
上海交通大学学报(医学版) ›› 2024, Vol. 44 ›› Issue (5): 606-616.doi: 10.3969/j.issn.1674-8115.2024.05.009
• 论著 · 循证医学 • 上一篇
收稿日期:2023-11-08
接受日期:2024-02-23
出版日期:2024-05-28
发布日期:2024-05-28
通讯作者:
方贻儒,彭代辉
E-mail:1185161632@qq.com;yirufang@aliyun.com;pdhsh@126.com
作者简介:孙晨寅(1998—),女,硕士生;电子信箱:1185161632@qq.com。
基金资助:
SUN Chenyin( ), WU Baichuan, ZHANG Huifeng, FANG Yiru(
), WU Baichuan, ZHANG Huifeng, FANG Yiru( ), PENG Daihui(
), PENG Daihui( )
)
Received:2023-11-08
Accepted:2024-02-23
Online:2024-05-28
Published:2024-05-28
Contact:
FANG Yiru,PENG Daihui
E-mail:1185161632@qq.com;yirufang@aliyun.com;pdhsh@126.com
Supported by:摘要:
目的·系统评价体动记录仪对于抑郁症患者昼夜节律特征的评估效果。方法·检索PubMed、Embase、Web of Science、Cochrane Library、PsycINFO、中国知网(CNKI)、万方数据知识服务平台(WanFang)、中国生物医学文献数据库(Chinese biomedical literature database,CBM),检索文献发表时间为从各数据库建库开始至2023年05月05日,收集使用体动记录仪评估抑郁症患者的昼夜节律并与健康对照进行比较的横断面研究。由2名研究者根据纳入与排除标准独立筛选文献,并采用Newcastle-Ottawa Scale(NOS)文献质量评价量表对纳入的文献进行质量评价,最后使用RevMan5.4软件进行meta分析。结果·共纳入9篇文献,包括抑郁症患者390名,健康对照288名。Meta分析结果显示,抑郁症患者昼夜节律余弦函数的中值(midline statistic of rhythm,MESOR)(SMD=-0.29,95% CI -0.51~-0.07,P=0.009)小于健康对照;抑郁症患者的入睡时间(sleep onset)(MD=33.06,95% CI 14.90~51.23,P=0.000)和觉醒时间(sleep offset)(MD=53.80,95% CI 22.38~85.23,P=0.000)晚于健康对照;抑郁症患者和健康对照1 d中最活跃的10 h的活动量(activity during the 10 most active hours,M10)(SMD=-0.26,95% CI -0.52~0.01,P=0.060)间差异无统计学意义,但抑郁症患者的活动量有小于健康对照的趋势;抑郁症患者和健康对照昼夜节律余弦函数的峰值相位(acrophase)(MD=25.33,95% CI -12.41~63.06,P=0.190)间差异无统计学意义;抑郁症患者和健康对照昼夜节律余弦函数的振幅(amplitude)(SMD=-0.14,95% CI -0.42~0.14,P=0.340)以及1 d中最不活跃的5 h的活动量(activity during the 5 least active hours,L5)(SMD=0.31,95% CI -0.10~0.71,P=0.140)间差异的统计学意义并不明确。结论·体动记录仪能够在一定程度上反映抑郁症患者的昼夜节律紊乱,但因纳入研究数量有限,研究人群及方法不一致,对分析质量和结果产生了一定影响,需要更多高质量的临床试验提供证据。
中图分类号:
孙晨寅, 吴百川, 张慧凤, 方贻儒, 彭代辉. 体动记录仪评估抑郁症昼夜节律:一项系统综述和meta分析[J]. 上海交通大学学报(医学版), 2024, 44(5): 606-616.
