结核病是由结核分枝杆菌引起的严重危害人类健康的慢性传染病,主要通过呼吸道飞沫传播,是传染病死亡的主要原因[1-3]。空洞、胸腔积液和结节在结核患者影像学中较多见,是引起咳嗽、咯血等临床症状的常见原因,是评估结核病预后的主要指标[4-6]。中国作为全球第3的结核病高负担国家[7],患者基数大,结核菌引起病症的同时常常伴有众多合并症,如糖尿病、高血压、肝脏和肾脏疾病等[8-12]。我国结核病患者糖尿病的总体患病率为7.8%,其中东部沿海地区的患病率达到8.3%[13]。我国高血压发病率逐年升高,一项横断面研究报道了结核患者的高血压患病率为15.2%[14]。目前系统研究各种合并症对结核病预后的影响报道不多,本研究采用回顾性队列研究,对450例结核患者的治疗结果和肺部损伤进行分析,探讨结核病诊断时的合并症对结核预后的影响,以期引导临床医生重视合并症结核患者的差异化治疗。
1 资料与方法
1.1 研究对象
选择2018年1月1日—2018年12月31日在同济大学附属上海市肺科医院治疗的结核患者。分组标准:①在结核病诊断时无其他合并症的结核患者为无合并症组。②合并患有糖尿病、高血压、肝脏疾病、肾脏疾病和胆囊疾病的合并症结核患者为合并症组。
纳入标准:①符合肺结核诊断标准[15],结核病病原学检测阳性的患者。②患者痰标本涂片阳性或结核分枝杆菌培养阳性;临床疑似非结核分枝杆菌(nontuberculous mycobacteria,NTM)患者辅助检测GeneXpertMTB/RIF阳性判为结核的患者。排除标准:①年龄<18周岁和>70周岁的患者。②抗结核药物耐药患者。③病历资料不全的患者。
1.2 治疗结果的判断标准
依据世界卫生组织(World Health Organization,WHO)发表的《结核病定义和报告框架》[16],完成治疗并且在治疗结束前至少2次涂片或培养呈阴性的患者判断为治愈,治疗方案需要终止或永久更改为新的方案或治疗策略的患者判断为治疗失败。
1.3 患者资料收集
通过同济大学附属上海市肺科医院信息处理数据库、电子病案系统收集结核患者的就诊资料,包括患者的人口学特征、临床症状、合并症、治疗结果以及影像学检测数据。收集2018年首次入院的CT资料,由2名经验丰富的影像学医师采用双盲法阅片,判断病灶分布、空洞积液和结节等情况,分析影像学特征。
1.4 统计学分析
采用SPSS25.0和GraphPad Prism 8软件进行统计分析。定量资料以M(Q1,Q3)表示。定性资料以频数(百分率)表示,采用χ2检验进行组间比较;当理论频数<5或总体样本量<40时,采用Fisher精确检验。采用Kaplan-Meier(K-M)分析计算生存曲线,并使用对数秩检验比较曲线之间的差异。P<0.05为差异有统计学意义。
2 结果
2.1 结核患者基本资料和临床特征
共纳入450例结核患者,中位年龄为33岁。患者的基本资料和临床特征如表1所示。
表1 结核患者基本资料和临床特征
Tab 1
| Item | Tuberculosis patients |
|---|---|
| Age/year | 33.00 (25.00, 51.25) |
| Gender/n(%) | |
| Male | 323 (71.8) |
| Female | 127 (28.2) |
| Fever/n(%) | 117 (26.0) |
| Cough/n(%) | 292 (64.9) |
| Hemoptysis/n(%) | 52 (11.6) |
| Sweat/n(%) | 23 (5.1) |
| Lose weight/n(%) | 10 (2.2) |
| Complication/n(%) | |
| Diabetes | 49 (10.9) |
| Hypertension | 23 (5.1) |
| Liver disease | 83 (18.4) |
| Kidney disease | 35 (7.8) |
| Gallbladder disease | 17 (3.8) |
| Grade of sputum smear/n(%) | |
| 1+ | 356 (79.1) |
| 2+ | 35 (7.8) |
| 3+ | 44 (9.8) |
| 4+ | 15 (3.3) |
2.2 结核病诊断时的合并症对结核治疗结果的影响
450例结核患者中,343例治愈,107例未治愈。如表2所示,173例诊断时有合并症的结核患者中有53例(30.6%)未治愈,未治愈率高于诊断时无合并症的结核患者(P=0.007)。诊断时有糖尿病、高血压和肾脏疾病的结核患者治愈率低于无合并症的结核患者,差异有统计学意义(均P<0.05);诊断时有肝脏疾病和胆囊疾病的结核患者与无合并症的结核患者治愈率比较,差异均无统计学意义(均P>0.05)。
