
上海交通大学学报(医学版) ›› 2024, Vol. 44 ›› Issue (5): 543-551.doi: 10.3969/j.issn.1674-8115.2024.05.001
• 高危妊娠专题 • 下一篇
马瑞琳1( ), 刘雨1(
), 刘雨1( ), 徐桂香1, 史昊然1, 崔俭俭1, 杨泽俊1, 毛艳1, 赵茵1,2(
), 徐桂香1, 史昊然1, 崔俭俭1, 杨泽俊1, 毛艳1, 赵茵1,2( )
)
收稿日期:2023-10-16
接受日期:2024-03-04
出版日期:2024-05-28
发布日期:2024-05-28
通讯作者:
赵 茵,电子信箱:Zhaoyin@hust.edu.cn。作者简介:马瑞琳(1997—),女,博士生;电子信箱:maruilin202076100@163.com基金资助:
MA Ruilin1( ), LIU Yu1(
), LIU Yu1( ), XU Guixiang1, SHI Haoran1, CUI Jianjian1, YANG Zejun1, MAO Yan1, ZHAO Yin1,2(
), XU Guixiang1, SHI Haoran1, CUI Jianjian1, YANG Zejun1, MAO Yan1, ZHAO Yin1,2( )
)
Received:2023-10-16
Accepted:2024-03-04
Online:2024-05-28
Published:2024-05-28
Contact:
ZHAO Yin, E-mail: Zhaoyin@hust.edu.cn.Supported by:摘要:
目的·通过超声多普勒检测子痫前期(preeclampsia,PE)大鼠模型子宫动脉、脐动脉、大脑中动脉参数,对比胎盘血管病理及妊娠结局,为评估PE动物模型胎盘功能提供有效方法和参考。方法·利用N-硝基-L-精氨酸甲酯(N′-nitro-L-arginine-methylesterhydrochloride,L-NAME)和0.9%氯化钠溶液腹腔注射,分别建立PE组(n=8)和正常妊娠(normal pregnancy,NP)组(n=8)的SD大鼠动物模型,检测血压和蛋白尿指标评估模型是否成功建立。在妊娠(gestational day,GD)第19日(GD19)时利用超声多普勒检测PE组和NP组子宫动脉、脐动脉以及胎鼠大脑中动脉相关指标,终止妊娠后通过胎盘血管病理、胎鼠胎盘质量情况评估胎盘功能。结果·PE组大鼠的血压(GD15:P=0.001;GD19:P=0.001)、蛋白尿(GD15:P=0.001;GD19:P=0.001)均高于NP组,其胎鼠脐动脉、子宫动脉的搏动指数(pulsation index,PI)显著高于NP组(均P=0.000),胎鼠大脑中动脉阻力指数(resistance index,RI)显著低于NP组(P=0.000)。胎鼠数量无显著差异,PE组胎盘、胎鼠质量显著低于NP组(P=0.006,P=0.000),胎盘组织血管特异性免疫组化染色提示PE组胎盘微血管迷路密度少于NP组(P=0.001)。通过相关性分析发现胎盘微血管迷路密度、胎鼠质量、胎盘质量与脐动脉RI、子宫动脉PI及RI呈负相关,而与大脑中动脉S/D、PI、RI呈正相关(均P<0.05)。结论·超声多普勒检测L-NAME诱导的PE大鼠模型子宫动脉、脐动脉、大脑中动脉指数相关指标可以良好反映妊娠结局和胎盘血管病理情况,可用于评价PE大鼠模型的胎盘血管灌注情况,具有动物模型研究的实用性和便利性。
中图分类号:
马瑞琳, 刘雨, 徐桂香, 史昊然, 崔俭俭, 杨泽俊, 毛艳, 赵茵. 子痫前期大鼠模型子宫动脉、脐动脉、大脑中动脉超声多普勒参数与胎盘血管病理及妊娠结局的关系[J]. 上海交通大学学报(医学版), 2024, 44(5): 543-551.