SUN Chenyin, WU Baichuan, ZHANG Huifeng, FANG Yiru, PENG Daihui. Evaluation of circadian rhythms in depression by using actigraphy: a systematic review and meta-analysis[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2024, 44(5): 606-616.
| Study | Research area | Depression | Control | Actigraphy | Outcome | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample size/n | Age/year | Sex (male/female)/n | Diagnostic criteria | Sample size/n | Age/year | Sex (male/female)/n | Instrument model | Wearing time/d | |||
ROBILLARD, 2015[ | Australia | 135 | 20.0±4.4 | 47/88 | DSM | 41 | 25.3±5.8 | 19/22 | Actiwatch-64/L/2, Philips Respironics | 4‒22 | ①③⑥⑦ |
| MERIKANTO, 2017[ | Finland | 8 | 16.0±1.1 | 8/0 | K-SADS-PL | 9 | 16.0±0.7 | 9/0 | Actiwatch-Plus®, Cambridge Neurotechnology Ltd, Cambridge, UK | 23 | ①④⑤ |
| SLYEPCHENKO, 2019[ | Canada | 38 | 39 (22.75) | 13/25 | MINI | 40 | 30 (20) | 20/20 | Actiwatch 2 monitor | 15 | ①②③④⑤ |
| MINAEVA, 2020[ | The Netherlands | 58 | 52.34±10.59 | 22/36 | CIDI | 63 | 51.94±12.05 | 34/29 | GENEActiv actigraphy | 14 | ①②③ |
| PYE, 2021[ | Australia | 27 | 62.7±8.1 | 8/19 | MINI | 47 | 63.1±8.1 | 19/28 | Respironics Actiwatch Spectrum | 14 | ①②③④⑤⑥⑦ |
| TONON, 2022[ | Brazil | 39 | 16.1±0.7 | 19/20 | K-SADS-PL | 26 | 15.4±0.8 | 16/10 | ActTrust Condor | 10 | ②③④⑤⑥⑦ |
| ROBILLARD, 2013[ | Australia | 46 | 20.1±4.7 | 17/29 | DSM-IV | 20 | 24.8±2.5 | 8/12 | Actiwatch64, Philips Respironics, OR | 7 | ⑥⑦ |
| ROBILLARD, 2018[ | Australia | 35 | 21.1±2.9 | 14/21 | DSM-IV | 15 | 24.3±3.4 | 7/8 | Actiwatch64/L/2, Philips Respironics, USA or GENEActiv, Activinsights, UK | 12 | ⑥⑦ |
| MCGLASHAN, 2019[ | Australia | 8 | 24.25±2.12 | 0/8 | DSM-IV-TR | 31 | 21.19±2.65 | 0/31 | Actiwatch Spectrum, PLUS, PRO, 2 or L, Philips Respironics, OR, USA | 7 | ⑥⑦ |
表1 纳入文献的基本特征
Tab 1 Basic characteristics of the included studies
| Study | Research area | Depression | Control | Actigraphy | Outcome | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample size/n | Age/year | Sex (male/female)/n | Diagnostic criteria | Sample size/n | Age/year | Sex (male/female)/n | Instrument model | Wearing time/d | |||
ROBILLARD, 2015[ | Australia | 135 | 20.0±4.4 | 47/88 | DSM | 41 | 25.3±5.8 | 19/22 | Actiwatch-64/L/2, Philips Respironics | 4‒22 | ①③⑥⑦ |
| MERIKANTO, 2017[ | Finland | 8 | 16.0±1.1 | 8/0 | K-SADS-PL | 9 | 16.0±0.7 | 9/0 | Actiwatch-Plus®, Cambridge Neurotechnology Ltd, Cambridge, UK | 23 | ①④⑤ |
| SLYEPCHENKO, 2019[ | Canada | 38 | 39 (22.75) | 13/25 | MINI | 40 | 30 (20) | 20/20 | Actiwatch 2 monitor | 15 | ①②③④⑤ |
| MINAEVA, 2020[ | The Netherlands | 58 | 52.34±10.59 | 22/36 | CIDI | 63 | 51.94±12.05 | 34/29 | GENEActiv actigraphy | 14 | ①②③ |
