原发甲状腺淋巴瘤(primary thyroid lymphoma,PTL)是一种罕见的甲状腺恶性肿瘤,约占结外淋巴瘤的2%[1],占所有甲状腺恶性肿瘤的1%~5%[2]。PTL主要的病理类型为弥漫性大B细胞淋巴瘤(diffuse large B-cell lymphoma,DLBCL),其次为黏膜相关边缘区B细胞淋巴瘤(mucosa-associated lymphoid tissue,MALT)[3]。原发甲状腺DLBCL定义为起源于甲状腺内淋巴组织的恶性肿瘤,伴或不伴有颈部淋巴结受累,且除颈部淋巴结病变局部浸润或远处转移到甲状腺的肿瘤外,经病理确诊为DLBCL[4-6]。继发甲状腺DLBCL为首先影响淋巴结和其他器官,后扩散至甲状腺的DLBCL。甲状腺DLBCL主要表现为颈部迅速增大的无痛性肿块,多见于中年女性[7]。本研究回顾性分析上海交通大学医学院附属瑞金医院收治的66例甲状腺DLBCL患者,旨在通过分析患者的临床病理特征、基因突变谱以及相关预后因素,探究原发和继发甲状腺DLBCL临床和预后特征差异,为临床治疗提供依据。
1 对象与方法
1.1 研究对象及资料收集
纳入2003年11月—2021年12月上海交通大学医学院附属瑞金医院收治的初次诊断为甲状腺DLBCL患者66例[其中23例(34.8%)为原发甲状腺DLBCL,43例(65.2%)为继发甲状腺DLBCL]。
纳入标准:① 所有患者均有完整的血常规等实验室指标、心电图、骨髓穿刺、全身CT或正电子发射计算机断层扫描(positron emission tomography-computed tomography,PET-CT)等检查结果。② 经病理组织活检及免疫组织化学染色确诊,并根据2016年世界卫生组织(WHO)淋巴瘤分类标准[8]进行病理复核。③ 患者PET-CT显示累及结外器官甲状腺。
收集患者一般信息,包括性别、年龄、美国东部肿瘤协作组(Eastern Cooperative Oncology Group,ECOG)评分、Ann Arbor分期、淋巴瘤病理免疫组织化学分析[Hans分型,MYC和BCL2蛋白双表达(double expression,DE)]、国际预后指数(international prognostic index,IPI)、乳酸脱氢酶(lactate dehydrogenase,LDH;参考值为120~250 IU/L)、PET-CT报告、是否行甲状腺切除术、治疗方案、靶向测序报告等,并随访其疾病转归及生存情况。
1.2 治疗方案
66例患者中,55例(83%)接受以利妥昔单克隆抗体(单抗)联合环磷酰胺、阿霉素、长春新碱及泼尼松(rituximab+cyclophosphamide+doxorubicin+vincristine+prednisone,R-CHOP)为基础的化学治疗(化疗)方案4~6个周期。其余11例患者采用非R-CHOP方案,主要包括利妥昔单抗联合依托泊苷、强的松、长春新碱、环磷酰胺、多柔霉素(dose-adjusted application of rituximab,etoposide,prednisone,vincristine,cyclophosphamide,and doxorubicin,DA-EPOCH-R),鲁顿酪氨酸激酶(Bruton′s tyrosine kinase,BTK)抑制剂联合来那度胺、利妥昔单抗等。
1.3 疗效评价及分期
化疗结束后对患者进行评估,评估手段包括42例(63.6%)采用PET-CT和24例(36.4%)采用颈部、胸部、腹部、盆腔增强CT。采用2014年版卢加诺(Lugano)淋巴瘤疗效评价标准[9-10]进行治疗效果评估,包括完全缓解(complete response,CR)、部分缓解(partial response,PR)、疾病稳定(stable disease,SD)、疾病进展(progressive disease,PD),客观缓解率(objective response rate,ORR)=CR率+PR率。按照Ann Arbor分期标准对患者进行临床分期,体能状态评分为ECOG评分,预后因素采用IPI。
1.4 随访
采用门诊、电话及查阅病历资料的方式进行随访。无进展生存(progress free survive,PFS)时间为从诊断起至第一次肿瘤进展、因任何原因死亡或随访终点的时间。总生存(overall survival,OS)时间为从诊断起至确认死亡或随访终点的时间。随访截止时间为2022年12月17日。
1.5 靶向测序基因突变