表2 诊断时有、无合并症的结核患者治疗结果的比较 [n(%)]
Tab 2
| Group | Cured | Not-cured | χ2 value | P value |
|---|---|---|---|---|
| TB with/without complications | 7.293 | 0.007 | ||
| Without | 223 (80.5) | 54 (19.5) | ||
| With | 120 (69.4) | 53 (30.6) | ||
| TB with/without diabetes | 5.646 | 0.017 | ||
| Without | 223 (80.5) | 54 (19.5) | ||
| With | 32 (65.3) | 17 (34.7) | ||
| TB with/without hypertension | 7.279 | 0.011 | ||
| Without | 223 (80.5) | 54 (19.5) | ||
| With | 13 (56.5) | 10 (43.5) | ||
| TB with/without liver disease | 0.456 | 0.500 | ||
| Without | 223 (80.5) | 54 (19.5) | ||
| With | 64 (77.1) | 19 (22.9) | ||
| TB with/without kidney disease | 5.739 | 0.017 | ||
| Without | 223 (80.5) | 54 (19.5) | ||
| With | 22 (62.9) | 13 (37.1) | ||
| TB with/without gallbladder disease | 2.461 | 0.126 | ||
| Without | 223 (80.5) | 54 (19.5) | ||
| With | 11 (64.7) | 6 (35.3) | ||
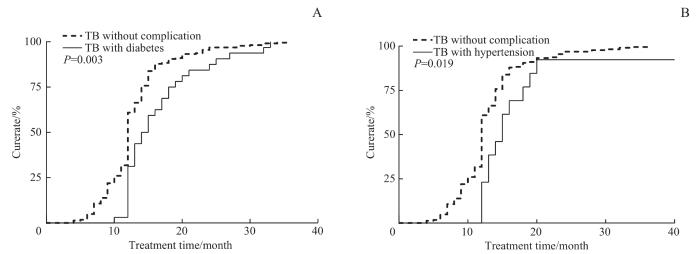
为探讨单一合并症对结核预后的影响,进一步对单一合并症的结核患者进行了抗结核治疗的预后分析,结果如表3所示。诊断时患有糖尿病的结核患者治愈率低于无合并症的结核患者,差异有统计学意义(P=0.007);诊断时有高血压的结核患者治愈率也低于无合并症的结核患者,差异有统计学意义(P=0.001)。
表3 诊断时仅患有1种合并症结核患者与无合并症患者治疗结果的比较 [n(%)]
Tab 3
| Group | Cured | Not-cured | χ2 value | P value |
|---|---|---|---|---|
| TB with/without diabete | 7.341 | 0.007 | ||
| Without | 223 (80.5) | 54 (19.5) | ||
| With | 15 (57.7) | 11 (42.3) | ||
| TB with/without hypertension | 14.413 | 0.001 | ||
| Without | 223 (80.5) | 54 (19.5) | ||
| With | 2 (25.0) | 6 (75.0) | ||
| TB with/without liver disease | 0.534 | 0.465 | ||
| Without | 223 (80.5) | 54 (19.5) | ||
| With | 38 (76.0) | 12 (24.0) | ||
| TB with/without kidney disease | 2.756 | 0.149 | ||
| Without | 223 (80.5) | 54 (19.5) | ||
| With | 8 (61.5) | 5 (38.4) | ||
| TB with/without gallbladder disease | 0.355 | 0.627 | ||
| Without | 223 (80.5) | 54 (19.5) | ||
| With | 5 (71.4) | 2 (28.5) | ||
图1
图1
诊断时患有糖尿病(A)与高血压(B)的结核患者与无合并症结核患者的生存曲线对比
Fig 1
Comparison of survival curve between tuberculosis patients with diabetes (A) and hypertension (B) at diagnosis and tuberculosis patients without complications