| PYE, 2021[ | Australia | 27 | 62.7±8.1 | 8/19 | MINI | 47 | 63.1±8.1 | 19/28 | Respironics Actiwatch Spectrum | 14 | ①②③④⑤⑥⑦ |
| TONON, 2022[ | Brazil | 39 | 16.1±0.7 | 19/20 | K-SADS-PL | 26 | 15.4±0.8 | 16/10 | ActTrust Condor | 10 | ②③④⑤⑥⑦ |
| ROBILLARD, 2013[ | Australia | 46 | 20.1±4.7 | 17/29 | DSM-IV | 20 | 24.8±2.5 | 8/12 | Actiwatch64, Philips Respironics, OR | 7 | ⑥⑦ |
| ROBILLARD, 2018[ | Australia | 35 | 21.1±2.9 | 14/21 | DSM-IV | 15 | 24.3±3.4 | 7/8 | Actiwatch64/L/2, Philips Respironics, USA or GENEActiv, Activinsights, UK | 12 | ⑥⑦ |
| MCGLASHAN, 2019[ | Australia | 8 | 24.25±2.12 | 0/8 | DSM-IV-TR | 31 | 21.19±2.65 | 0/31 | Actiwatch Spectrum, PLUS, PRO, 2 or L, Philips Respironics, OR, USA | 7 | ⑥⑦ |
| Study | Selection | Comparability | Outcome | Quality score | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ① | ② | ③ | ④ | ① | ② | ① | ② | ③ | ||
| ROBILLARD, 2015[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 |
| MERIKANTO, 2017[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 |
| SLYEPCHENKO, 2019[ | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 |
| MINAEVA, 2020[ | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| PYE, 2021[ | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 6 |
| TONON, 2022[ | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 6 |
| ROBILLARD, 2013[ | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| ROBILLARD, 2018[ | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 7 |
| MCGLASHAN, 2019[ | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 6 |
表2 纳入文献的质量评价结果
Tab 2 Quality assessment of the included studies
| Study | Selection | Comparability | Outcome | Quality score | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ① | ② | ③ | ④ | ① | ② | ① | ② | ③ | ||
| ROBILLARD, 2015[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 |
| MERIKANTO, 2017[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 |
| SLYEPCHENKO, 2019[ | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 |
| MINAEVA, 2020[ | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| PYE, 2021[ | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 6 |
| TONON, 2022[ | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 6 |
| ROBILLARD, 2013[ | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| ROBILLARD, 2018[ | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 7 |
| MCGLASHAN, 2019[ | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 6 |
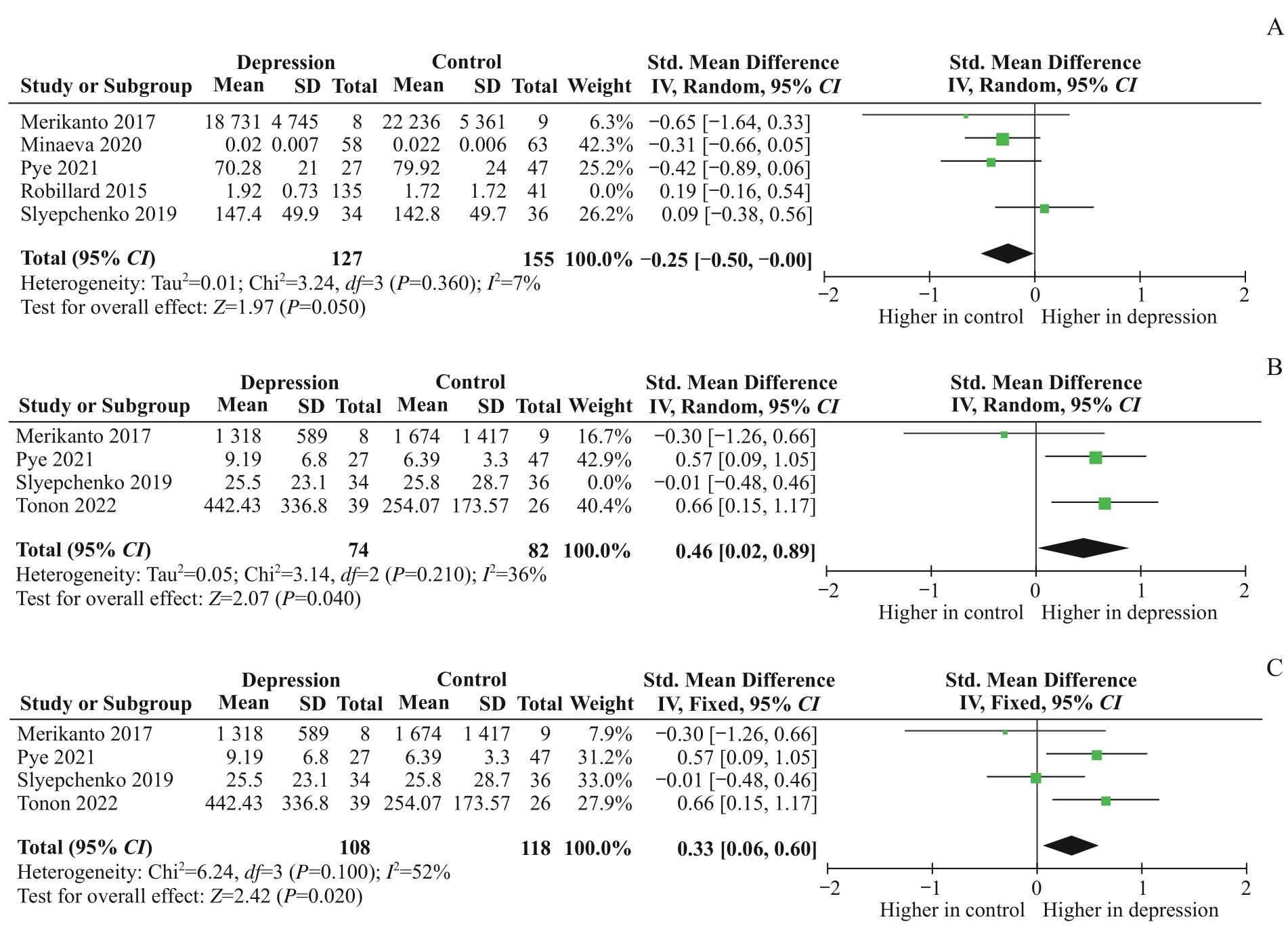
图9 敏感度分析森林图Note: A. Forest plot for sensitivity analysis of amplitude. B. Forest plot for sensitivity analysis of L5 (excluding studies). C. Forest plot for sensitivity analysis of L5 (changing statistical models).
