
上海交通大学学报(医学版) ›› 2022, Vol. 42 ›› Issue (5): 562-569.doi: 10.3969/j.issn.1674-8115.2022.05.002
收稿日期:2022-01-24
接受日期:2022-05-06
出版日期:2022-05-28
发布日期:2022-05-28
通讯作者:
刘琰,电子信箱:ly10515@rjh.com.cn。作者简介:董叫云(1976—),女,主管技师,学士;电子信箱:dongjiaoyun@hotmail.com基金资助:
DONG Jiaoyun( ), SONG Fei(
), SONG Fei( ), LU Shuliang, LIU Yan(
), LU Shuliang, LIU Yan( ), TIAN Ming(
), TIAN Ming( )
)
Received:2022-01-24
Accepted:2022-05-06
Online:2022-05-28
Published:2022-05-28
Contact:
LIU Yan, E-mail: ly10515@rjh.com.cn.Supported by:摘要:
目的·开发用于烧伤急救的、可快速降低皮肤温度并且对皮肤组织无刺激性的医疗用品——制冷喷雾剂和聚合物水凝胶。验证联合应用两者是否可快速阻断热源对皮肤组织的持续伤害,是否有利于创面的早期修复及降低烧伤创面的面积及深度。方法·将制冷液灌入高压罐中,评估制冷喷雾剂的制冷效果;制备水凝胶敷料,评估敷料的制冷时长;评估在大鼠背部皮肤连续使用制冷喷雾剂和水凝胶72 h后,对皮肤组织的刺激作用;建立大鼠烫伤模型,随机分为2组,每组6只,采用背部皮肤组织互相对比的方法,在烫伤区域使用制冷喷雾剂和水凝胶联合处理创面,分别与无处理组和自来水处理组做比较,24 h后评估烫伤部位的面积和创面炎症反应情况。结果·与普通自来水相比,15 %浓度的制冷喷雾剂的制冷效果最好,在3 min内,降温速度明显高于自来水对照组(P<0.05);水凝胶的冷却效果可维持8 h,可以在2 h内将70 ℃水的温度降至室温(22±2)℃,且水温全程低于对照组;2种材料对皮肤组织均无刺激性作用,未导致皮肤组织红斑、水肿等过敏反应。经制冷喷雾剂和水凝胶联合处理的烧伤创面,其焦痂面积显著减少,与无处理组及自来水处理组相比,均有统计学差异(P<0.05);H-E染色显示,与无处理组及自来水组相比较,联合应用制冷喷雾剂和水凝胶组的创面中,炎症细胞浸润的数量显著减少(P<0.05)。结论·制冷喷雾剂与聚合物水凝胶联合应用显示出良好的冷却效率,可减少焦痂面积、防止创面的不断加深及炎症细胞的聚集,有利于后期创面尽快愈合,且不会造成皮肤组织的过敏反应,可以作为烧伤患者急救管理的一种有效和方便的工具。
中图分类号:
董叫云, 宋菲, 陆树良, 刘琰, 田鸣. 制冷喷雾联合高分子水凝胶对急性烧伤创面的影响[J]. 上海交通大学学报(医学版), 2022, 42(5): 562-569.
DONG Jiaoyun, SONG Fei, LU Shuliang, LIU Yan, TIAN Ming. Effects of cryogen spray combined with polymeric hydrogel on acute burn wounds[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2022, 42(5): 562-569.
