认知功能障碍表现为语言、记忆、推理等一个或多个认知领域的认知能力降低[3]。既往研究通过中枢神经系统生命体征量表(Central Nervous System Vital Signs,CNSVS)发现,肥胖青少年在记忆、执行功能等方面的得分均显著低于健康青少年[4],提示肥胖青少年的认知功能减退。此外,有研究[5]报道,与对照组儿童相比,肥胖儿童的注意转换功能方面也存在缺陷。相比于认知相关量表,行为学试验对认知功能的评估更为敏感[6]。Flanker任务也叫侧抑制任务,要求受试者在接受目标刺激时作出反应,同时抑制无关刺激的影响,可反映个体对认知冲突的加工能力[7];其中,一致性刺激用于评估基本认知功能,不一致性刺激用于评估高阶认知功能[8]。Flanker任务在执行功能的研究中有着较广泛的应用,是评估认知控制的合适工具,但在青少年的认知控制研究方面应用相对有限[9]。n-back任务又叫倒数n项测试范式,可反映个体在短时间内存储和处理信息的能力,其中0-back任务用于评估即时记忆,1-back与2-back任务用于评估延迟记忆[10];同时,该任务也可用于评估个体的工作记忆,而工作记忆在阅读理解、推理、算术计算、数学问题解决、学习成绩提高中均发挥了重要作用[11]。然而,目前针对超重和肥胖青少年采用行为学试验开展的系统性认知评估研究仍较缺乏。
研究表明,认知相关疾病和肥胖之间的联系可能是由内分泌因子的多效性作用介导的,特别是一些由代谢相关组织器官分泌的内分泌因子[如瘦素、脂联素和成纤维细胞生长因子21(fibroblast growth factor 21,FGF21)等],其可透过血脑屏障作用于中枢神经系统,参与认知相关疾病的发生与发展[12]。FGF21是一种调节机体糖脂代谢和能量稳态的激素样内分泌因子,主要在肝脏、脂肪等组织中表达;同时,FGF21可由全身多处组织分泌产生并发挥神经保护作用,即可由中枢神经系统内细胞(胶质细胞、神经元等)少量产生以直接发挥保护作用,或由外周组织产生后穿过血脑屏障进入中枢神经系统来间接发挥保护作用[13]。研究[14]发现,FGF21能够通过降低D-半乳糖诱导的衰老小鼠的海马损伤,改善其认知功能。然而,在人群中尤其是肥胖青少年中,血清FGF21水平与认知功能的关系尚不清楚。
本研究采用行为学试验(包括Flanker任务、n-back任务)综合评估青少年的认知功能,分析青少年肥胖相关代谢指标与认知功能的相关性以及青少年超重和肥胖对认知功能的影响因素,并探索血清FGF21与青少年认知功能的联系,以期为肥胖引起认知功能改变的机制研究提供新的视角。
1 对象与方法
1.1 研究对象及其分组
本研究人群来自教育部实践共同体项目合作单位——上海市某高级中学2022年9月—2023年7月的在校高一、高二学生。纳入标准:年龄为15~18周岁;近90 d内体质量稳定(自我报告体质量变化<5 kg)。排除标准:有减重药物使用史或接受过肥胖外科治疗;患有非单纯性肥胖,包括内分泌与代谢性疾病(如库欣综合征、甲状腺功能低下、性腺功能减退、多囊卵巢综合征等)、肿瘤及创伤等;有严重精神疾病(如精神分裂症、双相情感障碍、重度抑郁)病史;患有神经性贪食症障碍。
最终,本研究共纳入175名青少年,依据中华人民共和国卫生行业标准——学龄儿童青少年超重与肥胖筛查[15]将其分为肥胖组(n=75)、超重组(n=50)及正常体型组(n=50)。其中,3组青少年的性别比、年龄均相匹配。
1.2 研究方法
1.2.1 资料的记录及收集
记录受试者的一般资料:① 一般人口学资料,包括年龄、性别。② 人体测量学资料,包括身高、体质量、腰围、臀围、收缩压(systolic blood pressure,SBP)、舒张压(diastolic blood pressure,DBP)及体成分数据(体脂肪量、体脂率),并计算体质量指数(body mass index,BMI)和腰臀比。同时,收集受试者的实验室检测指标,包括空腹血糖(fasting plasma glucose,FPB)、空腹胰岛素(fasting insulin,FINS)、糖化血红蛋白(glycosylated hemoglobin,HbA1c)、血肌酐(serum creatinine,Scr)、尿酸(uric acid,UA)、丙氨酸转氨酶(alanine transaminase,ALT)、天冬氨酸转氨酶(aspartate transaminase,AST)、γ‑谷氨酰转肽酶(γ-glutamyl transpeptidase,GGT)、总胆固醇(total cholesterol,TC)、三酰甘油(triacylglycerol,TAG)、高密度脂蛋白胆固醇(high density lipoprotein cholesterol,HDL-Ch)及低密度脂蛋白胆固醇(low density lipoprotein cholesterol,LDL-Ch)。
1.2.2 行为学试验方法