MA Ruilin, LIU Yu, XU Guixiang, SHI Haoran, CUI Jianjian, YANG Zejun, MAO Yan, ZHAO Yin. Relationship between Doppler ultrasound parameters of uterine artery, umbilical artery, middle cerebral artery and placental vasculopathology and pregnancy outcome in preeclampsia rat model[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2024, 44(5): 543-551.
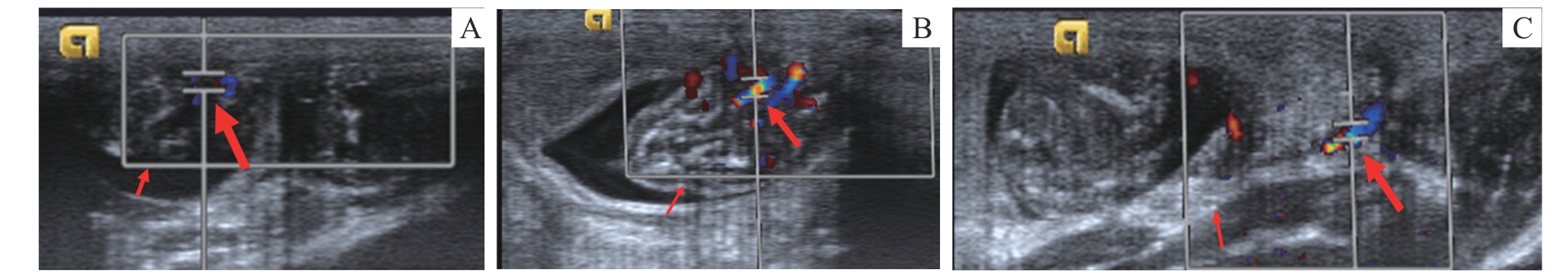
图1 SD大鼠脐动脉、大脑中动脉、子宫动脉的超声成像Note: A. Umbilical artery. Small arrow—fetal rat, large arrow—umbilical cord. B. Middle cerebral artery. Small arrow—fetal rat head, large arrow—middle cerebral artery. C. Uterine artery. Small arrow—lateral edge of the rat uterus, large arrow—uterine artery.
Fig 1 Ultrasound imaging of the umbilical artery, middle cerebral artery and uterine artery in SD rats
| Item | |||
|---|---|---|---|
表1 2组尾动脉血压及尿蛋白比较
Tab 1 Comparison of tail artery blood pressure and urinary protein between the two groups
| Item | |||
|---|---|---|---|
| Item | NP | PE | P value |
|---|---|---|---|
| 7.05±1.51 | 10.51±2.74 | 0.008 | |
| 2.08±0.78 | 1.59±0.71 | 0.203 | |
| 4.26±0.94 | 5.25±1.16 | 0.083 | |
| 3.61±0.97 | 13.95±18.00 | 0.127 | |
| 1.18±0.16 | 1.72±0.13 | 0.000 | |
| 0.71±0.07 | 0.88±0.06 | 0.000 |
表2 超声评价2组胎鼠脐动脉血流动力学的比较
Tab 2 Comparison of fetal umbilical artery hemodynamics using ultrasound evaluation between the two groups
| Item | NP | PE | P value |
|---|---|---|---|
| 7.05±1.51 | 10.51±2.74 | 0.008 | |
| 2.08±0.78 | 1.59±0.71 | 0.203 | |
| 4.26±0.94 | 5.25±1.16 | 0.083 | |
| 3.61±0.97 | 13.95±18.00 | 0.127 | |
| 1.18±0.16 | 1.72±0.13 | 0.000 | |
| 0.71±0.07 | 0.88±0.06 | 0.000 |
| Item | NP group | PE group | P value |
|---|---|---|---|
| 16.27±3.93 | 0.203 | ||
| 7.98±2.50 | 0.067 | ||
| 11.05±3.26 | 0.751 | ||