| Test | Skin response | Score |
|---|---|---|
| Erythema and eschar formation | No erythema | 0 |
| Very slight erythema (barely perceptible) | 1 | |
| Well-defined erythema | 2 | |
| Moderate to severe erythema | 3 | |
| Severe erythema (beet-redness) to slight eschar formation (injuries in depth) | 4 | |
| Edema formation | No edema | 0 |
| Very slight edema (barely perceptible) | 1 | |
| Slight edema (edges of area well-defined by definite raising) | 2 | |
| Moderate edema (raised approximately 1.0 mm) | 3 | |
| Severe edema (raised more than 1.0 mm and extending beyond exposure area) | 4 | |
| Total possible score for irritation | 8 | |
表1 皮肤刺激试验的分级值
Tab 1 Grading values for the skin irritation test
| Test | Skin response | Score |
|---|---|---|
| Erythema and eschar formation | No erythema | 0 |
| Very slight erythema (barely perceptible) | 1 | |
| Well-defined erythema | 2 | |
| Moderate to severe erythema | 3 | |
| Severe erythema (beet-redness) to slight eschar formation (injuries in depth) | 4 | |
| Edema formation | No edema | 0 |
| Very slight edema (barely perceptible) | 1 | |
| Slight edema (edges of area well-defined by definite raising) | 2 | |
| Moderate edema (raised approximately 1.0 mm) | 3 | |
| Severe edema (raised more than 1.0 mm and extending beyond exposure area) | 4 | |
| Total possible score for irritation | 8 | |
Mean skin irritation intensity score | Intensity grading value |
|---|---|
| 0‒<0.5 | No irritation |
| 0.5‒<2.0 | Sight irritation |
| 2.0‒<6.0 | Moderate irritation |
| 6.0‒<8.0 | Severe irritation |
表2 皮肤刺激强度分级值
Tab 2 Grading values for the skin irritation intensity
Mean skin irritation intensity score | Intensity grading value |
|---|---|
| 0‒<0.5 | No irritation |
| 0.5‒<2.0 | Sight irritation |
| 2.0‒<6.0 | Moderate irritation |
| 6.0‒<8.0 | Severe irritation |
| Formula | Cooling time/s | |||
|---|---|---|---|---|
| Repeat 1 | Repeat 2 | Repeat 3 | Average | |
| Ordinary tap water | 49.57 | 43.83 | 45.65 | 46.35 |
| 10% cryogen spray | 35.68 | 40.87 | 40.00 | 38.85 |
| 15% cryogen spray | 31.72 | 34.60 | 33.50 | 33.27 |
| 20% cryogen spray | 34.50 | 31.15 | 34.80 | 33.48 |
表3 不同浓度制冷喷雾剂和普通自来水干预后的冷却速度
Tab 3 The cooling rate of cryogen spray with different concentrations and ordinary tap water
| Formula | Cooling time/s | |||
|---|---|---|---|---|
| Repeat 1 | Repeat 2 | Repeat 3 | Average | |
| Ordinary tap water | 49.57 | 43.83 | 45.65 | 46.35 |
| 10% cryogen spray | 35.68 | 40.87 | 40.00 | 38.85 |
| 15% cryogen spray | 31.72 | 34.60 | 33.50 | 33.27 |