Fig 9 Forest plot for sensitivity analysis
| 1 | JONES S G, BENCA R M. Circadian disruption in psychiatric disorders[J]. Sleep Med Clin, 2015, 10(4): 481-493. |
| 2 | LOGAN R W, MCCLUNG C A. Rhythms of life: circadian disruption and brain disorders across the lifespan[J]. Nat Rev Neurosci, 2019, 20(1): 49-65. |
| 3 | WALKER W H 2nd, WALTON J C, DEVRIES A C, et al. Circadian rhythm disruption and mental health[J]. Transl Psychiatry, 2020, 10(1): 28. |
| 4 | FISHBEIN A B, KNUTSON K L, ZEE P C. Circadian disruption and human health[J]. J Clin Invest, 2021, 131(19): e148286. |
| 5 | DUARTE FARIA A, CARDOSO T D, CAMPOS MONDIN T, et al. Biological rhythms in bipolar and depressive disorders: a community study with drug-naïve young adults[J]. J Affect Disord, 2015, 186: 145-148. |
| 6 | MONDIN T C, CARDOSO T A, SOUZA L D M, et al. Mood disorders and biological rhythms in young adults: a large population-based study[J]. J Psychiatr Res, 2017, 84: 98-104. |
| 7 | OZCELIK M, SAHBAZ C. Clinical evaluation of biological rhythm domains in patients with major depression[J]. Braz J Psychiatry, 2020, 42(3): 258-263. |
| 8 | MURRAY G. Diurnal mood variation in depression: a signal of disturbed circadian function?[J]. J Affect Disord, 2007, 102(1/2/3): 47-53. |
| 9 | COURTET P, OLIÉ E. Circadian dimension and severity of depression[J]. Eur Neuropsychopharmacol, 2012, 22(Suppl 3): S476-S481. |
| 10 | DIFRANCESCO S, LAMERS F, RIESE H, et al. Sleep, circadian rhythm, and physical activity patterns in depressive and anxiety disorders: a 2-week ambulatory assessment study[J]. Depress Anxiety, 2019, 36(10): 975-986. |
| 11 | TAZAWA Y, WADA M, MITSUKURA Y, et al. Actigraphy for evaluation of mood disorders: a systematic review and meta-analysis[J]. J Affect Disord, 2019, 253: 257-269. |
| 12 | BURTON C, MCKINSTRY B, SZENTAGOTAI TĂTAR A, et al. Activity monitoring in patients with depression: a systematic review[J]. J Affect Disord, 2013, 145(1): 21-28. |
| 13 | WÜTHRICH F, NABB C B, MITTAL V A, et al. Actigraphically measured psychomotor slowing in depression: systematic review and meta-analysis[J]. Psychol Med, 2022, 52(7): 1208-1221. |
| 14 | CORNELISSEN G. Cosinor-based rhythmometry[J]. Theor Biol Med Model, 2014, 11: 16. |
| 15 | HIGGINS J P T, THOMAS J, CHANDLER J, et al. Cochrane handbook for systematic reviews of interventions[M]. 2nd ed. Chichester: John Wiley & Sons, 2019. |
| 16 | WAN X, WANG W Q, LIU J M, et al. Estimating the sample mean and standard deviation from the sample size, Median, range and/or interquartile range[J]. BMC Med Res Methodol, 2014, 14: 135. |
| 17 | ROBILLARD R, HERMENS D F, NAISMITH S L, et al. Ambulatory sleep-wake patterns and variability in young people with emerging mental disorders[J]. J Psychiatry Neurosci, 2015, 40(1): 28-37. |