| 2.05±0.16 | 0.000 | ||
| 0.77±0.10 | 0.000 | ||
| 0.51±0.44 | 0.000 |
表3 超声评价2组子宫动脉血流动力学的比较
Tab 3 Comparison of uterine artery hemodynamics using ultrasound evaluation between the two groups
| Item | NP group | PE group | P value |
|---|---|---|---|
| 16.27±3.93 | 0.203 | ||
| 7.98±2.50 | 0.067 | ||
| 11.05±3.26 | 0.751 | ||
| 2.05±0.16 | 0.000 | ||
| 0.77±0.10 | 0.000 | ||
| 0.51±0.44 | 0.000 |
| Item | NP | PE | P value |
|---|---|---|---|
| 0.264 | |||
| 0.000 | |||
| 0.073 | |||
| 0.000 | |||
| 0.000 | |||
| 0.000 |
表4 超声评价2组胎鼠大脑中动脉血流动力学的比较
Tab 4 Comparison of fetal middle cerebral artery hemodynamics using ultrasound evaluation between the two groups
| Item | NP | PE | P value |
|---|---|---|---|
| 0.264 | |||
| 0.000 | |||
| 0.073 | |||
| 0.000 | |||
| 0.000 | |||
| 0.000 |
| Item | NP group | PE group | P value |
|---|---|---|---|
| Placental quality/ | 0.006 | ||
| Fetal rat quality/ | 4.20 | 0.000 | |
| Fetal number/n | 0.526 |
表5 2组胎盘质量和胎鼠数量、质量比较
Tab 5 Comparison of placental quality, fetal rat number and fetal rat quality between the two groups
| Item | NP group | PE group | P value |
|---|---|---|---|
| Placental quality/ | 0.006 | ||
| Fetal rat quality/ | 4.20 | 0.000 | |
| Fetal number/n | 0.526 |
| P value | |||
|---|---|---|---|
表6 2组MVD比较
Tab 6 Comparison of MVD between the two groups
| P value | |||
|---|---|---|---|
| Item | MVD | Placental quality | Fetal rat quality |
|---|---|---|---|
| PS | -0.657 (0.006) | -0.160 (0.554) | -0.638 (0.008) |
| ED | 0.304 (0.253) | 0.522 (0.038) | 0.354 (0.178) |
| TAV | -0.466 (0.069) | -0.182 (0.500) | -0.424 (0.102) |
| S/D | -0.284 (0.287) | -0.698 (0.003) | -0.353 (0.179) |
| PI | -0.850 (0.000) | -0.450 (0.081) | -0.901 (0.000) |
| RI | -0.758 (0.001) | -0.740 (0.001) | -0.832 (0.000) |
