在上颌后牙区进行种植术时,常会出现牙槽骨窦嵴距不足的情况,经外侧壁入路的上颌窦底提升术已经成为针对窦嵴距过小而无法进行常规种植患者进行垂直骨增量的临床常用手段。在经外侧壁入路的上颌窦底提升术中,术中出血为常见的并发症,而引起大量出血的原因在于上颌窦动脉(maxillary sinus artery,MSA)的破损。MSA走形于上颌窦底提升术开窗区域附近,该动脉直径、走形位置等存在解剖变异。据统计,在经外侧壁入路的上颌窦底提升术中,由于MSA的血管解剖特性,骨内动脉损伤和出血的发生率可达20%[1]。现有研究[2-3]表明:MSA的走形类型、血管直径、血管至上颌窦底壁的距离为影响上颌窦底提升术的术中出血的重要因素。
本研究通过锥形术计算机断层扫描(cone-beam CT,CBCT)对大样本量人群的MSA进行观测,获取高清晰度及分辨率的MSA图像,采用流行病学方法对该人群MSA的解剖特点进行数据统计,推断可能影响MSA解剖变异的因素及分析不同解剖结构之间是否存在相互影响,以期为指导经外侧壁入路的上颌窦底提升术减少出血风险提供参考依据。
1 对象与方法
1.1 研究对象
选择2020年1月至2022年2月于上海交通大学医学院附属瑞金医院口腔科就诊,因行种植术而拍摄CBCT的患者1 021例作为研究对象。男性494例,女性527例。年龄18~88岁,平均年龄(47.9±5.6)岁。
纳入标准:①上颌窦无炎症、肿瘤、外伤、手术史及其他病变。②上颌窦周围无种植体及金属修复体。③上颌窦气化、形态、密度正常,图像清晰,无明显畸形。排除标准:①患者未满18周岁。②图像扫描范围不全。
1.2 材料与方法
1.2.1 仪器设备及测量软件
通过CBCT扫描仪(Accuitomo 170,森田,日本)进行图像采集,并由其自带软件进行观测及分析。扫描参数:电压220 V,输入功率2 kVA,频率50 Hz,采集图像时间15 s。扫描图像层厚 0.25 mm。
1.2.2 CBCT拍摄标准
头颅固定,眶耳平面平行于地面,后牙处于牙尖交错位,颌平面和正中矢状面与光标重叠。扫描范围:眶下缘至下颌骨下缘。
基准平面确定,在骨窗下调整矢状面视图,使前鼻棘至硬腭后缘连线与水平观测线平行,切换至水平面视图显露患者硬腭切牙孔及腭中线,调整冠状面视图使垂直观测线平分切牙孔并与腭中线重叠。
1.2.3 影像测量内容
(1)上颌窦侧壁厚度(lateral wall thickness,LWF):参照MONJE等[4]的方法,测量冠状位上第二前磨牙(the second premolar,P2)、第一磨牙(the first molar,M1)、第二磨牙(the second molar,M2)牙位的上颌窦底最低点上方5 mm处上颌窦侧壁厚度。
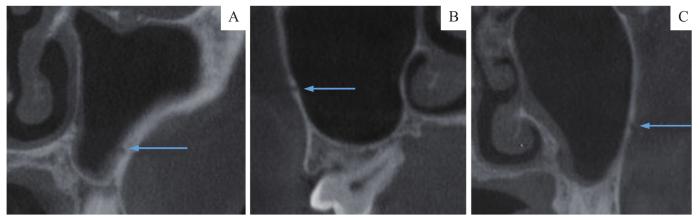
(2)MSA走形类型:按照走形位置与上颌窦侧壁的关系,对MSA走形(图1)分类为窦内型(位于上颌窦黏膜下方)、骨内型(完全位于上颌窦侧壁骨壁内)、表浅型(位于上颌窦侧壁骨膜下方)。
图1
图1
MSA走形类型
Note:A. Intrasinus type. B. Intraosseous type. C. Superficial type.