采用行为学试验评估青少年的认知功能。该试验需在学校的计算机教室完成,保持环境安静,所有受试者间隔落座且中间设有挡板。主试者为经过行为学试验标准化培训的学校老师,负责指导受试者使用E-Prime 3.0软件参与行为学试验。试验前,由主试者为受试者播放规则讲解视频,并接受受试者对于规则的提问,通过示范例题明确受试者已理解规则后开始正式试验。行为学试验的表现包括正确率(accuracy,ACC)和反应时共2个指标。
(1)Flanker任务
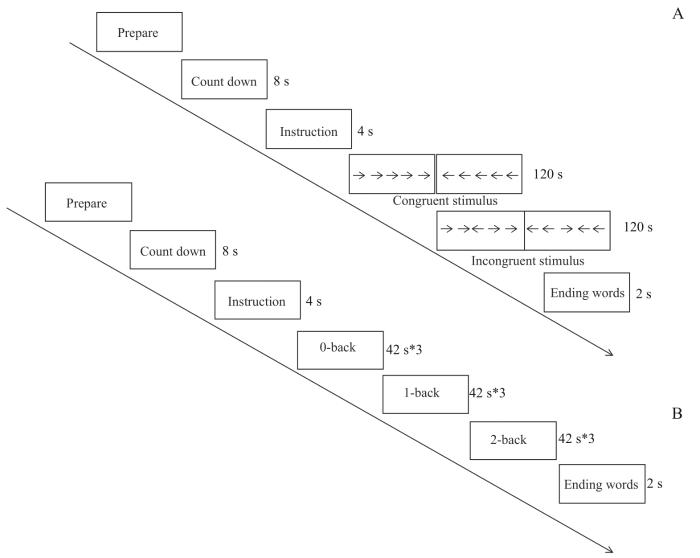
该任务的试验流程如图1A所示。测试过程中,受试者首先在电脑屏幕上看到“倒计时3、2、1”,接着看到指导语“请判断中间箭头的朝向,朝左请按1,朝右请按2”,随后看到一致性刺激和不一致性刺激图片,两类刺激图片各呈现120 s,最后看到结束语。试验流程共2个组块(block),每个组块有40个刺激,一致性刺激与不一致性刺激比例为1∶1,以随机顺序呈现,受试者的观察距离为1 m。正式试验前需对受试者进行训练,使受试者熟悉试验情景,减低练习效应。
图1
图1
行为学试验流程图
Note: A. Flanker task. B. n-back task.
Fig 1
Flowchart of behavioral experiment
(2)n-back任务
该任务的试验流程如图1B所示。测试过程中,受试者首先在电脑屏幕上看到“倒计时,3、2、1”,接着看到指导语“请判断当前字母与字母X(0-back)/上一个(1-back)/上上一个字母(2-back)是否相同,相同请按1,不相同请按2”,随后看到字母,每一组块呈现时间为42 s、各重复3次,最后看到结束语。试验流程共9个组块,每个组块包含12个刺激。受试者的观察距离为1 m。正式试验前需对受试者进行训练,使受试者熟悉试验情景,减低练习效应。
1.2.3 血清FGF21水平检测
使用酶联免疫吸附试验试剂盒(Antibody and Immunoassay Services,中国香港)[16]检测受试者的血清FGF21水平,具体操作按照试剂盒说明书进行。该试剂盒可检测到FGF21的最低浓度为30 pg/mL,批次内和批次间差异分别为5.41%和5.79%。
1.3 统计学方法
使用SPSS 25.0版软件进行统计分析。正态分布的定量资料以x±s表示,非正态分布的定量资料以M(Q1,Q3)表示,组间比较均采用单因素方差分析,其中非正态分布资料在分析之前需先行对数转换。定性资料以频数表示,组间比较采用χ2检验,在认知功能评估时先对性别、年龄进行校正,排除其对认知功能的影响。使用偏相关分析评估认知功能与人体测量学资料、实验室检测指标之间的关联。采用多元线性回归模型进一步探讨认知功能与人体测量学资料、实验室检测指标的相关性。P<0.05表示差异具有统计学意义。
2 结果
2.1 3组受试者资料比较
与正常体型组相比,超重组和肥胖组受试者的体脂肪量、体脂率、腰围、臀围、腰臀比、SBP、DBP以及FINS、UA、ALT、GGT水平呈现升高趋势(均P=0.000);肥胖组受试者的SBP、DBP及FPG、HbA1c、TAG水平高于正常体型组(均P<0.05),HDL-Ch水平低于正常体型组(P=0.045)。具体数据见表1。
表1 3组受试者一般资料和实验室检测指标比较
Tab 1
| Item | Normal weight group (n=50) | Overweight group (n=50) | Obese group (n=75) | P value |
|---|---|---|---|---|
| General information | ||||
| Age/year | 15.18 ± 0.48 | 15.52 ± 0.58 | 15.31 ± 0.52 | 0.327 |
| Gender (male/female)/n | 29/21 | 30/20 | 50/25 | 0.117 |
| BMI/(kg·m-2) | 21.35 ± 2.16 | 25.26 ± 0.98* | 30.37 ± 2.73*# | 0.000 |
| Body fat mass/kg | 12.73 ± 4.90 | 20.91 ± 4.69* | 29.95 ± 6.62*# | 0.000 |
| Body fat percentage/% | 20.93 ± 7.73 | 28.47 ± 7.21* | 33.55 ± 5.83*# | 0.000 |
| Waist circumference/cm | 73.95 ± 7.48 | 82.87 ± 3.69* | 95.53 ± 9.14*# | 0.000 |
| Hip circumference/cm | 94.70 ± 5.77 | 103.71 ± 3.80* | 110.09 ± 5.38*# | 0.000 |
| Waist-to-hip ratio | 0.80 ± 0.04 | 0.84 ± 0.01* | 0.89 ± 0.03*# | 0.000 |