66例患者中,40例进行了靶向测序[原发甲状腺DLBCL患者13例(32.5%),继发甲状腺DLBCL患者27例(67.5%)]。应用组织基因组DNA(gDNA)提取试剂盒(Promega,美国)提取gDNA。取1 μg DNA制备DNA全基因组文库。使用PCR引物扩增目的基因(55个淋巴瘤相关基因),将目标区域DNA富集后,采用Novaseq(Illumina,美国)测序平台进行测序。测序后原始数据利用CCDS(Consensus Coding Sequence)、人基因组数据库(hg19)、dbSNP(v138)、1000 genomes、COSMIC(Catalogue of Somatic Mutations in Cancer)、PolyPhen、SIFT(Sortig Intolerant From Tolerant)等进行生物信息学分析,确定致病基因突变位点。
1.6 统计学分析
采用SPSS 25.0统计软件分析数据。定量资料以M(最小值~最大值)表示。定性资料以频数(百分比)表示,组间比较采用χ2检验及Fisher确切概率法。采用Kaplan-Meier法绘制生存曲线,Log-rank检验比较组间PFS、OS的差异。应用Log-rank检验进行单因素分析,将单因素分析P<0.05的因素纳入Cox比例风险模型进行多因素分析。使用Mann-Whitney U检验分析基因突变差异。P<0.05表示差异具有统计学意义。
2 结果
2.1 患者临床病理特征分析
66例患者中位年龄为64(18~84)岁,38例(58%)>60岁,43例(65%)为女性,9例(14%)ECOG评分≥2分,32例(48%)为Ann Arbor分期Ⅲ~Ⅳ期,37例(56%)LDH升高,28例(42%)结外器官受累数目≥2个,42例(64%)为生发中心B细胞(germinal center B-cell,GCB),15例(23%)为DE,28例(42%)IPI为3~5分,19例(29%)曾接受甲状腺切除。
原发和继发甲状腺DLBCL患者在性别、年龄、ECOG评分上差异无统计学意义。原发和继发患者Ann Arbor分期Ⅲ~Ⅳ期(P=0.000)、LDH是否升高(P=0.043)、结外器官受累数目≥2个(P=0.000)、Hans分型(P=0.030)、DE(P=0.026)、IPI评分3~5分(P=0.000)、是否进行甲状腺手术切除(P=0.012)的比例的差异具有统计学意义(表1)。
表1 原发和继发甲状腺DLBCL患者临床病理特征分析
Tab 1
| Characteristic | Primary thyroid DLBCL (n=23) | Secondary thyroid DLBCL (n=43) | χ2 | P value |
|---|---|---|---|---|
| Gender/n(%) | 0.303 | 0.582 | ||
| Male | 7 (30.4) | 16 (37.2) | ||
| Female | 16 (9.6) | 27 (62.8) | ||
| Age/n(%) | 0.422 | 0.516 | ||
| ≤60 years | 11 (47.8) | 17 (39.5) | ||
| >60 years | 12 (52.2) | 26 (60.5) | ||
| ECOG score/n(%) | 0.229 | 0.632 | ||
| 0‒1 score | 21 (91.3) | 36 (83.7) | ||
| ≥2 score | 2 (8.7) | 7 (16.3) | ||
| Ann Arbor stage/n(%) | 33.226 | 0.000 | ||
| Ⅰ‒Ⅱ | 23 (100) | 11 (25.6) | ||
| Ⅲ‒Ⅳ | 0 (0) | 32 (74.4) | ||
| LDH/n(%) | 4.108 | 0.043 | ||
| Normal | 14 (60.9) | 15 (34.9) | ||
| Elevated | 9 (39.1) | 28 (65.1) | ||
| Extranodal involvement/n(%) | 26.012 | 0.000 | ||
| 0‒1 | 23 (100) | 15 (34.9) | ||
| ≥2 | 0 (0) | 28 (65.1) | ||
| Hans/n(%) | 4.694 | 0.030 | ||
| GCB | 18/21 (85.7) | 24/41 (58.5) | ||
| non-GCB | 3/21 (14.3) | 17/41 (41.5) | ||
| DE/n(%) | 4.933 | 0.026 | ||
| Yes | 1/17 (5.9) | 14/35 (40.0) | ||
| No | 16/17 (94.1) | 21/35 (60.0) | ||
| IPI/n(%) | 12.476 | 0.000 | ||
| 0‒2 score | 20 (87.0) | 18 (41.9) | ||