2.3 结核病诊断时的合并症对结核患者肺部损伤的影响
如表4所示,无合并症的结核患者中117例(42.2%)和诊断时有合并症的结核患者中101例(58.4%)双侧肺有损伤,差异有统计学意义(P=0.001)。诊断时有合并症的结核患者空洞发生率是40.5%,比无合并症的结核患者高14.5%,差异有统计学意义(P=0.001)。诊断时有合并症的结核患者肺部载菌量高于诊断时无合并症的结核患者,差异有统计学意义(P=0.007)。
表4 诊断时有、无合并症的结核患者肺部损伤的比较 [n(%)]
Tab 4
| Lung injury | TB without complications | TB with complications | χ2 value | P value |
|---|---|---|---|---|
| Area of lung injury | 11.112 | 0.001 | ||
| Bilateral lung | 117 (42.2) | 101 (58.4) | ||
| Unilateral lung | 160 (57.8) | 72 (41.6) | ||
| Cavity | 10.323 | 0.001 | ||
| Yes | 72 (26.0) | 70 (40.5) | ||
| No | 205 (74.0) | 103 (59.5) | ||
| Effusion | 0.606 | 0.436 | ||
| Yes | 46 (16.6) | 24 (13.9) | ||
| No | 231 (83.4) | 149 (86.1) | ||
| Nodule | 0.793 | 0.373 | ||
| Yes | 88 (31.8) | 62 (35.8) | ||
| No | 189 (68.2) | 111 (64.2) | ||
| Grade of sputum smear | 11.968 | 0.007 | ||
| 1+ | 227 (81.9) | 129 (74.6) | ||
| 2+ | 20 (7.2) | 15 (8.7) | ||
| 3+ | 27 (9.8) | 17 (9.8) | ||
| 4+ | 3 (1.1) | 12 (6.9) |
有合并症的结核患者肺部损伤分布在双侧肺的比例高于诊断时无合并症的结核患者(P=0.001),进一步细分发现仅糖尿病和肝脏疾病合并结核感染时影响肺部损伤。如表5所示,诊断时患有糖尿病的结核患者肺部损伤分布在双侧肺的比例高于诊断时无合并症的结核患者,差异有统计学意义(P=0.003);诊断时患有肝脏疾病的结核患者肺部损伤分布在双侧肺的比例高于诊断时无合并症的结核患者,差异有统计学意义(P=0.002)。
表5 诊断时有、无合并症的结核患者肺部损伤区域的比较 [n(%)]
Tab 5
| Group | Area of lung injury | χ2 value | P value | |
|---|---|---|---|---|
| Bilateral lung | Unilateral lung | |||
| TB with/without complications | 11.112 | 0.001 | ||
| Without | 117 (42.2) | 160 (57.8) | ||
| With | 101 (58.4) | 72 (41.6) | ||
| TB with/without diabetes | 8.928 | 0.003 | ||
| Without | 117 (42.2) | 160 (57.8) | ||
| With | 32 (65.3) | 17 (34.7) | ||
| TB with/without hypertension | 2.997 | 0.083 | ||
| Without | 117 (42.2) | 160 (57.8) | ||
| With | 14 (60.9) | 9 (39.1) | ||
| TB with/without liver disease | 9.467 | 0.002 | ||
| Without | 117 (42.2) | 160 (57.8) | ||
| With | 51 (61.5) | 32 (38.5) | ||
| TB with/without kidney disease | 0.509 | 0.476 | ||
| Without | 117 (42.2) | 160 (57.8) | ||
| With | 17 (48.6) | 18 (51.4) | ||