| SBP/mmHg | 115.04 ± 12.27 | 120.29 ± 11.51 | 124.39 ± 9.98* | 0.000 |
| DBP/mmHg | 63.84 ± 7.42 | 69.09 ± 8.73* | 70.44 ± 9.27* | 0.000 |
| Laboratory testing indicator | ||||
| FPG/(mmol·L-1) | 4.62 ± 0.35 | 4.78 ± 0.30 | 4.79 ± 0.37* | 0.014 |
| FINS/(mmol·L-1) | 15.03 (11.43, 19.28) | 21.67 (17.62, 29.76)* | 29.94 (18.96, 38.32)*# | 0.000 |
| HbA1c/% | 5.31 ± 0.21 | 5.32 ± 0.16 | 5.42 ± 0.27* | 0.008 |
| Scr/(µmol·L-1) | 65.95 (58.40, 76.85) | 66.25 (56.33, 73.83)* | 71.90 (63.50, 79.50)* # | 0.052 |
| UA/(µmol·L-1) | 368.86 ± 85.19 | 397.66 ± 82.31 | 451.24 ± 102.53* | 0.000 |
| ALT/(U·L-1) | 14.00 (11.00, 17.25) | 17.50 (15.00, 27.00)* | 26.00 (20.00, 48.00)*# | 0.000 |
| AST/(U·L-1) | 21.00 (17.75, 24.00) | 21.00 (18.00, 26.25) | 26.00 (20.00, 32.00)* | 0.000 |
| GGT/(U·L-1) | 16.50 (14.00, 21.00) | 19.50 (14.75, 25.00) | 23.00 (17.00, 32.00)*# | 0.000 |
| TC/(mmol·L-1) | 4.36 ± 0.78 | 4.30 ± 0.76* | 4.33 ± 0.74*# | 0.880 |
| TAG/(mmol·L-1) | 0.74 (0.55, 1.04) | 0.87 (0.61, 1.29) | 0.92 (0.69, 1.37) | 0.012 |
| HDL-Ch/(mmol·L-1) | 1.44 ± 0.29 | 1.26 ± 0.26* | 1.21 ± 0.25* | 0.000 |
| LDL-Ch/(mmol·L-1) | 2.48 ± 0.70 | 2.56 ± 0.56 | 2.69 ± 0.69 | 0.076 |
2.2 受试者的认知功能评估
对3组受试者的性别、年龄是否影响其认知功能进行分析,结果发现,任意一组中的高一年级(15.0~16.5岁)与高二年级(16.5~18.0岁)青少年的ACC、反应时差异均无统计学意义;同时,175名青少年中男性与女性的该2个指标间差异亦无统计学意义。继而提示,年龄、性别对于青少年行为学试验的表现无影响。
ACC方面,3组受试者在Flanker任务、n-back任务中的差异均无统计学意义。反应时方面,3组受试者的表现则不同:① Flanker任务。在一致性刺激或不一致性刺激的条件下,肥胖组受试者的反应时长于正常体型组(P=0.000,P=0.002)且亦长于超重组(P=0.030,P=0.001);而正常体型组与超重组间差异均无统计学意义。② n-back任务。随着记忆负荷的增加,3组受试者的反应时均逐渐延长。随着肥胖程度的增加,受试者在0-back任务中的反应时延长;在1-back任务中,肥胖组受试者的反应时长于正常体型组(P=0.000);在2-back任务中,肥胖组受试者的反应时不仅长于正常体型组(P=0.000)还长于超重组(P=0.001)。具体数据见表2。
表2 3组受试者的认知功能评估
Tab 2
| Item | Normal weight group (n=50) | Overweight group (n=50) | Obese group (n=75) | P value |
|---|---|---|---|---|
| Flanker task | ||||
| ACC | ||||
| Congruent stimulus | 0.97 ± 0.09 | 0.97 ± 0.04 | 0.98 ± 0.04 | 0.442 |
| Incongruent stimulus | 0.92 ± 0.09 | 0.93 ± 0.10 | 0.92 ± 0.14 | 0.854 |
| Reaction time/ms | ||||
| Congruent stimulus | 406.12 ± 108.32 | 431.35 ± 85.17 | 475.13 ± 84.31 | 0.000 |