表7 脐动脉相关参数指标与胎盘质量、胎鼠质量及胎盘MVD的相关性分析[r (P)]
Tab 7 Correlation analysis between umbilical artery parameters and placental quality, fetal rat quality and placental MVD [r (P)]
| Item | MVD | Placental quality | Fetal rat quality |
|---|---|---|---|
| PS | -0.657 (0.006) | -0.160 (0.554) | -0.638 (0.008) |
| ED | 0.304 (0.253) | 0.522 (0.038) | 0.354 (0.178) |
| TAV | -0.466 (0.069) | -0.182 (0.500) | -0.424 (0.102) |
| S/D | -0.284 (0.287) | -0.698 (0.003) | -0.353 (0.179) |
| PI | -0.850 (0.000) | -0.450 (0.081) | -0.901 (0.000) |
| RI | -0.758 (0.001) | -0.740 (0.001) | -0.832 (0.000) |
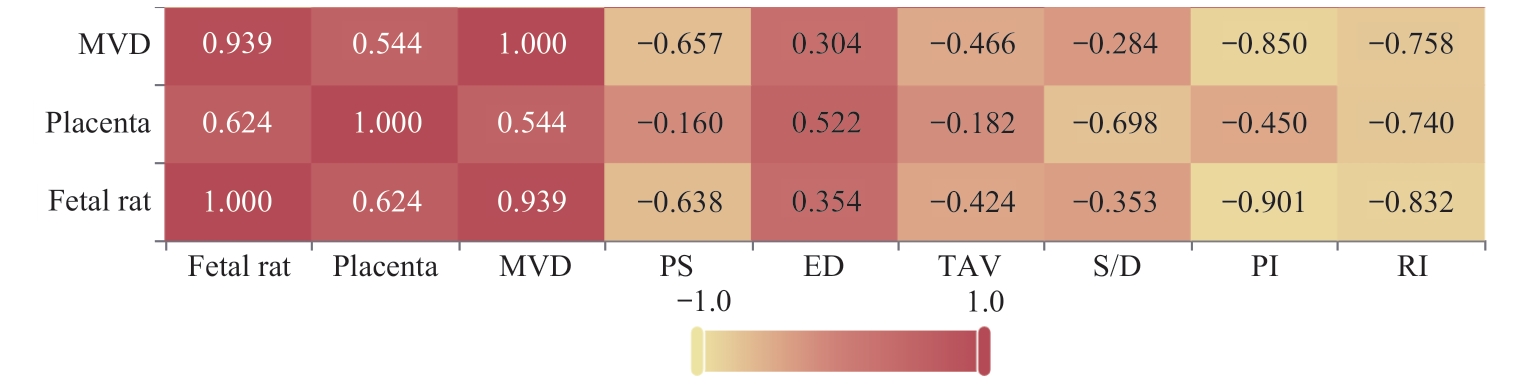
图4 脐动脉相关参数指标与胎盘质量、胎鼠质量及胎盘MVD相关性分析热图Note: Each number in the cells represents a correlation coefficient, with the depth of color indicating the magnitude of the value.
Fig 4 Heatmap of the correlation analysis between umbilical artery parameter indices and placental quality, fetal rat quality and placental MVD
| Item | MVD | Placental quality | Fetal rat quality |
|---|---|---|---|
| PS | -0.332 (0.209) | -0.381 (0.145) | -0.302 (0.256) |
| ED | 0.447 (0.083) | 0.291 (0.274) | 0.487 (0.056) |
| TAV | 0.078 (0.775) | -0.061 (0.824) | 0.123 (0.650) |
| S/D | -0.871 (0.000) | -0.638 (0.008) | -0.870 (0.000) |
| PI | -0.892 (0.000) | -0.615 (0.011) | -0.922 (0.000) |
| RI | -0.874 (0.000) | -0.621 (0.010) | -0.902 (0.000) |
表8 子宫动脉相关参数指标与胎盘质量、胎鼠质量及胎盘MVD的相关性分析[r (P)]
Tab 8 Correlation analysis between uterine artery parameters and placental quality, fetal rat quality and placental MVD [r (P)]
| Item | MVD | Placental quality | Fetal rat quality |
|---|---|---|---|
| PS | -0.332 (0.209) | -0.381 (0.145) | -0.302 (0.256) |
| ED | 0.447 (0.083) | 0.291 (0.274) | 0.487 (0.056) |
| TAV | 0.078 (0.775) | -0.061 (0.824) | 0.123 (0.650) |
