between CD79B mutation and OS in patients with kidney-involved DLBCL. B. Relationship between CD79B mutation and PFS in patients with kidney-involved DLBCL.
Fig 4
The relationship between CD79B gene mutation and OS (A) or PFS (B) in patients with kidney DLBCL
3 讨论
本研究表明,血清LDH升高是影响肾脏累及的DLBCL患者OS和PFS的预后不良因素。这与既往文献报道相符,即血清LDH升高可能提示肿瘤的高侵袭性,并与多器官的结外累及相关[11] 。
二代测序可通过研究疾病分子突变来揭示疾病分子机制,并进一步进行分子分型。本研究应用了二代测序中的靶向测序技术,对75例患者肿瘤组织样本的54个特征性基因进行了分析。结果提示,B细胞受体介导通路相关基因PIM1、MYD88、CD79B等在肾脏累及的DLBCL患者中具有较高的突变率,且CD79B突变与患者OS率相关。既往文献报道提示MYD88和CD79B突变可能与DLBCL的多个结外受累有关,肾脏是这2个基因突变的高频受累器官[9,11]。根据WRIGHT等[12]报道的DLBCL分子分型,携带MYD88和CD79B突变的患者属于MCD亚型,该亚型具有更大的结外受累概率。BTK抑制剂,如伊布替尼,联合化疗方案R-CHOP在MCD亚型患者中的应用,相较于单纯R-CHOP治疗的患者,显示出更高的无事件生存(event free survival,EFS)率和OS率[13]。这可能表明BTK抑制剂联合R-CHOP方案能够改善肾脏累及的DLBCL患者的预后,并为复发难治的肾脏累及的DLBCL患者提供了新的治疗策略。此外,肾脏累及的DLBCL患者KMT2D突变率较高,然而该基因突变与肾脏累及机制的关系鲜有文献报道,有待进一步研究。
综上所述,DLBCL肾脏累及是一种较少见的结外受累模式;血清LDH升高是DLBCL肾脏累及的患者的预后不良因素之一;PIM1、MYD88、CD79B和KMT2D基因的高频突变可能为肾脏累及的DLBCL的治疗提供新的可能性;BTK抑制剂和化疗的联合使用可能提升肾脏累及的DLBCL患者的预后。
作者贡献声明
王博恩参与研究实施、数据采集、数据分析解释、文章起草;陈思远、施晴、张慕晨、易红梅、董磊参与数据采集;王黎、程澍参与文章审阅;许彭鹏参与试验设计、文章起草、文章审阅、统计分析、提供研究经费、研究及写作指导;赵维莅参与试验设计、文章审阅。
AUTHOR's CONTRIBUTIONS
WANG Boen carried out research implementation, collected and analyzed the data, and wrote the manuscript; CHEN Siyuan, SHI Qing, ZHANG Muchen, YI Hongmei, and DONG Lei collected the data; WANG Li and CHENG Shu reviewed the article; XU Pengpeng designed experiments, drafted articles, reviewed the article, analyzed data, and provided research funding and guidance; ZHAO Weili designed experiments and reviewed the article.
利益冲突声明
所有作者声明不存在利益冲突
COMPETING INTERESTS
All authors declare no relevant conflict of interests.
参考文献