| Incongruent stimulus | 465.41 ± 95.59 | 463.55 ± 59.92 | 524.01 ± 103.79 | 0.000 |
| n-back task | ||||
| ACC | ||||
| 0-back | 0.94 ± 0.05 | 0.93 ± 0.07 | 0.93 ± 0.08 | 0.641 |
| 1-back | 0.84 ± 0.12 | 0.85 ± 0.08 | 0.86 ± 0.12 | 0.404 |
| 2-back | 0.78 ± 0.13 | 0.72 ± 0.16 | 0.78 ± 0.15 | 0.751 |
| Reaction time/ms | ||||
| 0-back | 522.52 ± 103.11 | 539.48 ± 104.85 | 564.34 ± 116.74 | 0.050 |
| 1-back | 541.76 ± 149.67 | 587.90 ± 160.04 | 656.60 ± 168.99 | 0.000 |
| 2-back | 570.49 ± 174.48 | 625.08 ± 199.08 | 754.24 ± 201.57 | 0.000 |
2.3 受试者行为学试验表现与其人体测量学资料、实验室检测指标的关系
在校正了性别、年龄后,我们采用偏相关分析对受试者的认知功能与其人体测量学资料、实验室检测指标的相关性进行评估。① ACC方面,3组受试者在Flanker任务、n-back任务中的差异均无统计学意义。② 反应时方面,Flanker任务的结果(表3)显示,一致性刺激条件下受试者的反应时与其BMI、体脂肪量、体脂率、腰臀比、腰围、臀围相关(均P<0.05),不一致性刺激条件下其反应时仅与BMI、体脂肪量、腰臀比、腰围及Scr、UA水平相关(均P<0.05)。n-back任务的结果(表4)显示,1-back任务中,受试者的反应时与其BMI、体脂肪量、体脂率、腰臀比、腰围、臀围及ALT、AST、GGT、UA水平相关(均P<0.05);2-back任务中,受试者的反应时与其BMI、体脂肪量、体脂率、腰臀比、腰围、臀围及ALT、AST、UA水平相关(均P<0.05)。
表3 受试者在Flanker任务中的表现与其人体测量学资料、实验室检测指标的相关性[r (P)值]
Tab 3
| Item | ACC | Reaction time | ||
|---|---|---|---|---|
| Incongruent stimulus | Congruent stimulus | Incongruent stimulus | Congruent stimulus | |
| BMI | -0.004 (0.958) | 0.033 (0.678) | 0.259 (0.000) | 0.337 (0.000) |
| Body fat mass | 0.004 (0.963) | 0.014 (0.857) | 0.154 (0.045) | 0.242 (0.000) |
| Body fat percentage | -0.013 (0.874) | -0.024 (0.764) | 0.061 (0.431) | 0.193 (0.011) |
| Waist-to-hip ratio | 0.008 (0.928) | 0.054 (0.495) | 0.217 (0.004) | 0.280 (0.000) |
| Waist circumference | 0.007 (0.930) | -0.018 (0.820) | 0.156 (0.042) | 0.269 (0.000) |
| Hip circumference | -0.016 (0.848) | -0.027 (0.731) | 0.107 (0.162) | 0.238 (0.002) |
| SBP | 0.051 (0.538) | 0.006 (0.940) | 0.041 (0.596) | 0.109 (0.155) |
| DBP | -0.029 (0.729) | 0.034 (0.674) | -0.042 (0.581) | 0.058 (0.452) |
| FINS | -0.053 (0.523) | 0.030 (0.707) | 0.088 (0.250) | 0.132 (0.084) |
| HbA1c | -0.114 (0.168) | -0.037 (0.639) | 0.023 (0.765) | 0.110 (0.153) |
| FPG | 0.072 (0.387) | 0.012 (0.877) | -0.074 (0.336) | 0.032 (0.680) |
| ALT | -0.105 (0.204) | 0.041 (0.607) | 0.100 (0.191) | 0.142 (0.062) |
| AST | -0.099 (0.231) | 0.069 (0.384) | 0.115 (0.133) | 0.099 (0.194) |