| S/D | -0.871 (0.000) | -0.638 (0.008) | -0.870 (0.000) |
| PI | -0.892 (0.000) | -0.615 (0.011) | -0.922 (0.000) |
| RI | -0.874 (0.000) | -0.621 (0.010) | -0.902 (0.000) |
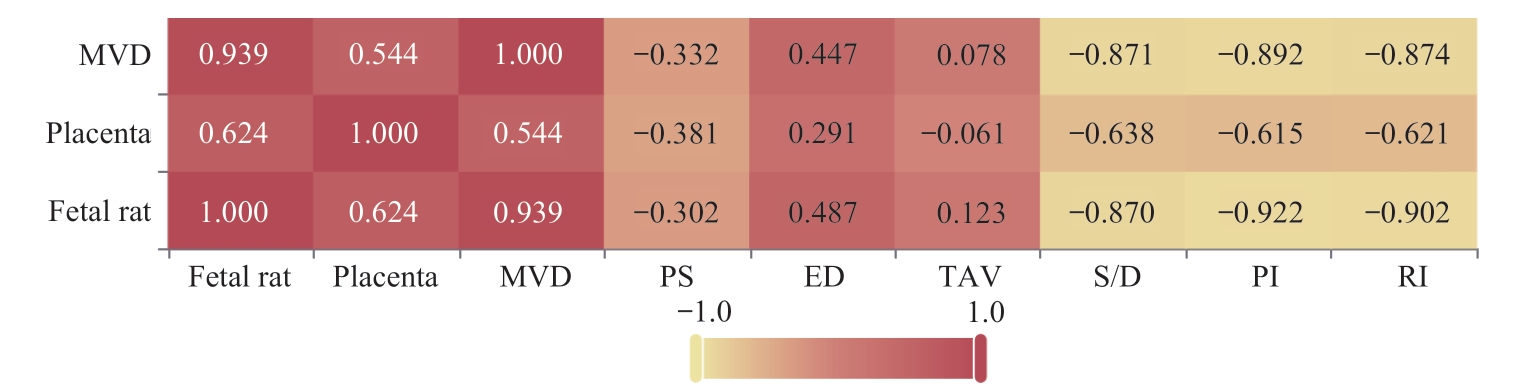
图5 子宫动脉相关参数指标与胎盘质量、胎鼠质量及胎盘MVD相关性分析热图Note: Each number in the cells represents a correlation coefficient, with the depth of color indicating the magnitude of the value.
Fig 5 Heatmap of the correlation analysis between uterine artery parameter indices and placental quality, fetal rat quality and placental MVD
| Item | MVD | Placental quality | Fetal rat quality |
|---|---|---|---|
| PS | -0.148 (0.586) | -0.196 (0.467) | -0.300 (0.260) |
| ED | -0.749 (0.001) | -0.575 (0.020) | -0.802 (0.000) |
| TAV | -0.333 (0.207) | -0.342 (0.195) | -0.451 (0.079) |
| S/D | 0.923 (0.000) | 0.582 (0.018) | 0.915 (0.000) |
| PI | 0.895 (0.000) | 0.571 (0.021) | 0.850 (0.000) |
| RI | 0.914 (0.000) | 0.569 (0.022) | 0.888 (0.000) |
表9 大脑中动脉相关参数指标与胎盘质量、胎鼠质量及胎盘MVD的相关系数
Tab 9 Correlation coefficients between middle cerebral artery parameters and placental quality, fetal rat quality, and placental MVD
| Item | MVD | Placental quality | Fetal rat quality |
|---|---|---|---|
| PS | -0.148 (0.586) | -0.196 (0.467) | -0.300 (0.260) |
| ED | -0.749 (0.001) | -0.575 (0.020) | -0.802 (0.000) |
| TAV | -0.333 (0.207) | -0.342 (0.195) | -0.451 (0.079) |
| S/D | 0.923 (0.000) | 0.582 (0.018) | 0.915 (0.000) |
| PI | 0.895 (0.000) | 0.571 (0.021) | 0.850 (0.000) |
| RI | 0.914 (0.000) | 0.569 (0.022) | 0.888 (0.000) |
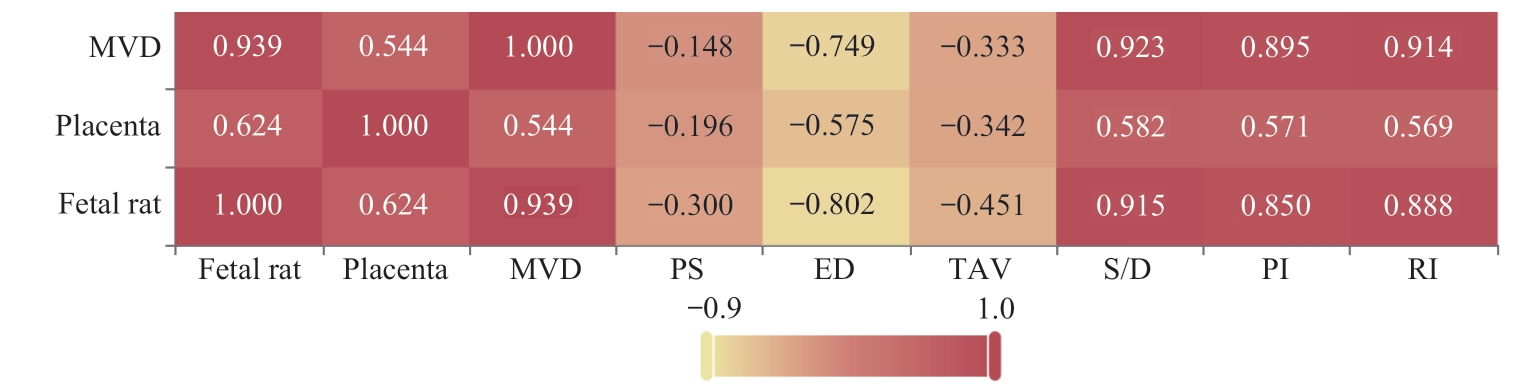
图6 大脑中动脉相关参数指标与胎盘质量、胎鼠质量及胎盘MVD相关性分析热图Note: Each number in the cells represents a correlation coefficient, with the depth of color indicating the magnitude of the value.
