目前关于GNRI对老年T2DM患者发生肺部感染预测价值的研究尚不够充分。因此,本研究在综合分析现有研究成果的基础上,深入探讨GNRI在预测老年T2DM患者发生肺部感染方面的应用价值,以期为临床医生和患者提供更加科学、有效的营养评估和肺部感染风险预测方法。
1 对象与方法
1.1 研究对象
1.2 资料收集
通过上海交通大学医学院附属同仁医院电子病历系统收集患者的临床和实验室资料。临床资料包括患者年龄、性别、身高、体质量和合并疾病(高血压、冠心病、慢性支气管炎),此外,还包括了糖尿病的病程和相关并发症的情况。实验室检查资料包括白细胞(white blood cell,WBC)、中性粒细胞比值(neutrophil ratio,NEUT)、淋巴细胞比值(lymphocyte ratio,LYMPH)、糖化血红蛋白(glycosylated hemoglobin,HbA1c)、空腹血糖(fasting blood glucose,FBG)、ALB、白介素-6(interleukin-6,IL-6)、C反应蛋白(C reactive protein,CRP)、降钙素原(procalcitonin,PCT)。
1.3 GNRI和体质量指数计算
参照既往研究[9]中的方法,计算GNRI和体质量指数(body mass index,BMI)。具体公式如下。
(1)GNRI=1.489×ALB水平+41.7×(m真实/m理想)。式中:ALB水平单位为g/L;m真实、m理想为体质量,单位为kg;m理想=22×h2;h为身高,单位为m。
(2)BMI=mB/h2。式中:BMI单位为kg/m2;mB为体质量,单位为kg;h为身高,单位为m。
1.4 肺部感染诊断
诊断标准[10]:发热超过38 ℃,新近出现咳嗽、咳痰或原有呼吸道疾病症状加重,外周血白细胞计数升高及中性粒细胞比值增加升高。结合肺部影像学表现及细菌学培养结果进一步明确。
1.5 统计学分析
采用SPSS25.0软件对数据进行统计分析。符合正态分布或近似正态分布的定量资料以x±s表示,组间比较采用独立样本t检验;严重偏态分布的定量资料以M(Q1,Q3)表示,组间比较采用秩合检验。定性资料描述为频数(百分率),组间比较采用χ2检验或Fisher精确概率检验。GNRI与CRP的相关性采用皮尔逊相关性分析,与PCT的相关性采用斯皮尔曼相关性分析。采用二元Logistic回归分析影响感染的独立危险因素。利用受试者操作特征(receiver operating characteristic,ROC)曲线描述数据的综合准确度以及区分度,并使用曲线下面积(area under the curve,AUC)来量化ROC曲线。所有的检验方向为双侧,P<0.05为差异具有统计学意义。
2 结果
2.1 感染组和非感染组临床资料比较
共纳入264例老年2型糖尿病患者,整体患者的平均年龄为(88.37±8.92)岁。其中,男性158例(59.8%),有154例(58.3%)患者发生了肺部感染。此外,整体平均GNRI值为94.75±8.10。详见表1。
表1 2组临床资料比较
Tab 1
| Item | Total sample (n=264) | Non-infected group (n=110) | Infected group (n=154) | t/Z/χ² value | P |
|---|---|---|---|---|---|
| Age/year | 88.37±8.92 | 91.17±4.50 | 86.36±10.62 | 5.023 | <0.001 |
| GNRI | 94.75±8.10 | 100.11±7.55 | 90.91±6.07 | 10.956 | <0.001 |
| Height/m | 1.67±0.08 | 1.66±0.09 | 1.67±0.08 | -1.627 | 0.105 |
| Body mass/kg | 63.92±10.77 | 67.13±10.58 | 61.62±10.34 | 4.221 | <0.001 |
| WBC/(×109·L-1) | 8.52±2.99 | 6.21±1.56 | 10.17±2.65 | -15.220 | <0.001 |
| NEUT/% | 68.40±11.80 | 61.04±7.49 | 73.65±11.52 | -10.770 | <0.001 |
| LYMPH/% | 20.58±9.27 | 25.64±6.96 | 16.96±9.03 | 8.819 | <0.001 |
| HbA1c/% | 7.67±0.86 | 7.51±0.76 | 7.78±0.92 | -2.540 | 0.012 |
| FBG/(mmol·L-1) | 8.18±1.43 | 7.55±1.22 | 8.63±1.40 | -6.682 | <0.001 |
| ALB/(g·L-1) | 34.35±3.50 | 36.07±3.04 | 33.11±3.28 | 7.445 | <0.001 |