| GGT | -0.095 (0.251) | 0.057 (0.473) | 0.088 (0.251) | 0.123 (0.107) |
| Scr | 0.075 (0.363) | 0.077 (0.335) | 0.219 (0.004) | 0.049 (0.521) |
| UA | -0.067 (0.420) | 0.035 (0.662) | 0.171 (0.025) | 0.139 (0.069) |
| TC | 0.026 (0.755) | -0.053 (0.508) | -0.015 (0.849) | -0.116 (0.130) |
| TAG | -0.112 (0.177) | -0.113 (0.154) | 0.002 (0.975) | -0.003 (0.973) |
| HDL-Ch | -0.014 (0.863) | 0.063 (0.425) | 0.014 (0.855) | -0.045 (0.556) |
| LDL-Ch | 0.042 (0.616) | -0.083 (0.293) | -0.005 (0.950) | -0.098 (0.202) |
表4 受试者在n-back任务中的表现与其人体测量学资料、实验室检测指标的相关性[r (P)值]
Tab 4
| Item | ACC | Reaction time | ||||
|---|---|---|---|---|---|---|
| 0-back | 1-back | 2-back | 0-back | 1-back | 2-back | |
| BMI | 0.032 (0.701) | 0.078 (0.344) | 0.087 (0.299) | 0.151 (0.069) | 0.268 (0.000) | 0.351 (0.000) |
| Body fat mass | 0.027 (0.745) | 0.057 (0.489) | 0.061 (0.465) | 0.124 (0.135) | 0.217 (0.004) | 0.282 (0.000) |
| Body fat percentage | 0.030 (0.722) | 0.042 (0.615) | 0.062 (0.459) | 0.065 (0.438) | 0.173 (0.023) | 0.240 (0.000) |
| Waist-to-hip ratio | 0.002 (0.983) | -0.022 (0.794) | 0.077 (0.357) | 0.095 (0.253) | 0.257 (0.000) | 0.320 (0.000) |
| Waist circumference | -0.058 (0.491) | 0.001 (0.986) | 0.008 (0.921) | 0.122 (0.143) | 0.200 (0.008) | 0.248 (0.000) |
| Hip circumference | -0.040 (0.635) | 0.062 (0.454) | 0.044 (0.602) | 0.082 (0.328) | 0.208 (0.006) | 0.257 (0.000) |
| SBP | -0.051 (0.544) | 0.012 (0.887) | 0.101 (0.227) | -0.004 (0.961) | 0.107 (0.164) | 0.101 (0.186) |
| DBP | -0.099 (0.238) | -0.079 (0.344) | -0.056 (0.500) | 0.059 (0.482) | 0.137 (0.074) | 0.059 (0.443) |
| FINS | -0.042 (0.612) | -0.085 (0.303) | -0.080 (0.339) | 0.013 (0.872) | 0.116 (0.128) | 0.138 (0.070) |
| HbA1c | -0.028 (0.738) | -0.149 (0.071) | -0.085 (0.308) | 0.001 (0.988) | 0.103 (0.177) | 0.055 (0.473) |
| FPG | -0.176 (0.035) | -0.114 (0.169) | -0.036 (0.666) | -0.139 (0.095) | -0.021 (0.790) | 0.025 (0.741) |
| ALT | -0.067 (0.420) | -0.046 (0.580) | -0.067 (0.425) | 0.046 (0.579) | 0.161 (0.035) | 0.207 (0.006) |
| AST | -0.008 (0.923) | -0.042 (0.614) | -0.060 (0.469) | 0.045 (0.591) | 0.156 (0.040) | 0.199 (0.009) |