Fig 6 Heatmap of the correlation analysis between middle cerebral artery parameter indices and placental quality, fetal rat quality and placental MVD
| 1 | DIMITRIADIS E, ROLNIK D L, ZHOU W, et al. Pre-eclampsia[J]. Nat Rev Dis Primers, 2023, 9(1): 8. |
| 2 | 朱玥霖, 李倩倩, 王雁玲, 等. 胎盘发育和子痫前期[J]. 生物医学转化, 2022, 3(4): 22-29. |
| ZHU Y L, LI Q Q, WANG Y L, et al.Placenta development and preeclampsia[J]. Biomedical Transformation, 2022, 3(4): 22-29. | |
| 3 | VATISH M, POWYS V R, CERDEIRA A S. Novel therapeutic and diagnostic approaches for preeclampsia[J]. Curr Opin Nephrol Hypertens, 2023, 32(2): 124-133. |
| 4 | CARTER A M. Comparative studies of placentation and immunology in non-human primates suggest a scenario for the evolution of deep trophoblast invasion and an explanation for human pregnancy disorders[J]. Reproduction, 2011, 141(4): 391-396. |
| 5 | CARTER A M, PIJNENBORG R. Evolution of invasive placentation with special reference to non-human primates[J]. Best Pract Res Clin Obstet Gynaecol, 2011, 25(3): 249-257. |
| 6 | BAKRANIA B A, GEORGE E M, GRANGER J P. Animal models of preeclampsia: investigating pathophysiology and therapeutic targets[J]. Am J Obstet Gynecol, 2022, 226(2S): S973-S987. |
| 7 | PIJNENBORG R, ROBERTSON W B, BROSENS I, et al. Review article: trophoblast invasion and the establishment of haemochorial placentation in man and laboratory animals[J]. Placenta, 1981, 2(1): 71-91. |
| 8 | VERKESTE C M, SLANGEN B F, DAEMEN M, et al. The extent of trophoblast invasion in the preplacental vasculature of the guinea-pig[J]. Placenta, 1998, 19(1): 49-54. |
| 9 | SOARES M J, CHAKRABORTY D, KARIM RUMI M A, et al. Rat placentation: an experimental model for investigating the hemochorial maternal-fetal interface[J]. Placenta, 2012, 33(4): 233-243. |
| 10 | SHU W, LI H Y, GONG H, et al. Evaluation of blood vessel injury, oxidative stress and circulating inflammatory factors in an L-NAME-induced preeclampsia-like rat model[J]. Exp Ther Med, 2018, 16(2): 585-594. |
| 11 | GINOSAR Y, GIELCHINSKY Y, NACHMANSSON N, et al. BOLD-MRI demonstrates acute placental and fetal organ hypoperfusion with fetal brain sparing during hypercapnia[J]. Placenta, 2018, 63: 53-60. |
| 12 | MARKOVIC S, FAGES A, ROUSSEL T, et al. Placental physiology monitored by hyperpolarized dynamic 13C magnetic resonance[J]. Proc Natl Acad Sci USA, 2018, 115(10): E2429-E2436. |