| IL-6/(pg·ml-1) | 10.00 (5.86, 18.00) | 5.35 (3.45, 7.35) | 15.00 (10.00, 22.04) | -10.441 | <0.001 |
| CRP/(mg·L-1) | 10.21 (5.40, 33.25) | 5.60 (4.65, 7.00) | 26.03 (13.32, 50.10) | -10.935 | <0.001 |
| PCT/(ng·ml-1) | 0.10 (0.05, 0.23) | 0.06 (0.04, 0.15) | 0.15 (0.06, 0.33) | -4.731 | <0.001 |
| Diabetic duration/year | 4.00 (1.00, 9.00) | 4.00 (1.00, 9.00) | 3.50 (1.00, 8.00) | -0.710 | 0.480 |
| Gender/n(%) | 0.650 | 0.420 | |||
| Male | 158 (59.8) | 69 (62.7) | 89 (57.8) | ||
| Female | 106 (40.2) | 41 (37.3) | 65 (42.2) | ||
| CHD/n(%) | 20.533 | <0.001 | |||
| No | 48 (18.2) | 6 (5.5) | 42 (27.3) | ||
| Yes | 216 (81.8) | 104 (94.5) | 112 (72.7) | ||
| Hypertension/n(%) | 0.804 | 0.370 | |||
| No | 55 (20.83) | 20 (18.2) | 35 (22.7) | ||
| Yes | 209 (79.2) | 90 (81.8) | 119 (77.3) | ||
| Chronic bronchitis/n(%) | 35.418 | <0.001 | |||
| No | 130 (49.2) | 78 (70.9) | 52 (33.8) | ||
| Yes | 134 (50.8) | 32 (29.1) | 102 (66.2) | ||
| Diabetic nephropathy/n(%) | 0.700 | 0.403 | |||
| No | 212 (80.3) | 91 (82.7) | 121 (78.6) | ||
| Yes | 52 (19.7) | 19 (17.3) | 33 (21.4) | ||
| Peripheral vascular disease of diabetes/n(%) | 0.800 | 0.370 | |||
| No | 209 (79.2) | 90 (81.8) | 119 (77.3) | ||
| Yes | 55 (20.8) | 20 (18.2) | 35 (22.7) | ||
| Diabetic foot/n(%) | 0.860 | 0.355 | |||
| No | 245 (92.8) | 104 (94.6) | 141 (91.6) | ||
| Yes | 19 (7.2) | 6 (5.4) | 13 (8.4) |
为了探讨发生肺部感染的可能影响因素,对感染组和非感染组患者的临床资料进行了对比,结果如表1所示。发生肺部感染组患者的体质量显著低于感染组[(61.62±10.34)kg vs(67.13±10.58)kg,P<0.001]。感染组患者合并慢性支气管炎的比例(66.2%)高于非感染组(29.1%),差异具有统计学意义(P<0.001)。此外,发生肺部感染的患者其WBC、NEUT、HbA1c、FBG、IL-6、CRP、PCT水平均显著高于非感染组患者,但是GNRI、ALB和LYMPH显著低于非感染组(均P<0.05)。
2.2 GNRI水平与CRP、PCT的相关性
相关性分析结果显示,GNRI与CRP、PCT水平均呈负相关(r=-0.451,-0.347,均P<0.001)。
2.3 多因素Logistic回归分析
表2 影响老年T2DM患者发生肺部感染的因素分析
Tab 2
| Item | OR | 95% CI | P value |
|---|---|---|---|
| Age | 0.843 | 0.743‒0.957 | 0.008 |
| GNRI | 0.798 | 0.712‒0.894 | <0.001 |
| LYMPH | 0.928 | 0.852‒1.010 | 0.084 |
| HbA1c | 1.368 | 0.605‒3.091 | 0.451 |
| FBG | 1.232 | 0.697‒2.179 | 0.473 |
| IL-6 | 1.176 | 1.032‒1.340 | 0.015 |
| CRP | 1.374 | 1.182‒1.597 | <0.001 |
| PCT | 3.232 | 0.252‒41.508 | 0.368 |
| CHD | 1.280 | 0.098‒16.709 | 0.850 |
| Chronic bronchitis | 4.938 | 1.126‒21.652 | 0.034 |