| 18 | MERIKANTO I, PARTONEN T, PAUNIO T, et al. Advanced phases and reduced amplitudes are suggested to characterize the daily rest-activity cycles in depressed adolescent boys[J]. Chronobiol Int, 2017, 34(7): 967-976. |
| 19 | SLYEPCHENKO A, ALLEGA O R, LENG X M, et al. Association of functioning and quality of life with objective and subjective measures of sleep and biological rhythms in major depressive and bipolar disorder[J]. Aust N Z J Psychiatry, 2019, 53(7): 683-696. |
| 20 | MINAEVA O, BOOIJ S H, LAMERS F, et al. Level and timing of physical activity during normal daily life in depressed and non-depressed individuals[J]. Transl Psychiatry, 2020, 10(1): 259. |
| 21 | PYE J, PHILLIPS A J, CAIN S W, et al. Irregular sleep-wake patterns in older adults with current or remitted depression[J]. J Affect Disord, 2021, 281: 431-437. |
| 22 | TONON A C, CONSTANTINO D B, AMANDO G R, et al. Sleep disturbances, circadian activity, and nocturnal light exposure characterize high risk for and current depression in adolescence[J]. Sleep, 2022, 45(7): zsac104. |
| 23 | ROBILLARD R, NAISMITH S L, ROGERS N L, et al. Delayed sleep phase in young people with unipolar or bipolar affective disorders[J]. J Affect Disord, 2013, 145(2): 260-263. |
| 24 | ROBILLARD R, CARPENTER J S, ROGERS N L, et al. Circadian rhythms and psychiatric profiles in young adults with unipolar depressive disorders[J]. Transl Psychiatry, 2018, 8(1): 213. |
| 25 | MCGLASHAN E M, COLEMAN M Y, VIDAFAR P, et al. Decreased sensitivity of the circadian system to light in current, but not remitted depression[J]. J Affect Disord, 2019, 256: 386-392. |
| 26 | 张天嵩. 经典meta分析统计模型的合理选择[J]. 中国循证医学杂志, 2020, 20(12): 1477-1481. |
| ZHANG T S. The selection of appropriate statistical models for traditional meta-analysis[J]. Chinese Journal of Evidence-Based Medicine, 2020, 20(12): 1477-1481. | |
| 27 | 张天嵩. 传统meta分析统计模型的合理使用[J]. 中国医院统计, 2023, 30(4): 299-303, 308. |
| ZHANG T S. Rational use of statistical models for traditional meta-analysis[J]. Chinese Journal of Hospital Statistics, 2023, 30(4): 299-303, 308. | |
| 28 | ALLADA R, BASS J. Circadian mechanisms in medicine[J]. N Engl J Med, 2021, 384(6): 550-561. |
| 29 | CARPENTER J S, CROUSE J J, SCOTT E M, et al. Circadian depression: a mood disorder phenotype[J]. Neurosci Biobehav Rev, 2021, 126: 79-101. |
| 30 | CROUSE J J, CARPENTER J S, SONG Y J C, et al. Circadian rhythm sleep-wake disturbances and depression in young people: implications for prevention and early intervention[J]. Lancet Psychiatry, 2021, 8(9): 813-823. |