| TB with/without gallbladder disease | 3.289 | 0.070 | ||
| Without | 117 (42.2) | 160 (57.8) | ||
| With | 11 (64.7) | 6 (35.3) | ||
如表6所示,有合并症的结核患者肺部空洞发生率高于诊断时无合并症的结核患者。分层分析发现患有糖尿病的结核患者中33例(67.4%)发生空洞,患有肾脏疾病的结核患者中16例(45.7%)发生空洞,空洞发生率均高于无合并症的结核患者,差异有统计学意义(均P<0.05)。
表6 诊断时有、无合并症的结核患者肺部空洞的比较 [n(%)]
Tab 6
| Group | Cavity | χ2 value | P value | Group | Cavity | χ2 value | P value | ||
|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | ||||||
| TB with/without complications | 10.323 | 0.001 | TB with/without liver disease | 1.369 | 0.242 | ||||
| Without | 72 (26.0) | 205 (74.0) | Without | 72 (26.0) | 205 (74.0) | ||||
| With | 70 (40.5) | 103 (59.5) | With | 27 (32.5) | 56 (67.5) | ||||
| TB with/without diabetes | 32.610 | 0.000 | TB with/without kidney disease | 5.968 | 0.015 | ||||
| Without | 72 (26.0) | 205 (74.0) | Without | 72 (26.0) | 205 (74.0) | ||||
| With | 33 (67.4) | 16 (32.6) | With | 16 (45.7) | 19 (54.3) | ||||
| TB with/without hypertension | 0.000 | 0.992 | TB with/without gallbladder disease | 3.589 | 0.088 | ||||
| Without | 72 (26.0) | 205 (74.0) | Without | 72 (26.0) | 205 (74.0) | ||||
| With | 6 (26.1) | 17 (73.9) | With | 8 (47.1) | 9 (52.9) | ||||
如表7所示,合并症结核患者肺部载菌量更高且差异有统计学意义(P=0.007)。分层分析发现,患有糖尿病的结核患者肺部载菌量高于无合并症的结核患者,差异有统计学意义(P=0.000);患有肝脏疾病的结核患者肺部载菌量也高于无合并症的结核患者,差异有统计学意义(P=0.004)。诊断时合并患有高血压、肾脏疾病和胆囊疾病的结核患者肺部载菌量与无合并症的结核患者相比,差异均无统计学意义(均P>0.05)。
表7 诊断时有、无合并症的结核患者肺部载菌量情况比较 [n(%)]
Tab 7
| Group | Grade of sputum smear | χ2 value | P value | |||
|---|---|---|---|---|---|---|
| 1+ | 2+ | 3+ | 4+ | |||
| TB with complications | 11.968 | 0.007 | ||||
| Without | 227 (81.9) | 20 (7.2) | 27 (9.8) | 3 (1.1) | ||
| With | 129 (74.6) | 15 (8.7) | 17 (9.8) | 12 (6.9) | ||
| TB with diabetes | 27.877 | 0.000 | ||||
| Without | 227 (81.9) | 20 (7.2) | 27 (9.8) | 3 (1.1) | ||
| With | 28 (57.1) | 4 (8.2) | 11 (22.4) | 6 (12.3) | ||
| TB with hypertension | 7.640 | 0.083 | ||||
| Without | 227 (81.9) | 20 (7.2) | 27 (9.8) | 3 (1.1) | ||
| With | 17 (73.9) | 2 (8.7) | 2 (8.7) | 2 (8.7) | ||