| GGT | 0.061 (0.464) | -0.068 (0.413) | -0.148 (0.075) | 0.017 (0.835) | 0.161 (0.034) | 0.139 (0.068) |
| Scr | -0.050 (0.546) | -0.173 (0.035) | -0.021 (0.798) | 0.032 (0.700) | 0.085 (0.264) | 0.101 (0.188) |
| UA | 0.032 (0.698) | -0.093 (0.260) | -0.140 (0.093) | 0.158 (0.057) | 0.227 (0.003) | 0.310 (0.000) |
| TC | 0.182 (0.028) | -0.016 (0.850) | -0.059 (0.483) | -0.037 (0.656) | 0.029 (0.709) | -0.028 (0.719) |
| TAG | 0.051 (0.539) | -0.092 (0.267) | -0.223 (0.007) | 0.058 (0.488) | 0.027 (0.722) | 0.026 (0.732) |
| HDL-Ch | 0.075 (0.366) | 0.011 (0.893) | 0.098 (0.240) | 0.042 (0.619) | -0.024 (0.752) | -0.116 (0.127) |
| LDL-Ch | 0.158 (0.058) | -0.010 (0.907) | -0.076 (0.364) | -0.058 (0.484) | 0.068 (0.371) | 0.036 (0.638) |
2.4 受试者反应时的影响因素的多元线性回归分析
随后,本研究采用多元线性回归模型对受试者在行为学任务中的反应时行进一步分析。在Flanker任务中,以受试者在一致性刺激条件下的反应时作为因变量,将上述偏相关分析中有统计学意义的指标及具有临床意义的指标作为自变量纳入模型,结果显示BMI(P=0.000)与反应时延长相关;以受试者在不一致性刺激条件下的反应时作为因变量进行分析,结果显示BMI(P=0.000)、臀围(P=0.013)是反应时延长的影响因素。在n-back任务中,以受试者在1-back任务中的反应时为因变量,以上述偏相关分析中有统计学意义的指标及具有临床意义的指标为自变量,结果显示BMI(P=0.001)与1-back任务的反应时相关;以受试者在2-back任务中的反应时为因变量进行分析,结果显示BMI(P=0.000)亦是2-back任务反应时延长的影响因素。具体数据见表5。以上结果提示,BMI是Flanker、n-back任务中受试者反应时的影响因素。
表5 受试者反应时的影响因素的多元线性回归分析
Tab 5
| Variable | β | STD | t value | P value |
|---|---|---|---|---|
| Flanker task | ||||
| Incongruent stimulus | ||||
| BMI | 11.064 | 0.511 | 4.053 | 0.000 |
| Hip circumference | -3.664 | -0.315 | -2.499 | 0.013 |
| Congruent stimulus | ||||
| BMI | 6.468 | 0.295 | 4.043 | 0.000 |
| n-back task | ||||
| 1-back | ||||
| BMI | 9.505 | 0.250 | 3.378 | 0.001 |
| 2-back | ||||
| BMI | 15.045 | 0.317 | 4.368 | 0.000 |
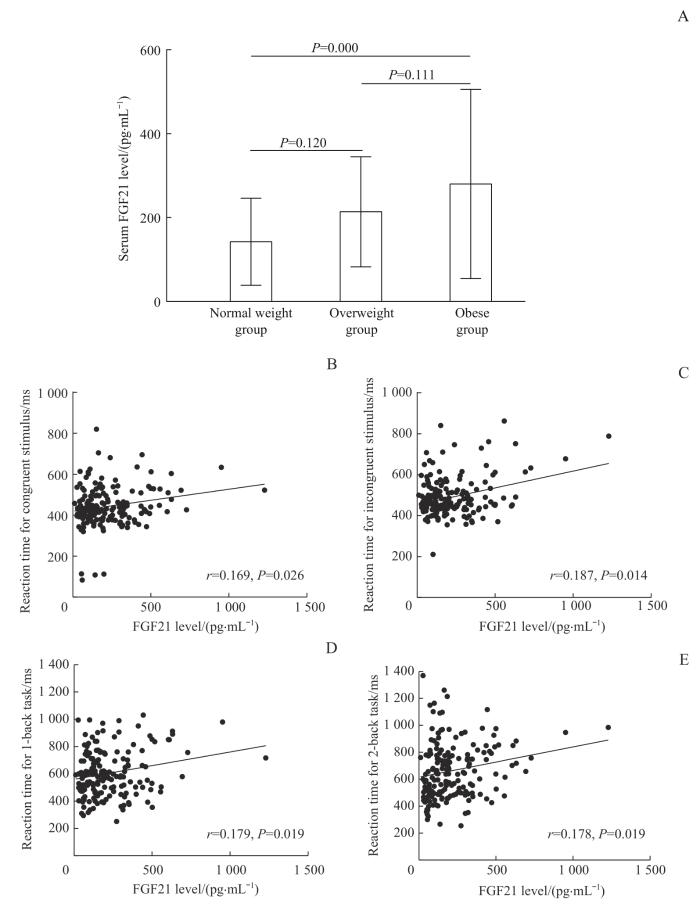
2.5 受试者血清FGF21水平与其行为学任务中表现的相关性分析
图2
图2
3组受试者血清FGF21水平比较及其与不同条件下反应时的相关性分析
Note:A. Comparison of serum FGF21 levels among the three groups of subjects. B/C. Correlation analysis between reaction time and serum FGF21 levels in subjects under congruent (B) or incongruent (C) stimulus conditions. D/E. Correlation analysis between reaction time and serum FGF21 levels in subjects with 1-back task (D) or 2-back task (E).