此外,GNRI每升高1个单位,则发生肺部感染的风险下降20.2%(OR=0.798,95%CI 0.712~0.894,P<0.001),提示GNRI是感染的独立保护性因素,GNRI的升高可能有助于预防肺部感染的发生。
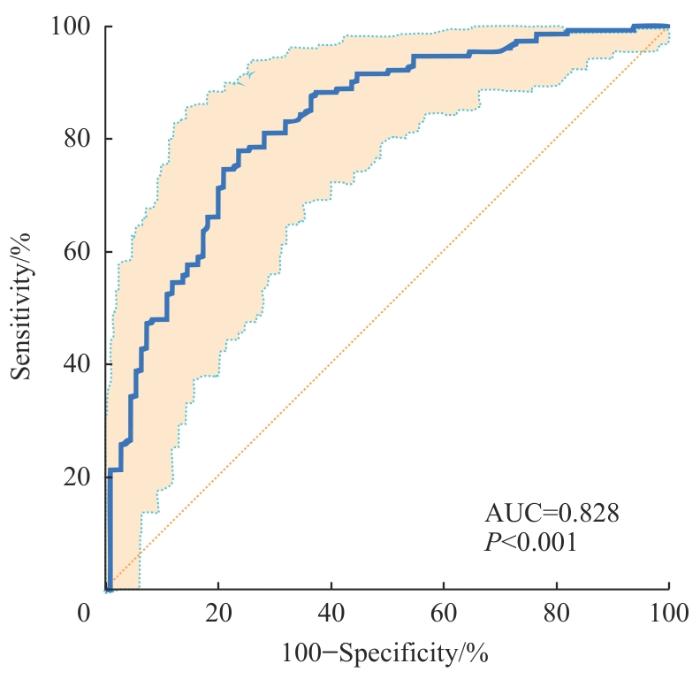
2.4 ROC曲线分析
表3 GNRI对肺部感染预测价值的相关ROC参数
Tab 3
| Parameter | Value | 95%CI |
|---|---|---|
| AUC | 0.828 | 0.777‒0.872 |
| SE | 0.026 | N/A |
| Yuden-index | 0.543 | 0.420‒0.626 |
| Cut-off | 94.727 | 93.870‒99.820 |
| Sensitivity/% | 77.9 | 70.5‒84.2 |
| Specificity/% | 76.6 | 67.3‒83.9 |
| PPV/% | 82.2 | 76.6‒86.7 |
| NPV/% | 71.2 | 64.3‒77.2 |
图1
2.5 低GNRI组和高GNRI组临床资料对比结果
由以上数据可知,GNRI在预测患者是否肺部感染时有着较高的预测价值。基于此将GNRI分为2组,并进一步比较低GNRI组(≤94.727)和高GNRI组(>94.727)间的临床资料以及炎性指标的差异,结果如表4所示。高GNRI组的体质量、ALB和LYMPH均显著高于低GNRI组(均P<0.05)。但是高GNRI组的WBC、NEUT、FBG、IL-6、CRP、PCT均低于低GNRI组,差异有统计学意义(均P<0.05)。
表4 低GNRI组和高GNRI组临床资料对比结果
Tab4
| Item | Total sample (n=264) | Low-GNRI group (n=145) | High-GNRI group (n=119) | t/Z/χ² value | P value |
|---|---|---|---|---|---|
| Age/year | 88.37±8.92 | 88.26±9.06 | 88.50±8.79 | -0.210 | 0.833 |
| Height/m | 1.66±0.08 | 1.66±0.08 | 1.67±0.09 | -0.730 | 0.468 |
| Body mass/kg | 63.92±10.77 | 58.20±8.41 | 70.88±9.11 | -11.740 | <0.001 |
| WBC/(×109·L-1) | 8.52±2.99 | 9.43±2.92 | 7.41±2.69 | 5.820 | <0.001 |
| NEUT/% | 68.40±11.80 | 71.46±12.05 | 64.66±10.37 | 4.930 | <0.001 |
| LYMPH/% | 20.58±9.27 | 18.68±9.45 | 22.89±8.52 | -3.760 | <0.001 |
| HbA1c/% | 7.67±0.86 | 7.61±0.87 | 7.73±0.86 | -1.050 | 0.293 |
| FBG/(mmol·L-1) | 8.18±1.42 | 8.36±1.33 | 7.96±1.51 | 2.320 | 0.021 |
| ALB/(g·L-1) | 34.35±3.50 | 32.77±3.04 | 36.27±3.03 | -9.330 | <0.001 |
| IL-6/(pg·ml-1) | 10.00 (5.86, 18.00) | 12.80 (8.12, 20.20) | 7.00 (4.23, 12.69) | -5.970 | <0.001 |
| CRP/(mg·L-1) | 10.21 (5.40, 33.25) | 24.00 (9.67, 47.24) | 6.30 (5.20, 9.34) | -7.120 | <0.001 |
| PCT/(ng·ml-1) | 0.10 (0.05, 0.23) | 0.13 (0.06, 0.32) | 0.08 (0.05, 0.16) | -3.770 | <0.001 |
| Diabetic duration/year | 4.00 (1.00, 9.00) | 4.00 (1.00, 8.00) | 4.00 (1.00, 9.00) | -0.070 | 0.944 |
| Gender/n(%) | 2.930 | 0.087 | |||
| Male | 158 (59.9) | 80 (55.2) | 78 (65.5) | ||
| Female | 106 (40.1) | 65 (44.8) | 41 (34.5) | ||
| CHD/n(%) | 3.270 | 0.071 | |||
| No | 48 (18.2) | 32 (22.1) | 16 (13.5) | ||
| Yes | 216 (81.8) | 113 (77.9) | 103 (86.5) | ||