Fig 1
Shape type of MSA
(3)MSA骨孔直径(diameter of MSA,DMSA):参照YANG等[5]的方法,测量P2、M1、M2冠状位的上颌窦外侧壁血管骨孔顶壁至底壁的距离。
(4)MSA底壁至上颌窦底距离(distance between the lower margin of the vessel and the sinus floor,DVSF):参照YANG等[5]的方法,测量P2、M1、M2冠状位的MSA骨孔底壁与上颌窦底最低点的距离。
(5)M1牙位上颌窦宽度:测量M1冠状位的上颌窦底最低点上方5 mm处上颌窦宽度。
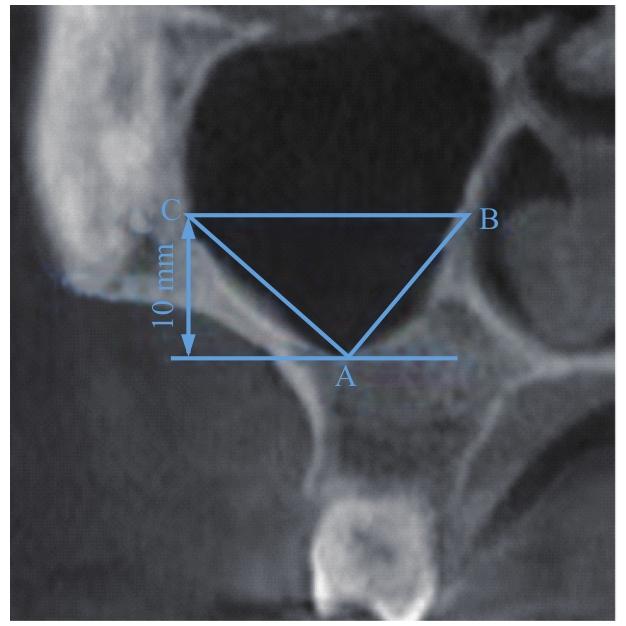
图2
图2
M1牙位上颌窦角度测量方法
Note: Point A—The bottom of maxillary sinus in M1 tooth position; Point B—The intersection point of the parallel line and the medial wall of maxillary sinus; Point C—The intersection point of the parallel line and the lateral wall of maxillary sinus.
Fig 2
Measurement method of maxillary sinus angle in M1 tooth position
(7)MSA走形位置变异:观测已检出的MSA与上颌窦底的关系,分析动脉走形于上颌窦底壁或上颌窦底根方牙槽骨内有无变异。
所有测量数据均由同一具影像学检查资质专业人员进行3次测量,以其平均值作为最终数据。
1.3 统计学方法
采用SPSS 26.0软件进行分析处理。定量资料以x±s表示。2组间数据比较采用独立样本t检验,根据组间方差是否齐选择方差齐时P值结果或方差不齐经SPSS软件自动校正后P值结果;多组间数据比较采用单因素方差LSD法分析。定量资料以n(%)表示,各组间率的比较采用χ2检验。相关性分析采用Pearson相关性分析。P<0.05时,表示差异具有统计学意义。
2 结果
2.1 MSA走形位置变异
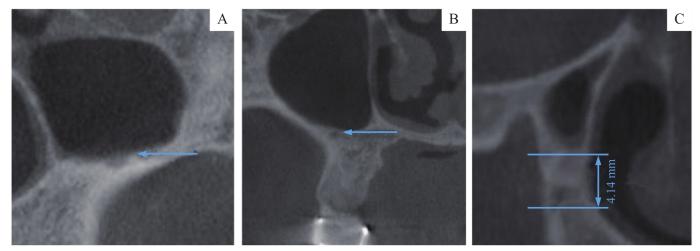
图3
图3
MSA走形位置变异
Note:A.The MSA was located at the bottom of maxillary sinus. B. The MSA was located in the root apical of molars. C. The MSA was located in the alveolar bone 4.14 mm from maxillary sinus floor.