| 31 | MELHUISH BEAUPRE L, BROWN G M, KENNEDY J L. Circadian genes in major depressive disorder[J]. World J Biol Psychiatry, 2020, 21(2): 80-90. |
| 32 | TONON A C, PILZ L K, MARKUS R P, et al. Melatonin and depression: a translational perspective from animal models to clinical studies[J]. Front Psychiatry, 2021, 12: 638981. |
| 33 | MENDOZA J. Circadian insights into the biology of depression: symptoms, treatments and animal models[J]. Behav Brain Res, 2019, 376: 112186. |
| 34 | DAUT R A, FONKEN L K. Circadian regulation of depression: a role for serotonin[J]. Front Neuroendocrinol, 2019, 54: 100746. |
| 35 | SCHUCH F, VANCAMPFORT D, FIRTH J, et al. Physical activity and sedentary behavior in people with major depressive disorder: a systematic review and meta-analysis[J]. J Affect Disord, 2017, 210: 139-150. |
| 36 | HASLER B P, BUYSSE D J, KUPFER D J, et al. Phase relationships between core body temperature, melatonin, and sleep are associated with depression severity: further evidence for circadian misalignment in non-seasonal depression[J]. Psychiatry Res, 2010, 178(1): 205-207. |
| 37 | GHANEAN H, CENITI A K, KENNEDY S H. Fatigue in patients with major depressive disorder: prevalence, burden and pharmacological approaches to management[J]. CNS Drugs, 2018, 32(1): 65-74. |
| 38 | GIANFREDI V, FERRARA P, PENNISI F, et al. Association between daily pattern of physical activity and depression: a systematic review[J]. Int J Environ Res Public Health, 2022, 19(11): 6505. |
| 39 | RIEMANN D, KRONE L B, WULFF K, et al. Sleep, insomnia, and depression[J]. Neuropsychopharmacology, 2020, 45(1): 74-89. |
| 40 | HAGENAUER M H, PERRYMAN J I, LEE T M, et al. Adolescent changes in the homeostatic and circadian regulation of sleep[J]. Dev Neurosci, 2009, 31(4): 276-284. |
| 41 | HICKIE I, CARPENTER J, ROBILLARD R. Variations in the sleep-wake cycle from childhood to adulthood: chronobiological perspectives[J]. ChronoPhysiology Ther, 2015: 37. |
| 42 | TAKAESU Y, KANDA, NAGAHAMA Y, et al. Delayed sleep-wake rhythm is associated with cognitive dysfunction, social dysfunction, and deteriorated quality of life in patients with major depressive disorder[J]. Front Psychiatry, 2022, 13: 1022144. |
| 43 | CHAN J W, LAM S P, LI S X, et al. Eveningness and insomnia: independent risk factors of nonremission in major depressive disorder[J]. Sleep, 2014, 37(5): 911-917. |
| 44 | HORI H, KOGA N, HIDESE S, et al. 24-h activity rhythm and sleep in depressed outpatients[J]. J Psychiatr Res, 2016, 77: 27-34. |
| 45 | BAGLIONI C, NANOVSKA S, REGEN W, et al. Sleep and mental disorders: a meta-analysis of polysomnographic research[J]. Psychol Bull, 2016, 142(9): 969-990. |