| 3‒5 score | 3 (13.0) | 25 (58.1) | ||
| Thyroidectomy/n(%) | 6.242 | 0.012 | ||
| Yes | 11 (47.8) | 8 (18.6) | ||
| No | 12 (52.2) | 35 (81.4) |
2.2 疗效评估与结局评价
66例患者均进行疗效评估,其中47例CR(71%),6例PR(9%),ORR为80%,13例SD或PD(20%)。23例原发甲状腺DLBCL患者中,20例患者CR(87%),ORR为87%,3例患者SD或PD(13%);43例继发甲状腺DLBCL患者中,27例患者CR(63%),6例患者PR(14%),ORR为77%,10例患者SD或PD(23%)。原发甲状腺DLBCL患者的CR率高于继发甲状腺DLBCL(P=0.039),组间PR、ORR,以及SD或PD的差异均无统计学意义。
2.3 基于R-CHOP治疗方案的患者的生存分析
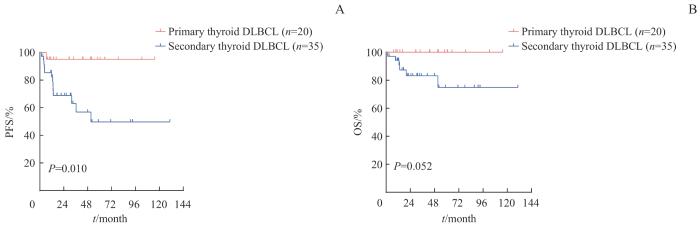
基于R-CHOP治疗方案的甲状腺DLBCL患者55例,中位随访时间为33.7(95%CI 19.6~47.8)个月,整体预期5年PFS率为66.2%,预期5年OS率为84.3%。其中,原发甲状腺DLBCL患者(n=20)预期5年PFS率为95.0%,高于继发甲状腺DLBCL患者(n=35)的49.7%,差异具有统计学意义(P=0.010)。
原发甲状腺DLBCL患者预期5年OS率100%,继发甲状腺DLBCL患者预期5年OS率74.9%,差异无统计学意义(图1)。
图1
图1
原发甲状腺DLBCL和继发甲状腺DLBCL患者的PFS(A)和OS(B)曲线
Note: Survival analysis of 55 patients based on R-CHOP.
Fig 1
PFS (A) and OS (B) curves in patients with primary and secondary thyroid DLBCL
2.4 预后因素分析
对55例接受基于R-CHOP治疗方案的患者进行预后因素分析。单因素分析显示,Ann Arbor分期Ⅲ~Ⅳ期、LDH升高、non-GCB、DE是PFS的不良预后因素,Ann Arbor分期Ⅲ~Ⅳ期、LDH升高、DE是OS的不良预后因素(表2)。多因素Cox分析显示,Ann Arbor Ⅲ~Ⅳ期(HR=4.693,95%CI 1.218~18.081,P=0.025)和LDH升高(HR=5.058,95%CI 1.166~21.941,P=0.030)为PFS独立预后不良因素,结果未显示OS的独立预后不良因素。
表2 影响甲状腺DLBCL患者预后的单因素分析
Tab 2
| Item | PFS | OS | ||
|---|---|---|---|---|
| HR (95%CI) | P value | HR (95%CI) | P value | |
| Gender | 1.593 (0.558‒4.544) | 0.380 | 1.638 (0.330‒8.117) | 0.542 |
| Age>60 years | 1.699 (0.565‒5.113) | 0.340 | 5.647 (0.635‒50.183) | 0.084 |
| ECOG score≥2 score | 2.932 (0.640‒13.426) | 0.146 | 2.940 (0.343‒25.216) | 0.302 |
| Ann Arbor stage Ⅲ‒Ⅳ | 4.411 (1.373‒14.170) | 0.007 | 7.088 (0.827‒60.717) | 0.037 |
| LDH elevated | 5.500 (1.519‒19.911) | 0.004 | 6.982 (0.809‒60.266) | 0.040 |
| Extranodal involvement≥2 | 2.505 (0.867‒7.235) | 0.079 | 3.248 (0.593‒17.788) | 0.151 |
| non-GCB | 5.291 (1.667‒16.788) | 0.002 | 3.066 (0.597‒15.744) | 0.159 |
| DE | 6.178 (1.813‒21.058) | 0.001 | 18.079 (1.837‒177.923) | 0.001 |
| Thyroidectomy | 0.259 (0.058‒1.162) | 0.058 | 0.377 (0.044‒3.226) | 0.354 |
2.5 基因突变分析
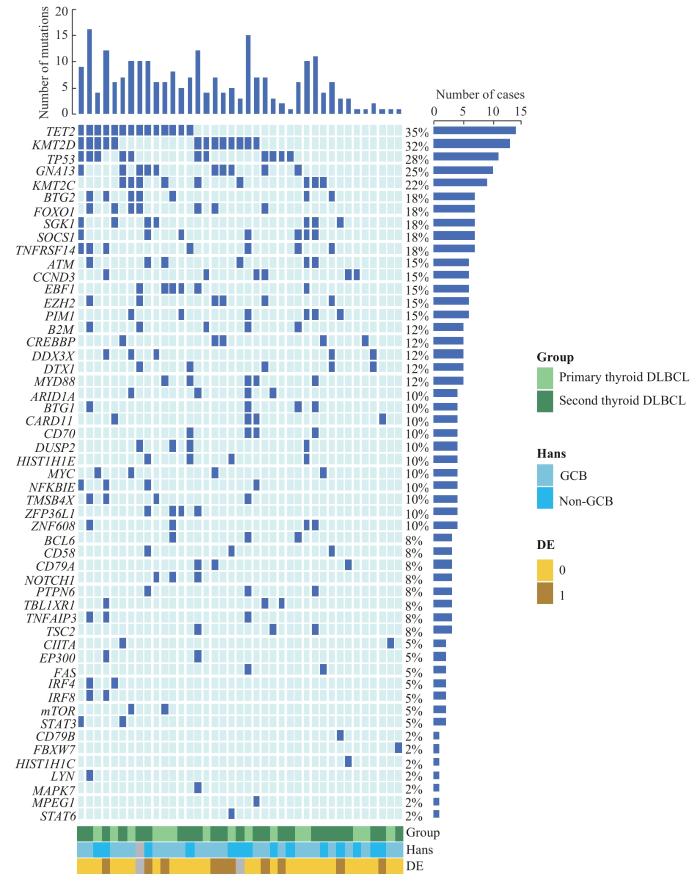