Fig 3
Variability of the MSA position
2.2 MSA走形类型
对患者双侧上颌窦进行CBCT观测,共检出1 124侧上颌窦的MSA。走形类型最常见的为骨内型(占60.4%),其次为窦内型(占36.5%),表浅型最少(仅占3.1%)。不同性别患者中检出的各MSA走形类型的差异均无统计学意义(P>0.05)。比较不同年龄段患者中各个动脉走形检出率的差异,发现中年组(41~60岁)骨内型检出率较青年组(18~40岁)和老年组(>60岁)略高(P=0.005)。结果见表1。
表1 不同性别及不同年龄段MSA走形类型 [n(%)]
Tab 1
| Item | Gender | Age | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Male (n=544) | Female (n=580) | χ2 value | P value | Youthful (n=379) | Middle-aged (n=387) | Aged (n=358) | χ2 value | P value | |
| Intrasinus type | 198 (36.4) | 212 (36.6) | 0.003 | 0.957 | 138 (36.4) | 129 (33.3) | 143 (39.9) | 1.388 | 0.500 |
| Intraosseous type | 324 (60.0) | 355 (61.2) | 0.319 | 0.572 | 232 (61.2) | 244 (63.0) | 203 (56.7) | 10.471 | 0.005 |
| Superficial type | 22 (4.0) | 13 (2.2) | 3.024 | 0.082 | 9 (2.4) | 14 (3.6) | 12 (3.4) | 1.461 | 0.482 |
2.3 DMSA
利用CBCT观测患者双侧MSA,部分上颌窦中未能检出。在双侧上颌窦P2、M1、M2牙位检测到MSA的数量分别为489、479、963个,总计1 931个。DMSA>3 mm者12个,其中测得最大DMSA为4.19 mm。M1牙位测得的DMSA最大[(1.42±0.44)mm],其次为M2牙位[(1.27±0.41)mm],P2牙位DMSA最小[(1.26±0.42)mm]。男性在不同牙位的DMSA均大于女性组,差异有统计学意义(P<0.05),不同年龄患者之间DMSA的差异无统计学意义(P>0.05)。结果见表2。
表2 不同性别及年龄段在不同牙位的上颌窦DMSA (mm)
Tab 2
| Tooth position | Gender | Age | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | t value | P value | Youthful | Middle-aged | Aged | F value | P value | |
| P2 (n=489) | 1.40±0.45 | 1.09±0.30 | 8.429 | 0.000 | 1.22±0.40 | 1.28±0.46 | 1.29±0.40 | 1.077 | 0.311 |
| M1 (n=479) | 1.52±0.45 | 1.25±0.37 | 6.997 | 0.010 | 1.29±0.39 | 1.44±0.40 | 1.51±0.49 | 1.142 | 0.163 |
| M2 (n=963) | 1.37±0.44 | 1.15±0.33 | 8.703 | 0.000 | 1.19±0.32 | 1.28±0.45 | 1.33±0.42 | 0.964 | 0.612 |
P2、M1、M2牙位2 mm≥DMSA>1 mm的MSA分别占64.8%、76.6%、64.8%。当DMSA>2 mm时,出血不能靠血管收缩自行止住[7],需要进行即使止血。而当DMSA≤1 mm时,即使不慎术中出血也可自行止血,对手术操作要求较低。对不同牙位DMSA>2 mm者数量占比进行比较,发现各牙位间差异无统计学意义(P>0.05)。对不同牙位DMSA≤1 mm者的占比进行比较,结果显示:M1牙位DMSA≤1 mm者的占比均低于P2、M2牙位(P=0.000);进而两两比较发现,M1与P2之间、M1与M2之间,差异有统计学意义(均P=0.000),P2与M2之间差异无统计学意义(P>0.05)。结果见表3。
表3 上颌窦DMSA>2 mm及≤1 mm者在不同牙位的分布情况[n(%)]
Tab 3
| Item | P2 (n=489) | M1 (n=479) | M2 (n=963) | χ2 value | P value |
|---|---|---|---|---|---|
| DAAA>2 mm | 26 (5.3) | 44 (9.2) | 64 (6.7) | 5.865 | 0.053 |