| 46 | ANGEL V D, LEWIS S, WHITE K, et al. Digital health tools for the passive monitoring of depression: a systematic review of methods[J]. NPJ Digit Med, 2022, 5(1): 3. |
| 47 | MAATOUG R, OUDIN A, ADRIEN V, et al. Digital phenotype of mood disorders: a conceptual and critical review[J]. Front Psychiatry, 2022, 13: 895860. |
| 48 | ALI F Z, PARSEY R V, LIN S, et al. Circadian rhythm biomarker from wearable device data is related to concurrent antidepressant treatment response[J]. NPJ Digit Med, 2023, 6(1): 81. |
| 49 | XAVIER N B, ABREU A C V O, AMANDO G R, et al. Chronobiological parameters as predictors of early treatment response in major depression[J]. J Affect Disord, 2023, 323: 679-688. |
| 50 | DUNCAN W C Jr, SLONENA E, HEJAZI N S, et al. Motor-activity markers of circadian timekeeping are related to ketamine′s rapid antidepressant properties[J]. Biol Psychiatry, 2017, 82(5): 361-369. |
| 51 | WINKLER D, PJREK E, LANZENBERGER R, et al. Actigraphy in patients with treatment-resistant depression undergoing electroconvulsive therapy[J]. J Psychiatr Res, 2014, 57: 96-100. |
| [1] | 傅艺玲, 吴茜, 罗晓庆, 吴艾泓, 夏雪兰, 郑敏. 晚期癌症患者预立医疗照护计划参与行为影响因素的系统综述[J]. 上海交通大学学报(医学版), 2024, 44(4): 482-493. |
| [2] | 杨瑞君, 吕书红, 刘志业, 张新, 刘志浩. 中国5省初中生视屏时间和饮食行为与抑郁症状的关联[J]. 上海交通大学学报(医学版), 2024, 44(3): 358-364. |
| [3] | 高怡青, 彭裕, 许华俊, 易红良, 关建, 殷善开. 全球阻塞性睡眠呼吸暂停指南质量评价[J]. 上海交通大学学报(医学版), 2024, 44(2): 237-249. |
| [4] | 杨越, 何开举, 宗家豪, 杨自逸, 吴向嵩, 龚伟. 细胞游离DNA在胆道癌诊断中的价值:一项meta分析[J]. 上海交通大学学报(医学版), 2023, 43(9): 1175-1185. |
| [5] | 马文琳, 林元杰, 金婷婷, 石薇, 蒋莉华, 赵莉. 初中生自我中心主义与非自杀性自伤的关系研究[J]. 上海交通大学学报(医学版), 2023, 43(8): 971-976. |
| [6] | 陈惠, 朱唯一, 姚屹瑾. 调整左旋甲状腺素治疗剂量对甲状腺功能减退孕妇母婴结局影响的meta分析[J]. 上海交通大学学报(医学版), 2023, 43(7): 906-915. |
| [7] | 马卓然, 袁安彩, 蒋惠如, 陈潇雨, 张薇, 卜军. 脂质蓄积指数与中国成年人高血压关系的meta分析[J]. 上海交通大学学报(医学版), 2023, 43(4): 466-473. |
| [8] | 梁妍景, 黄楚贤, 李红艳, 侯黎莉. 维生素E对放疗或化疗导致的口腔黏膜炎有效性的meta分析[J]. 上海交通大学学报(医学版), 2023, 43(2): 208-214. |
| [9] | 李偲媛, 和申, 李华芳. 重度抑郁症中自噬通路及其关键标志物的研究进展[J]. 上海交通大学学报(医学版), 2023, 43(10): 1324-1331. |
| [10] | 杨玲, 侯黎莉, 赵燕, 陈卫宏, 张金凤, 毛艳. 口腔癌患者张口受限患病率的meta分析[J]. 上海交通大学学报(医学版), 2023, 43(1): 61-69. |
| [11] | 方芳, 台瑞, 余倩, 章雅青. 预康复对胃肠道择期手术患者术后恢复效果的系统评价[J]. 上海交通大学学报(医学版), 2023, 43(1): 70-78. |
| [12] | 陈卫宏, 侯黎莉, 杨玲, 毛艳, 张金凤. 冷冻疗法预防头颈癌患者放射性口腔黏膜炎的meta分析[J]. 上海交通大学学报(医学版), 2022, 42(5): 635-645. |
| [13] | 吴侠霏, 方婕, 漆洪波, 余昕烊. 妊娠期糖尿病对C57BL/6J子代成年鼠神经精神功能的影响[J]. 上海交通大学学报(医学版), 2022, 42(4): 422-432. |
| [14] | 谭颖超, 杨珺玥, 王莉娜. 白细胞介素-1B-511C/T基因多态性与冠状动脉粥样硬化性心脏病关联的meta分析[J]. 上海交通大学学报(医学版), 2022, 42(2): 197-204. |
| [15] | 李欣, 范青. 机器学习在抑郁症患者面部特征研究中的应用进展[J]. 上海交通大学学报(医学版), 2022, 42(1): 124-129. |
| 阅读次数 | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
全文 1427
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
摘要 |
|
|||||||||||||||||||||||||||||||||||||||||||||||||