靶向测序结果显示,共检测到53个基因发生了突变。如图2所示,突变频率>20%的基因包括TET2(n=14,35%)、KMT2D(n=13,32%)、TP53(n=11,28%)、GNA13(n=10,25%)、KMT2C
图2
图2
甲状腺DLBCL患者的基因突变图谱
Note: TET2—tet methylcytosine dioxygenase 2; KMT2D—lysine methyltransferase 2D; TP53—tumor protein p53; GNA13—G protein subunit α13; KMT2C—lysine methyltransferase 2C; BTG2—BTG anti-proliferation factor 2; FOXO1—forkhead box O1; SGK1—serum/glucocorticoid regulated kinase 1; SOCS1—suppressor of cytokine signaling 1; TNFRSF14—TNF receptor superfamily member 14; ATM—ATM serine/threonine kinase; CCND3—cyclin D3; EBF1—EBF transcription factor 1; EZH2—enhancer of zeste 2 polycomb repressive complex 2 subunit; PIM1—Pim-1 proto-oncogene, serine/threonine kinase; B2M—β2-microglobulin; CREBBP—CREB binding protein; DDX3X—DEAD-box helicase 3 X-linked; DTX1—deltex E3 ubiquitin ligase 1; MYD88—MYD88 innate immune signal transduction adaptor; ARID1A—AT-rich interaction domain 1A; BTG1—BTG anti-proliferation factor 1; CARD11—caspase recruitment domain family member 11; CD70—CD70 molecule; DUSP2—dual specificity phosphatase 2; HIST1H1E—H1.4 linker histone, cluster member; MYC—MYC proto-oncogene, bHLH transcription factor; NFKBIE—NFKB inhibitor epsilon; TMSB4X—thymosin β4 X-linked; ZFP36L1—ZFP36 ring finger protein-like 1; ZNF608—zinc finger protein 608; BCL6—BCL6 transcription repressor; CD58—CD58 molecule; NOTCH1—notch receptor 1; PTPN6—protein tyrosine phosphatase non-receptor type 6; TBL1XR1—TBL1X/Y-related 1; TNFAIP3—TNFα-induced protein 3; TSC2—TSC complex subunit 2; CIITA—class Ⅱ major histocompatibility complex transactivator; EP300—E1A binding protein p300; FAS—Fas cell surface death receptor; IRF4—interferon regulatory factor 4; IRF8—interferon regulatory factor 8; mTOR—mechanistic target of rapamycin kinase; STAT3—signal transducer and activator of transcription 3; FBXW7—F-box and WD repeat domain containing 7; HIST1H1C—H1.2 linker histone, cluster member; LYN—LYN proto-oncogene, Src family tyrosine kinase; MAPK7—mitogen-activated protein kinase 7; MPEG1—macrophage-expressed 1; STAT6—signal transducer and activator of transcription 6.