| DAAA≤1 mm | 146 (29.9) | 68 (14.2) | 274 (28.5) | 41.716 | 0.000 |
2.4 DVSF
M2、M1、P2牙位的DVSF逐渐降低,分别为(8.44±3.80)mm、(6.93±3.69)mm、(5.57±3.88)mm。男性在P2、M2牙位的DVSF均大于女性(P<0.05),在M1牙位2组间差异无统计学意义(P>0.05)。不同年龄患者之间DVSF的差异无统计学意义(P>0.05)。结果见表4。
表4 不同性别及年龄患者在不同牙位的DVSF (mm)
Tab 4
| Tooth position | Gender | Age | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | t value | P value | Youthful | Middle-aged | Aged | F value | P value | |
| P2 (n=489) | 5.82±4.12 | 5.30±3.51 | 1.515 | 0.024 | 5.97±4.00 | 5.71±3.94 | 5.15±3.67 | 1.077 | 0.311 |
| M1 (n=479) | 7.15±3.85 | 6.54±3.40 | 1.765 | 0.059 | 6.96±3.77 | 7.15±3.49 | 6.62±3.82 | 1.036 | 0.420 |
| M2 (n=963) | 9.01±3.84 | 7.79±3.54 | 5.085 | 0.017 | 8.49±3.89 | 8.67±3.61 | 8.08±3.74 | 0.972 | 0.619 |
当DVSF>9 mm或<2 mm时出血风险相对较小[8]。为进一步了解DVSF对出血风险的影响,对不同牙位9 mm≥DVSF≥2 mm的MSA占比进行统计分析。P2、M1、M2牙位9 mm≥DVSF≥2 mm的MSA数量(占比)分别为311(63.6%)、316(66.0%)、534(55.5%),差异有统计学意义(P=0.000)。进一步两两比较,发现M2牙位9 mm≥DVSF≥2 mm者占比明显小于P2、M1牙位(P=0.003,P=0.000),P2与M1牙位比较差异无统计学意义(P>0.05)。
2.5 LWT与DMSA及DVSF的相关性
在P2、M1、M2牙位分别测量了422、434、949侧上颌窦的LWT。P2、M1、M2牙位LWT分别为(2.47±1.06)mm、(2.72±1.57)mm、(1.64±0.88)mm。
将不同牙位的LWT与DMSA、DVSF分别进行Pearson相关性分析,结果显示:LWT与DMSA在P2、M1牙位呈弱相关(r=0.2,P=0.000;r=0.2,P=0.000);LWT与DVSF在M1牙位呈弱负相关(r=-0.3,P=0.000)。结果见表5。
表5 不同牙位LWT与上颌窦DMSA及DVSF相关性
Tab 5
| Tooth position | DMSA | DVSF | |||
|---|---|---|---|---|---|
| r | P value | r | P value | ||
| P2 | 0.2 | 0.000 | -0.1 | 0.057 | |
| M1 | 0.2 | 0.000 | -0.3 | 0.000 | |
| M2 | 0.0 | 0.095 | -0.1 | 0.066 | |
2.6 M1牙位上颌窦宽度与DMSA及DVSF的相关性
共纳入位于M1牙位479侧上颌窦进行描述统计,其上颌窦宽度为(14.44±3.15)mm。Pearson相关性分析结果显示,M1牙位上颌窦宽度与DMSA和DVSF均呈弱负相关(r=-0.1,P=0.001;r=-0.1,P=0.006)。
2.7 M1牙位上颌窦角度与DMSA及DVSF相关性
共纳入位于M1牙位的479侧上颌窦进行描述统计,其上颌窦角度为83.72°±12.94°。Pearson相关性分析,M1牙位上颌窦角度与DMSA呈弱负相关(r=-0.2,P=0.001),与DVSF不具有相关性(P>0.05)。
3 讨论
3.1 MSA走形位置变异及走形类型分析
本研究发现MSA走形位置存在变异,多数MSA走形位于上颌窦侧壁,紧贴上颌窦底区域。因此在该区域进行上颌窦外提升术时,分离窦底黏膜需要保证黏膜完整性,必要时可增大骨窗直径以保证术野清晰。此外,MSA走形可位于上颌窦底根方牙槽骨及牙齿根尖区域。如若该侧患牙缺失,种植时应注意植体方向,勿偏颊侧损伤动脉;如若牙槽嵴垂直骨量不足需要上颌窦提升,在进行上颌窦内提升术时需要更加小心。
3.2 DMSA对出血风险的提示