Fig 2
Comparison of serum FGF21 levels among the three groups of subjects and its correlation analysis with reaction time under different conditions
而后,以血清FGF21水平作为因变量,将认知功能相关指标作为自变量开展多元线性回归分析,结果(表6)显示,受试者在2-back任务中的ACC(P=0.000)、不一致刺激条件下的反应时(P=0.048)是其血清FGF21水平的独立影响因素。
表6 受试者认知功能相关指标与血清FGF21水平的多元线性回归分析
Tab 6
| Variable | β | STD | t value | P value | adjusted R² |
|---|---|---|---|---|---|
| 2-back ACC | -2.090 | -0.334 | -3.687 | 0.000 | 0.110 |
| Reaction time for incongruent stimulus | 0.002 | 0.182 | 2.004 | 0.048 |
3 讨论
本研究的结果显示,肥胖组青少年在基本及高阶认知功能、工作记忆中的反应时均显著长于正常体型组;受试者的BMI与其在基本及高阶认知功能、工作记忆中的反应时皆呈正相关,且BMI是Flanker任务、n-back任务中反应时延长的影响因素。此外,与其他2组相比,肥胖组青少年的血清FGF21水平均较高,且与Flanker任务、n-back任务中反应时显著相关。
既往研究[17]采用行为学试验与神经电学对青春期前儿童肥胖与认知冲突的加工能力之间的关系进行评估,结果显示在Flanker任务的不一致性刺激下,肥胖儿童的反应时显著长于健康体质量儿童,提示儿童肥胖可降低其认知冲突的加工能力。相关神经心理测试研究[4]对肥胖组、健康对照组青少年在CNSVS测试中的8项指标得分进行比较,结果发现肥胖组青少年在所有认知领域的平均得分均显著低于对照组,表明肥胖对青少年认知功能的多个方面均有损伤。本研究结果显示,与正常体型组相比,Flanker任务中肥胖组青少年在一致或不一致性刺激条件下的反应时均有显著延长,即肥胖青少年在基本与高阶认知功能层面的表现均差于正常体型组,这也可表明肥胖对青少年认知功能造成了较广泛的负面影响。既往针对肥胖青少年工作记忆的研究相对较少,其中一项针对肥胖青少年代谢手术的研究[18]发现体质量减轻与前额叶激活的减少相关,表明肥胖青少年的认知功能改变与代谢变化的神经可塑性相关。本研究发现,肥胖青少年在1-back和2-back任务中的反应时均显著长于正常体型组,表明肥胖青少年的即时记忆与延迟记忆功能均有下降。有研究[19]表明肥胖会导致全身脂肪组织堆积及相关细胞因子、炎症因子分泌增加,继而使肥胖患者处于全身炎症状态;其中TAG被认为可部分介导肥胖对认知功能的影响,如高水平的TAG能够阻碍瘦素、FGF21等透过血脑屏障,进而对神经系统产生不利影响,最终导致认知失调。也有研究[20]认为,神经递质多巴胺可能是导致肥胖个体与正常个体认知功能产生差异的原因。目前,有关肥胖青少年认知功能的改变尚需要进一步的研究,同时还需要更精确的方法(如氢质子磁共振波谱、弥散张量成像、静息态脑功能磁共振成像等新兴磁共振技术)对认知功能加以评估。
临床研究[21]表明,肥胖、高脂饮食与学习、记忆和执行功能缺陷以及潜在的脑萎缩相关。近期的一项研究[22]从流行病学的角度揭示过度肥胖是认知功能下降的关键代谢风险因素,而减少过量的内脏脂肪、降低腰臀比能够有效改善认知功能,提高思维能力、学习能力和记忆力。肥胖动物模型的研究[23]发现,高脂喂养的小鼠由于肝脏脂肪变性、巨噬细胞浸润和胰岛素抵抗等,其海马区域会出现炎症损伤,最终致使小鼠发生记忆缺陷。同时,肥胖导致的全身炎症和中枢炎症可通过多种机制影响突触神经元的功能,最终导致肥胖患者认知功能的变化。此外,肥胖还会引起血脑屏障发生损伤。有研究[24]发现高脂喂养的大鼠与非肥胖大鼠相比会出现血脑屏障通透性增加及海马依赖性认知障碍。且动物研究[25]发现,血脑屏障损伤后血清源性物质可进入海马间隙以激活小胶质细胞,最终引起认知功能障碍。目前,肥胖相关的认知障碍发病机制尚未被完全阐明,需更加深入的研究探讨。