| TB with liver disease | 13.597 | 0.004 | ||||
| Without | 227 (81.9) | 20 (7.2) | 27 (9.8) | 3 (1.1) | ||
| With | 66 (79.5) | 5 (6.0) | 5 (6.0) | 7 (8.5) | ||
| TB with kidney disease | 4.369 | 0.224 | ||||
| Without | 227 (81.9) | 20 (7.2) | 27 (9.8) | 3 (1.1) | ||
| With | 27 (77.1) | 3 (8.6) | 3 (8.6) | 2 (5.7) | ||
| TB with gallbladder disease | 3.474 | 0.302 | ||||
| Without | 227 (81.9) | 20 (7.2) | 27 (9.8) | 3 (1.1) | ||
| With | 12 (70.6) | 2 (11.8) | 2 (11.8) | 1 (5.8) | ||
3 讨论
结核病的高危险因素中,糖尿病位居第4位[7],罹患糖尿病会增加结核患者肺部损伤范围,增加治疗失败的风险[17-18]。本研究痰涂片结果显示,患有糖尿病的结核患者肺部载菌量高于无合并症的结核患者,糖尿病引起的免疫系统紊乱,导致抗结核菌感染的免疫功能障碍,减弱患者机体抗感染和修复能力,促进患者体内结核菌的生长和繁殖[19]。一项多中心横断面研究[20]表明,患有糖尿病的结核患者治疗失败的风险是无合并症患者的3.25倍,空洞发生的风险是无合并症患者的3.89倍。这与本研究的结果一致:患有糖尿病的结核患者未治愈率(34.7%)高于无合并症患者(19.5%),其空洞发生率(67.4%)高于无合并症患者(26.0%)。
我国的一项回顾性研究[11]分析了慢性肾脏疾病合并结核病的基本特征,数据显示慢性肾脏病患者的结核病发病率和死亡率明显高于普通人群,说明肾脏疾病会影响结核病的进展,但未探讨肾脏疾病对结核患者肺部损伤及预后的影响。本研究发现诊断时患有肾脏疾病的结核患者治愈率更低,空洞发生率更高,证明结核诊断时患有肾脏疾病会影响结核患者的预后,增加结核患者的肺部损伤。
本研究有一定的局限性。首先,本研究属于回顾性研究,存在选择偏倚。其次,纳入的样本量相对较少,在分析患有合并症的结核患者肺部损伤时,可能不能代表研究对象全貌。最后,本研究仅分析了诊断时结核患者的肺部损伤,未进一步分析抗结核治疗过程中肺部损伤情况。
总体来说,诊断时患有糖尿病、高血压和肾脏疾病的结核患者治愈率更低,患有糖尿病和肝脏疾病的结核患者肺部载菌量更多、肺部损伤区域更大,患有糖尿病和肾脏疾病的结核患者肺部空洞发生率更高。结核病诊断时的合并症对结核预后的不同影响,提示临床医生应重视合并症结核患者的差异化治疗,了解合并症对结核病的预后影响,方便及早采取干预措施,提高结核患者的治愈率,缩短治疗时间,降低医疗成本。
作者贡献声明
骆梦醒负责数据分析和论文撰写,参与研究设计;邹欣和高雅娴参与数据整理和数据统计;吴小翠和余方友参与数据整理;胡洋参与论文修改;曾奇兵和刘忠华负责研究设计和论文修改。所有作者均阅读并同意最终稿件的提交。
AUTHOR's CONTRIBUTIONS
LUO Mengxing performed the statistical analysis and drafted the manuscript, contributing to the study design. ZOU Xin and GAO Yaxian participated in data collation and data statistics. WU Xiaocui and YU Fangyong participated in data collation. HU Yang was involved in the revision of the manuscrip. ZENG Qibing and LIU Zhonghua were responsible for the study design and revised the manuscript. All the authors have read the last version of paper and consented for submission.
利益冲突声明
所有作者声明不存在利益冲突。
COMPETING INTERESTS
All authors disclose no relevant conflict of interests.
参考文献