2 mm≥DMSA>1 mm的MSA占比在22.1%~64.9%不等[8],本研究结果与其相近。既往研究[7]认为,血管直径<1 mm出血风险最小,因为小动脉(<2.0 mm)出血时,反应性血管收缩可降低血流量,出血会逐渐停止;当血管直径>2 mm时,出血的风险较高,血管收缩不足以自行止血。据统计,1 mm≥DMSA>0.5 mm时术中出血概率达10%,而当2 mm≥DMSA>1 mm时出血概率约为57%[10]。因此,本研究对P2、M1、M2牙位DMSA>2 mm者占比进行了统计,发现各组间差异无统计学意义,认为上颌窦外提升术时出现较大出血的风险与牙位无关。而对P2、M1、M2牙位DMSA≤1 mm者占比统计发现,在M1牙位的DMSA较其他牙位更大,且≤1 mm者占比更少,提示在M1牙位进行上颌窦外提升术时出血风险较大。既往研究[11]认为当血管直径>3 mm时应避让或进行结扎。若开窗区域血管直径>3 mm,且动脉走形于上颌窦侧壁骨膜下,则应视为上颌窦提升术的禁忌[12]。本研究中,DMSA>3 mm者较少(12例),但该人群行上颌窦提升术时损伤动脉、无法自行止血的概率较大。总之,上颌窦提升术前必须进DMSA的观测,避免术中发生医源性损伤,造成大出血。此外,本研究发现不同牙位男性DMSA均大于女性,提示男性患者出血概率更大[13]。有研究[14]表明DMSA或与年龄相关。本研究未发现不同年龄患者之间DMSA的差异,可能由于不同研究中测量手段差异、人种差异、年龄范围划分不同等原因导致。
3.3 DVSF对出血风险的提示
DANESH-SANI等[15]对860例患者进行CBCT的回顾性研究发现,MSA的平均DVSF为8.16 mm。本研究统计得出不同牙位(P2、M1、M2)处DVSF略低于文献数值,但与VALENTE[16]报道的5.8~10.4 mm数值相近。目前测量DVSF的文献较少,是否由于人种差异导致数值不一致还需进一步研究。本研究发现,由P2牙位向M2牙位,DVSF逐渐增大,该结论与WATANABE等[17]的结果一致。李濠吉等[3]研究了DVSF与出血风险的关系,发现当DVSF<7 mm时,动脉有26.4%的损伤风险,DVSF>9 mm或<2 mm时出血风险相对较小。因此,本研究对不同牙位9 mm≥DVSF≥2 mm者的占比进行统计比较,得出在P2、M1牙位该占比均高于M2牙位,提示在P2、M1牙位手术出血风险更高。既往大多研究测量MSA骨孔的最低点至牙槽嵴顶的距离,然而,牙槽嵴的高度因缺牙与否、缺牙时间、牙周炎等因素影响变异度较大,因此测量DVSF可以避免混杂因素影响。在进行种植术时可依据该指标,对不同牙位的剩余牙槽嵴高度进行测量,以上牙槽后动脉血管至上颌窦底的平均距离+种植区域剩余牙槽嵴距离作为参考。
3.4 LWT与DMSA的相关性对出血风险的提示
既往研究[18]在较厚的上颌窦侧壁中发现了较大直径的MSA,认为LWT也是影响DMSA的一个变量。本研究据此对两者进行了相关性分析,得出在P2、M1牙位的LWT与DMSA存在弱相关,支持了既往研究结论。因此如若开窗区域上颌窦侧壁较厚,应预测存在一定出血风险。
综上,MSA解剖结构变异较大,在进行外侧壁入路的上颌窦底提升术前必须通过CBCT观测MSA的骨孔直径、位置、走形关系以及其相邻的解剖结构,以明确手术的难度及术中血管损伤的概率。术前应当询问患者是否有高血压及服用抗凝药史,术前控制血压并行血常规及凝血七项检查,术中准备结扎及压迫用纱布及止血用骨蜡、电刀等。特别由于男性患者及在M1区域DMSA更大,术中存在较大出血概率,因此需要格外注意该类患者的MSA血管解剖结构及走形位置。随着年龄增大,上颌窦气化程度增加,可能导致MSA与骨壁关系由窦内型向骨内型转变。如果该走形类型动脉位于开窗区域附近,可影响术中黏膜瓣切口位置及开窗位置,故需要特别关注;由于MSA可走形于上颌窦底黏膜处,因此在进行开窗术分离窦底黏膜时需要更加小心,必要时可增大骨窗直径以保证术野的清晰;MSA还可走形于上颌窦底根方牙槽骨中,因此不仅在进行外侧壁入路的上颌窦底提升术时,在进行常规种植术及内侧入路的上颌窦底提升术时,也存在动脉损伤的可能性。为降低可能出现的血肿、感染、种植体松动等并发症,术前应常规采用CBCT找到MSA并进行观测分析。
作者贡献声明
吴炯睿负责实验思路构思、方法设计、数据分析、数据整理和初稿撰写;高益鸣负责实验核实、实验监督和指导。所有作者均阅读并同意了最终稿件的提交。
AUTHOR's CONTRIBUTIONS
WU Jiongrui participated in conceptualization, methodology, formal analysis, data curation and writing original draft. GAO Yiming participated in checking, supervision and leading. All authors have read and agreed to submit the final manuscript.
利益冲突声明
所有作者声明不存在利益冲突。
COMPETING INTERESTS
All authors disclose no relevant conflict of interests.
参考文献