| 20% cryogen spray | 34.50 | 31.15 | 34.80 | 33.48 |
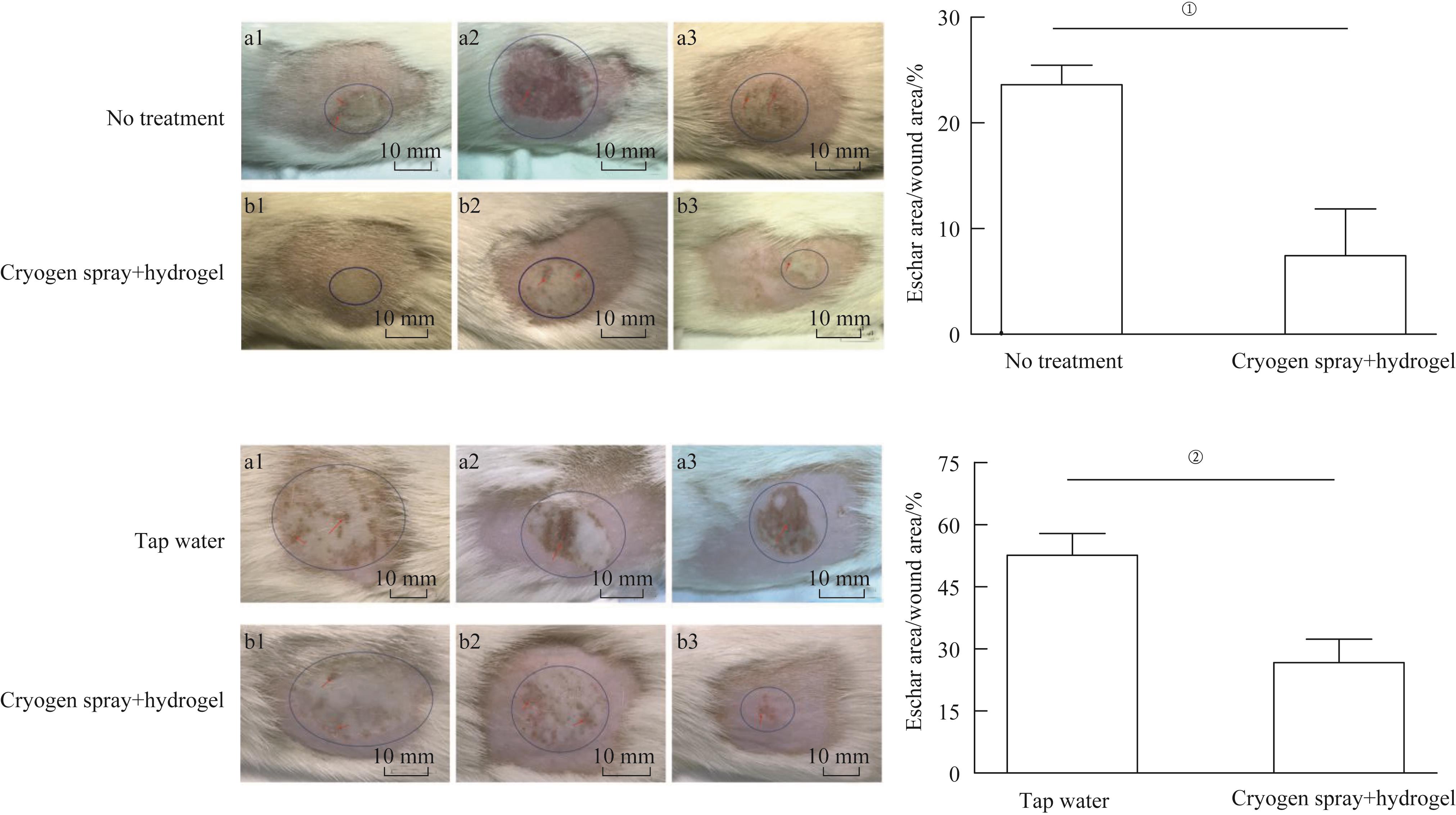
图6 制冷喷雾剂与水凝胶联合干预对受伤皮肤伤口面积和焦痂区域(红色箭头所示)的影响Note:①P=0.028;②P=0.029.
Fig 6 Effects of cryogen spray combined with hydrogel on the wound and eschar areas in the wounded skin

图7 制冷喷雾剂与水凝胶联合使用后受伤皮肤组织学表现(H-E染色,×20)Note:①P=0.003;②P=0.036.
Fig 7 Histological observation of the wounded skin treated by cryogen spray combined with hydrogel (H-E staining, ×20)
| 1 | WORLD HEALTH ORGANIZATION. Fact sheet burns[EB/OL]. 2018[2019-04-23]. https://www.who.int/news-room/fact-sheets/detail/burns. |
| 2 | SPRONK I, EDGAR D W, VAN B M E, et al. Improved and standardized method for assessing years lived with disability after burns and its application to estimate the non-fatal burden of disease of burn injuries in Australia, New Zealand and the Netherlands[J]. BMC Public Health, 2020, 20(1):121. |
| 3 | ABDEL HAMID A A M,SOLIMAN M F M. Effect of topical aloe vera on the process of healing of full-thickness skin burn: a histological and immunohistochemical study[J]. J Histol Histopathol, 2015, 2(1): 3. |
| 4 | CHENG W,WANG S,SHEN C, et al. Epidemiology of hospitalized burn patients in china: a systematic review[J]. Burns Open, 2018, 2(1): 8-16. |
| 5 | FINNERTY C C, JESCHKE M G, BRANSKI L K, et al. Hypertrophic scarring: the greatest unmet challenge after burn injury[J]. Lancet, 2016, 388(10052):1427-1436. |
| 6 | MCCULLOH C, NORDIN A, TALBOT L J, et al. Accuracy of prehospital care providers in determining total body surface area burned in severe pediatric thermal injury[J]. J Burn Care Res, 2018, 39(4):491-496. |
| 7 | CHAN L C, LEE M S, OU Y N, et al. Energy requirements for ICU burn patients in whom the total body surface area affected exceeds 50 percent: a practical equation[J]. Asia Pac J Clin Nutr, 2018, 27(6):1182-1189. |
| 8 | SHECKTER C C, LI A, PRIDGEN B, et al. The impact of skin allograft on inpatient outcomes in the treatment of major burns 20-50% total body surface area: a propensity score matched analysis using the nationwide inpatient sample[J]. Burns, 2019, 45(1):146-156. |
| 9 | KADDOURA I, ABU-SITTAH G, IBRAHIM A, et al. Burn injury: review of pathophysiology and therapeutic modalities in major burns[J]. Ann Burns Fire Disasters, 2017, 30(2):95-102. |
| 10 | CUTTLE L, KIMBLE R M. First aid treatment of burn injuries[J]. Wound Practice & Research, 2010, 18(1): 6-13. |