| Hypertension/n(%) | 0.450 | 0.501 | |||
| No | 55 (20.8) | 28 (19.3) | 27 (22.7) | ||
| Yes | 209 (79.2) | 117 (80.7) | 92 (77.3) | ||
| Chronic bronchitis/n(%) | 0.350 | 0.552 | |||
| No | 134 (50.8) | 76 (52.4) | 58 (48.7) | ||
| Yes | 130 (49.2) | 69 (47.6) | 61 (51.3) | ||
| Diabetic nephropathy/n(%) | 0.700 | 0.403 | |||
| No | 212 (80.3) | 99 (68.3) | 113 (95.0) | ||
| Yes | 52 (19.7) | 46 (31.7) | 6 (5.0) | ||
| Peripheral vascular disease of diabetes/n(%) | 0.800 | 0.37 | |||
| No | 209 (79.2) | 113 (77.9) | 96 (80.7) | ||
| Yes | 55 (20.8) | 32 (22.1) | 23 (19.3) | ||
| Diabetic foot/n(%) | 0.860 | 0.355 | |||
| No | 245 (92.8) | 131 (90.3) | 114 (95.8) | ||
| Yes | 19 (7.2) | 14 (9.7) | 5 (4.2) |
3 讨论
既往有研究[13]表明,低白蛋白血症和营养不良会增加肺部感染发生风险,但是低白蛋白血症指标相对单一,它可能与炎症或水合状态的关系更大,营养不良的评估也受多种因素的限制。目前临床多用量表、主观全面评定量表进行营养评估,但容易受主观因素影响[14]。GNRI综合考虑BMI和ALB水平,是一种客观、简便的筛查方法,可用于评估老年人的营养状况[9]。有大量证据[15]表明,GNRI与其他营养评估指标之间存在一定的相关性,可以更好地预测短期和长期临床结果。同时,姜逍瑶等[16]学者研究发现GNRI对老年缺血性卒中相关性肺炎有较好的预测价值。GNRI目前被当作是心血管疾病、慢性肾脏疾病或癌症等慢性疾病患者的预后指标[17]。张家丽团队[18]研究了GNRI在老年医院获得性肺炎患者中预后评估的价值,并构建了一个预测老年医院获得性肺炎预后的列图。可见,GNRI可以更好地评估T2DM营养不良与肺部感染风险之间关系。
本研究绘制的ROC曲线显示,在GNRI预测是否感染时的AUC为0.828,敏感度为77.9%,特异度为76.6%,最佳截断值为94.727,提示GNRI对T2DM患者是否发生肺部感染有着较高的预测能力。本研究进一步根据GNRI数值高低对人群进行分组,结果发现GNRI的表达和炎症相关指标IL-6、CRP、PCT呈负相关,提示营养状况差的老年T2DM患者可增加肺部感染发生率。所以本研究结果表明,GNRI可以作为一种简单有效的工具,及早识别老年T2DM患者发生肺部感染。在临床实践中对营养相关风险进行筛查,可以帮助临床医生早期发现有肺部感染风险的患者,并及时为这些患者提供营养支持。
综上所述,本研究发现,GNRI的升高在老年T2DM患者中与肺部感染风险的降低具有关联,表明它可能是一个保护性因素。尽管本研究具有一定的局限性,主要体现在样本量相对较小,这限制了结果的普遍适用性,未来可通过更大规模的前瞻性研究,进一步验证这一发现。此外,本研究的优势在于填补了现有研究中关于T2DM营养不良与肺部感染风险关系研究的空白。鉴于此,GNRI有潜力发展成为预测老年T2DM患者肺部感染风险的有力临床工具,为临床决策提供支持。
作者贡献声明
连明珠、方姝予参与研究设计、论文的写作和修改;张常晓、盛凯参与数据整理和论文修改;郭梦参与数据收集和整理。所有作者均阅读并同意了最终稿件的提交。
AUTHOR's CONTRIBUTIONS
LIAN Mingzhu and FANG Shuyu contributed to the research design and the drafting and revision of the manuscript. ZHANG Changxiao and SHENG Kai participated in data organization and assisted with manuscript revision. GUO Meng was responsible for data collection and collation. All authors have reviewed and approved the final manuscript for submission.
利益冲突声明
所有作者声明不存在利益冲突。
COMPETING INTERESTS
All authors disclose no relevant conflict of interests.
参考文献