| 13 | ARTHUIS C J, MENDES V, MÊME S, et al. Comparative determination of placental perfusion by magnetic resonance imaging and contrast-enhanced ultrasound in a murine model of intrauterine growth restriction[J]. Placenta, 2018, 69: 74-81. |
| 14 | DINES V, SUVAKOV S, KATTAH A, et al. Preeclampsia and the kidney: pathophysiology and clinical implications[J]. Compr Physiol, 2023, 13(1): 4231-4267. |
| 15 | FEBRES-CORDERO D A, YOUNG B C. Hypertensive disorders of pregnancy[J]. NeoReviews, 2021, 22(11): e760-e766. |
| 16 | POON L C, SHENNAN A, HYETT J A, et al. The International Federation of Gynecology and Obstetrics (FIGO) initiative on pre-eclampsia: a pragmatic guide for first-trimester screening and prevention[J]. Int J Gynaecol Obstet, 2019, 145(Suppl 1): 1-33. |
| 17 | 谢幸, 孔北华, 段涛. 妇产科学[M]. 9版. 北京: 人民卫生出版社, 2018. |
| XIE X, KONG B H, DUAN T. Obstetrics and Gynecology[M]. The 9th edition. Beijing: People′s Medical Publishing House, 2018. | |
| 18 | USTA A, TURAN G, SANCAKLI USTA C, et al. Placental fractalkine immunoreactivity in preeclampsia and its correlation with histopathological changes in the placenta and adverse pregnancy outcomes[J]. J Matern Fetal Neonatal Med, 2020, 33(5): 806-815. |
| 19 | TICA O S, TICA A A, COJOCARU D, et al. Maternal steroids on fetal doppler indices, in growth-restricted fetuses with abnormal umbilical flow from pregnancies complicated with early-onset severe preeclampsia[J]. Diagnostics, 2023, 13(3): 428. |
| 20 | SHI M T, YANG X F, SUN L, et al. Comparison of different modified operations in the reduced uteroplacental perfusion pressure rat model of preeclampsia[J]. J Reprod Immunol, 2023, 156: 103815. |
| 21 | SAKOWICZ A, BRALEWSKA M, KAMOLA P, et al. Reliability of rodent and rabbit models in preeclampsia research[J]. Int J Mol Sci, 2022, 23(22): 14344. |
| 22 | Zeisler H, Llurba E, Chantraine F, et al. Predictive value of the sFlt-1:PlGF ratio in women with suspected preeclampsia[J]. N Engl J Med, 2016, 374(1): 13-22. |
| 23 | ARTHUIS C J, NOVELL A, ESCOFFRE J M, et al. New insights into uteroplacental perfusion: quantitative analysis using doppler and contrast-enhanced ultrasound imaging[J]. Placenta, 2013, 34(5): 424-431. |
| 24 | SPRADLEY F T, GE Y, GRANGER J P, et al. Utero-placental vascular remodeling during late gestation in Sprague-Dawley rats[J]. Pregnancy Hypertens, 2020, 20: 36-43. |