| 11 | GRIFFIN B R, FREAR C C, BABL F, et al. Cool running water first aid decreases skin grafting requirements in pediatric burns: a cohort study of two thousand four hundred ninety-five children[J]. Ann Emerg Med, 2020, 75(1):75-85. |
| 12 | MOFAZZAL J M A, SAHANDI Z P, MOOSAVI B S M, et al. Nanomedicine and advanced technologies for burns: preventing infection and facilitating wound healing[J]. Adv Drug Deliv Rev, 2018, 123:33-64. |
| 13 | STOICA A E, CHIRCOV C, GRUMEZESCU A M. Hydrogel dressings for the treatment of burn wounds: an up-to-date overview[J]. Materials (Basel), 2020, 13(12). |
| 14 | YAO Y, ZHANG A, YUAN C, et al. Recent trends on burn wound care: hydrogel dressings and scaffolds[J]. Biomater Sci, 2021, 9(13):4523-4540. |
| 15 | JANDERA V, HUDSON D A, DE W P M, et al. Cooling the burn wound: evaluation of different modalites[J]. Burns, 2000, 26(3):265-270. |
| 16 | GOODWIN N S, SPINKS A, WASIAK J. The efficacy of hydrogel dressings as a first aid measure for burn wound management in the pre-hospital setting: a systematic review of the literature[J]. Int Wound J, 2016, 13(4):519-525. |
| 17 | CHO Y S, CHOI Y H. Comparison of three cooling methods for burn patients: a randomized clinical trial[J]. Burns, 2017, 43(3):502-508. |
| 18 | RAHMAN M S, ISLAM R, RANA M M, et al. Characterization of burn wound healing gel prepared from human amniotic membrane and Aloe vera extract[J]. BMC Complement Altern Med, 2019, 19(1):115. |
| 19 | KATTAN A E, ALSHOMER F, ALHUJAYRI A K, et al. Current knowledge of burn injury first aid practices and applied traditional remedies: a nationwide survey[J]. Burns Trauma, 2016, 4:37. |
| 20 | WALLACE H J, O'NEILL T B, WOOD F M, et al. Determinants of burn first aid knowledge: cross-sectional study[J]. Burns, 2013, 39(6):1162-1169. |
| 21 | CUTTLE L, PEARN J, MCMILLAN J R, et al. A review of first aid treatments for burn injuries[J]. Burns, 2009, 35(6):768-775. |
| 22 | FADEYIBI I O, IBRAHIM N A, MUSTAFA I A, et al. Practice of first aid in burn related injuries in a developing country[J]. Burns, 2015, 41(6):1322-1332. |
| 23 | HYLAND E J, HARVEY J G, HOLLAND A J. First aid for burns: too little, too late and often wrong[J]. Med J Aust, 2014, 200(2):85. |
| 24 | 王德怀, 谭子明, 康滔, 等. 冷疗应用于烧伤现场急救处理现状Meta分析[J]. 临床军医杂志, 2019, 47(6): 582-585. |
| WANG D H, TAN Z M, KANG T, et al. Meta analysis on the current situation of cold therapy applied in emergency treatment of burns[J]. Clin J Med Off, 2019, 47(6): 582-585. | |
| 25 | WANG X S,CHEN B,ZHOU Z F. Atomization and surface heat transfer characteristics of cryogen spray cooling with expansion-chambered nozzles[J]. Int J Heat Mass Transf, 2018, 121(6): 15-27. |