FGF21是一种主要表达于肝脏的激素样蛋白,可通过与靶器官中成纤维细胞生长因子受体(fibroblast growth factor receptor,FGFR)和共受体β-klotho形成复合物来激活下游信号,进而参与机体代谢并维持脂代谢和糖代谢稳态。既往研究[26]发现,肥胖患者的血清FGF21水平与正常体型人群相比显著升高,在中心性肥胖的非酒精性脂肪肝患者中该指标水平与肝脏脂肪含量呈正相关。这与本研究结果相一致,即肥胖组青少年的血清FGF21水平显著高于正常体型组。此外,相关研究[27]发现,与非肥胖小鼠相比,纯合的Lepob突变小鼠(ob/ob)、Leprdb突变小鼠(db/db)及饮食诱导的肥胖小鼠体内FGF21水平均显著升高,并伴随靶组织中FGFR和β-Klotho表达下降,继而提示小鼠存在FGF21抵抗状态。目前,FGF21已被证实可在大脑的新陈代谢、认知方面发挥重要作用。既往研究[14]显示,FGF21通过抑制微管相关蛋白tau和β-淀粉样蛋白的聚合,促进脑源性神经营养因子的表达,维持线粒体蛋白的稳定,并通过NF-κB(核因子κB)和AMPK/Akt(腺苷酸激活蛋白激酶/丝氨酸-苏氨酸激酶)信号通路调控炎症和氧化应激来减轻神经免疫损伤,从而抑制神经退行性改变。此外,FGF21还可以通过FGFR1/β-klotho上调过氧化物酶体增殖物活化受体γ来保护血脑屏障,降低炎症对认知功能的损伤[28]。鉴于中枢神经系统可能是FGF21治疗肥胖相关代谢异常的重要靶点,因此对FGF21在认知障碍中的作用研究具有较为重要的临床价值,或可为肥胖相关认知障碍的诊治过程提供新的思路。
综上所述,本研究通过行为学试验综合评估了超重、肥胖青少年的认知功能,发现在青少年肥胖阶段已存在认知功能障碍,其中BMI是青少年认知功能改变的影响因素,且认知功能与BMI、FGF21水平显著相关。研究结果为进一步探讨肥胖青少年认知改变的机制研究提供了新的方向。
作者贡献声明
韩瑞、吴倩、倪嘉成、康飘、陈安然参与了数据采集,韩瑞、刘丹负责数据分析,韩瑞负责论文的写作和修改,张盈、于淑洁、程棣参与了文献检索,方启晨、李华婷负责数据分析指导和论文审阅。所有作者均阅读并同意了最终稿件的提交。
AUTHOR's CONTRIBUTIONS
HAN Rui, WU Qian, NI Jiacheng, KANG Piao and CHEN Anran participated in data collection. HAN Rui and LIU Dan were responsible for data analysis. HAN Rui was responsible for writing and revising the paper. ZHANG Ying, YU Shujie and CHENG Di participated in literature retrieval. FANG Qichen and LI Huating were responsible for data analysis and guidance and paper review. All the authors have read the last version of paper and consented for submission.
利益冲突声明
所有作者声明不存在利益冲突。
COMPETING INTERESTS
All authors disclose no relevant conflict of interests.
参考文献