| 25 | TRAVIS O K, TARDO G A, GIACHELLI C, et al. Interferon γ neutralization reduces blood pressure, uterine artery resistance index, and placental oxidative stress in placental ischemic rats[J]. Am J Physiol Regul Integr Comp Physiol, 2021, 321(2): R112-R124. |
| 26 | BIBEAU K, SICOTTE B, BÉLAND M, et al. Placental underperfusion in a rat model of intrauterine growth restriction induced by a reduced plasma volume expansion[J]. PLoS One, 2016, 11(1): e0145982. |
| 27 | PAPAGEORGHIOU A T, YU C K H, ERASMUS I E, et al. Assessment of risk for the development of pre-eclampsia by maternal characteristics and uterine artery doppler[J]. BJOG, 2005, 112(6): 703-709. |
| 28 | ZHOU P, SUN Y, TAN Y P, et al. Fetal and neonatal middle cerebral artery hemodynamic changes and significance under ultrasound detection in hypertensive disorder complicating pregnancy patients with different severities[J]. Comput Math Methods Med, 2022, 2022: 6110228. |
| [1] | 糜小扬, 丁莹, 陈奕静, 贾洁. 孕期超加工食品摄入与妊娠结局关系的研究进展[J]. 上海交通大学学报(医学版), 2025, 45(1): 113-121. |
| [2] | 周天凡, 邵飞雪, 万盛, 周晨晨, 周思锦, 花晓琳. 基于人工智能模型量化视网膜血管特征参数预测子痫前期的可行性研究[J]. 上海交通大学学报(医学版), 2024, 44(5): 552-559. |
| [3] | 李玉, 张羽. 慢性肾脏病患者不良妊娠结局的危险因素分析[J]. 上海交通大学学报(医学版), 2024, 44(5): 560-566. |
| [4] | 黄勤, 黄缨, 李文. 输卵管复合妊娠的超声检查时间探讨[J]. 上海交通大学学报(医学版), 2024, 44(12): 1545-1551. |
| [5] | 耿瑶, 张杨, 赵洁, 李伟, 蔡国青. MTA1在子痫前期胎盘组织中的表达及其对滋养细胞功能的影响[J]. 上海交通大学学报(医学版), 2024, 44(11): 1383-1390. |
| [6] | 张方, 王筱金, 马珏, 何韵婷, 何豪, 翟晶, 郭玉娜, 陈焱, 王炳顺. 妊娠早期血脂谱与子痫前期发病风险的关系——基于真实世界数据的研究[J]. 上海交通大学学报(医学版), 2021, 41(4): 483-488. |
| [7] | 曾金妹, 陈日玲, 何洁云, 梁东梅, 练婷玉, 尹明娟, 饶佳为, 倪进东. 高龄初产妇妊娠并发症和不良妊娠结局分析[J]. 上海交通大学学报(医学版), 2021, 41(11): 1485-1490. |
| [8] | 林 静1, 2,刘 含1, 2,刘欣梅1, 2,陈小君1,黄荷凤1, 2. 高龄初产妇与高龄经产妇的妊娠结局比较[J]. 上海交通大学学报(医学版), 2020, 40(1): 58-. |
| [9] | 吴轲 1,孙涵潇 2,蔡美琴 1. 类胡萝卜素对母婴健康影响的研究进展[J]. 上海交通大学学报(医学版), 2019, 39(8): 929-. |
| [10] | 张素群,倪琛,盛美萍,汪云. 体外受精-胚胎移植术中单胚胎移植与双胚胎移植的妊娠结局及影响因素分析[J]. 上海交通大学学报(医学版), 2019, 39(6): 642-. |
| [11] | 顾燕1,蔡孟1,宋云1,蒲才秀2. 右美托咪定复合舒芬太尼用于重度子痫前期剖宫产产妇术后自控静脉镇痛的研究[J]. 上海交通大学学报(医学版), 2018, 38(7): 784-. |
| [12] | 刘丹,周洪贵,李明星,张煜,彭莉晴 . 二维超声联合四维彩色多普勒超声在子宫占位性病变诊断中的应用[J]. 上海交通大学学报(医学版), 2017, 37(7): 969-. |
| [13] | 江珊,徐上妍,宋琳琳,等. 甲状腺结节血供程度与弹性评分的相关性研究[J]. 上海交通大学学报(医学版), 2015, 35(5): 714-. |
| [14] | 沈璐,杨祖菁,叶伟萍,等. GNA12基因甲基化与子痫前期的相关性分析[J]. 上海交通大学学报(医学版), 2015, 35(5): 698-. |
| [15] | 顾 玮,周雷平,林 婧,等. 子宫动脉血流值在子痫前期中的预测价值[J]. 上海交通大学学报(医学版), 2015, 35(2): 223-. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||