| 26 | CHENG W,XIE B,HAN F, et al. An experimental investigation of heat transfer enhancement by addition of high-alcohol surfactant (HAS) and dissolving salt additive (DSA) in spray cooling[J]. Exp Therm Fluid Sci, 2013, 45(2): 198-202. |
| 27 | LIU H,CAI C,JIA M, et al. Experimental investigation on spray cooling with low-alcohol additives[J]. Appl Therm Eng, 2019, 146(1): 921-930. |
| 28 | GUPTA A,KOWALCZUK M,HEASELGRAVE W, et al. The production and application of hydrogels for wound management: a review[J]. Eur Polym J, 2019, 111(2): 134-151. |
| 29 | DHALIWAL K, LOPEZ N. Hydrogel dressings and their application in burn wound care[J]. Br J Community Nurs, 2018, 23(Sup9):S24-SS27. |
| 30 | ZHANG L, YIN H, LEI X, et al. A systematic review and meta-analysis of clinical effectiveness and safety of hydrogel dressings in the management of skin wounds[J]. Front Bioeng Biotechnol, 2019, 7:342. |
| [1] | 徐彤彤, 阮慧瞳. 负载白细胞介素-4的水凝胶微球调控卒中后免疫微环境对神经功能修复的影响[J]. 上海交通大学学报(医学版), 2025, 45(9): 1161-1170. |
| [2] | 周幸蝶, 陈泽昊, 吕振东, 张煜辉, 刘丽. 原位诱导低氧水凝胶对髓核细胞外基质分泌的促进作用[J]. 上海交通大学学报(医学版), 2025, 45(8): 990-1000. |
| [3] | 赵建磊, 赵婧琦, 刘唱, 黄靖竣, 金升元. 水动力清创治疗烧伤的效果:随机对照试验的系统评价[J]. 上海交通大学学报(医学版), 2025, 45(5): 614-623. |
| [4] | 徐唯, 李蒙, 王昊泽, 崔凯, 肖泽宇. 炎症部位定植水凝胶益生菌治疗炎性肠病的效果观察[J]. 上海交通大学学报(医学版), 2024, 44(7): 883-890. |
| [5] | 宋晨璐, 向军, 杨惠忠. 血清肝素结合蛋白对重度烧伤患者预后及脓毒症发生的早期预警价值[J]. 上海交通大学学报(医学版), 2024, 44(4): 474-481. |
| [6] | 陈泽昊, 吕振东, 张震, 崔文国, 张煜辉. 水凝胶刚度影响髓核细胞表型及其功能的体内外研究[J]. 上海交通大学学报(医学版), 2023, 43(7): 804-813. |
| [7] | 杨淑, 崔文国, 魏杰, 蔡正伟. 自愈合可注射性透明质酸水凝胶的构建及促进血管生成的研究[J]. 上海交通大学学报(医学版), 2023, 43(12): 1480-1492. |
| [8] | 马芳芳, 秦洁洁, 任灵杰, 唐笑梅, 刘佳, 施敏敏, 蒋玲曦. 基于水凝胶微球建立胰腺癌原代细胞的3D培养模型[J]. 上海交通大学学报(医学版), 2023, 43(1): 79-87. |
| [9] | 夏侗樑, 董家辰, 束蓉. 水凝胶缓释系统在牙周组织再生中的应用[J]. 上海交通大学学报(医学版), 2021, 41(7): 959-962. |
| [10] | 蔡传栋, 王非, 崔文国, 范存义, 刘珅. 基质金属蛋白酶响应性G4 PAMAM-IBU/GelMA水凝胶的构建及其特征研究[J]. 上海交通大学学报(医学版), 2021, 41(2): 140-146. |
| [11] | 刘立立1,崔文国1, 2. 负载骨形态发生蛋白2微球的可注射水凝胶的抑菌和成骨性能评价[J]. 上海交通大学学报(医学版), 2020, 40(9): 1184-1192. |
| [12] | 相宜 1, 2,刘立立 1, 2,崔文国 1, 2. 携载抗菌黏性脂质体的水凝胶构建及促进骨修复的研究[J]. 上海交通大学学报(医学版), 2019, 39(9): 947-. |
| [13] | 李学川,滕培敏,原博,乔亮,杨惠忠. 异型聚氨酯泡沫敷料促进大面积烧伤患者头皮供皮区愈合的研究[J]. 上海交通大学学报(医学版), 2019, 39(5): 514-. |
| [14] | 宁航,夏一如,董家辰,束蓉. 载重组人釉原蛋白水凝胶缓释系统对人牙周膜成纤维细胞 生物学特性的影响[J]. 上海交通大学学报(医学版), 2019, 39(3): 244-. |
| [15] | 徐正鹏 1,王粟 2,糜琛蓉 3,韩立中 2,王文奎 1. 烧伤患者感染病原菌的分布及耐药性分析[J]. 上海交通大学学报(医学版), 2019, 39(3): 292-. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||