Fig 2
Gene mutation profiles in thyroid DLBCL patients
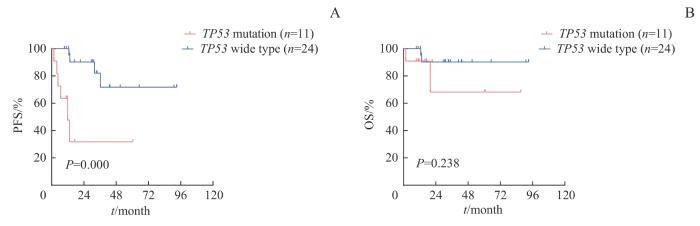
(n=9,22%),且TP53突变是甲状腺DLBCL患者PFS的不良预后因素(P=0.000,图3)。突变率≥10%的基因中,未发现原发与继发甲状腺DLBCL间存在差异。
图3
图3
甲状腺DLBCL患者 TP53 基因的突变状态与PFS(A)和OS(B)的关系
Fig 3
PFS (A) and OS curves (B) in patients with thyroid DLBCL TP53 gene mutation
3 讨论
在本研究中,55例(83%)患者接受以R-CHOP为基础的治疗方案。甲状腺DLBCL患者预期5年OS为84.3%,原发、继发甲状腺DLBCL患者预期5年OS率分别为100%、74.9%。与文献[13]报道侵袭性B细胞淋巴瘤5年OS率[原发甲状腺(82.5%±11.3%)、继发甲状腺(71.8%±15.3%)]相近。
二代测序可以通过研究疾病分子突变来揭示疾病分子机制,并进一步行分子分型。本研究对40例甲状腺DLBCL患者肿瘤组织样本进行靶向与淋巴瘤相关的55个基因测序,来检测基因突变状态,结果发现TET2、KMT2D、TP53、GNA13、KMT2C在甲状腺DLBCL患者中具有较高的突变率。本研究中,未发现原发与继发组间突变率≥10%的基因存在突变差异,可能与病例数相对较少有关。TET2突变与DLBCL ST2分型有关[14],ST2型为SGK1和TET2突变,其中小鼠成熟B细胞Tet2突变缺失会扰乱B细胞的稳态,并导致GCB淋巴瘤进展。ST2分型中,P2RY8(P2Y receptor family member 8)和相应的信号调节因子GNA13突变失活抑制S-geranylgeranyl-L-glutathione反应,进而抑制B细胞的正常空间分布[15]。TP53突变与淋巴瘤进展有关,包括干扰素(interferon,IFN)下调,抑制细胞凋亡,诱导免疫抑制的肿瘤微环境等。TP53突变的患者预后较差[16],与甲状腺DLBCL较低的PFS相关。既往研究显示,TP53突变患者可在R-CHOP基础上联合地西他滨治疗[17],提示R-CHOP联合地西他滨或可提升TP53突变的甲状腺DLBCL患者预后。
综上所述,甲状腺淋巴瘤是一种罕见的结外淋巴瘤,病理类型以DLBCL为主。原发甲状腺DLBCL生存情况优于继发甲状腺DLBCL。Ann Arbor Ⅲ~Ⅳ期、LDH升高、non-GCB、DE(MYC和BCL2蛋白)是影响甲状腺DLBCL患者的不良预后因素。TET2、KMT2D、TP53、GNA13、KMT2C是甲状腺DLBCL中常见的高突变基因,以TP53为靶点或将为甲状腺DLBCL的治疗提供新的方案。
作者贡献声明
杜沚珊负责研究实施、数据分析解释。杜沚珊、王玥、石子旸、施晴、易红梅、董磊参与数据采集。王黎、程澍、许彭鹏、赵维莅参与文章审阅。许彭鹏负责实验设计、统计分析,提供研究经费,并提供研究及写作指导。赵维莅负责研究设计。杜沚珊、许彭鹏参与文章起草。所有作者均阅读并同意了最终稿件的提交。
AUTHOR's CONTRIBUTIONS
DU Zhishan participated in research implementation, data analysis and interpretation. DU Zhishan, WANG Yue, SHI Ziyang, SHI Qing, YI Hongmei, and DONG Lei collected study data. WANG Li, CHENG Shu, XU Pengpeng, and ZHAO Weili reviewed the article. XU Pengpeng designed experiments, analyzed data, provided research fund, and provided research and writing guidance. ZHAO Weili designed the research. DU Zhishan and XU Pengpeng drafted the article. All the authors have read the last version of paper and consented for submission.
利益冲突声明
所有作者声明不存在利益冲突。
COMPETING INTERESTS
All authors disclose no conflicts of interest.
参考文献