
上海交通大学学报(医学版) ›› 2021, Vol. 41 ›› Issue (2): 173-179.doi: 10.3969/j.issn.1674-8115.2021.02.008
收稿日期:2020-06-01
出版日期:2021-02-28
发布日期:2021-02-28
作者简介:胡培堃(1993—),男,住院医师,博士生;电子信箱:基金资助:
Pei-kun HU( ), Jie HE, Lian-ming WU, Heng GE, Jian-rong XU, Jun PU(
), Jie HE, Lian-ming WU, Heng GE, Jian-rong XU, Jun PU( )
)
Received:2020-06-01
Online:2021-02-28
Published:2021-02-28
Supported by:摘要:
目的·应用心脏磁共振(cardiac magnetic resonance,CMR)技术,探究ST段抬高型心肌梗死(ST-segment elevation myocardial infarction,STEMI)患者微血管阻塞(microvascular obstruction,MVO)对左室功能及预后的影响。方法·纳入2016年1月—2017年12月于上海交通大学医学院附属仁济医院心内科就诊的STEMI患者124例,应用CMR技术评估患者再灌注后心肌梗死百分比、心肌MVO百分比及左室功能。依据心肌MVO百分比,将患者分为MVO(+)组和MVO(-)组,比较2组的基线特征、血生化指标和CMR指标。MVO(+)组依据心肌梗死百分比的四分位数进一步分为4个亚组,利用Pearson相关分析探究各亚组患者心肌MVO百分比与左室射血分数(left ventricular ejection fraction,LVEF)的相关性。随访所有患者30 d内不良事件的发生情况,采用受试者操作特征曲线(receiver operating characteristic curve,ROC曲线)分析心肌MVO百分比对不良事件的预测价值。结果·在基线特征无明显差异的情况下,MVO(+)组的白细胞计数、血清磷酸肌酸激酶、肌酸激酶同工酶、心肌肌钙蛋白I、总胆固醇水平均高于MVO(-)组(均P<0.05)。MVO(+)组的LVEF低于MVO(-)组(P=0.000)。Pearson相关分析显示,心肌MVO百分比与LVEF呈负相关(均P<0.05)。ROC曲线显示,心肌MVO百分比预测患者30 d内不良事件的曲线下面积为0.889(95%CI 0.823~0.975),其敏感度和特异度均高于心肌梗死百分比。结论·合并MVO的STEMI患者的左室功能及预后更差,提示需更加重视对于此类患者的临床干预。
中图分类号:
胡培堃, 何杰, 吴连明, 葛恒, 许建荣, 卜军. ST段抬高型心肌梗死患者微血管阻塞对左室功能及预后的影响[J]. 上海交通大学学报(医学版), 2021, 41(2): 173-179.
Pei-kun HU, Jie HE, Lian-ming WU, Heng GE, Jian-rong XU, Jun PU. Effect of microvascular obstruction on left ventricle function and prognosis in patients with ST-segment elevation myocardial infarction[J]. JOURNAL OF SHANGHAI JIAOTONG UNIVERSITY (MEDICAL SCIENCE), 2021, 41(2): 173-179.
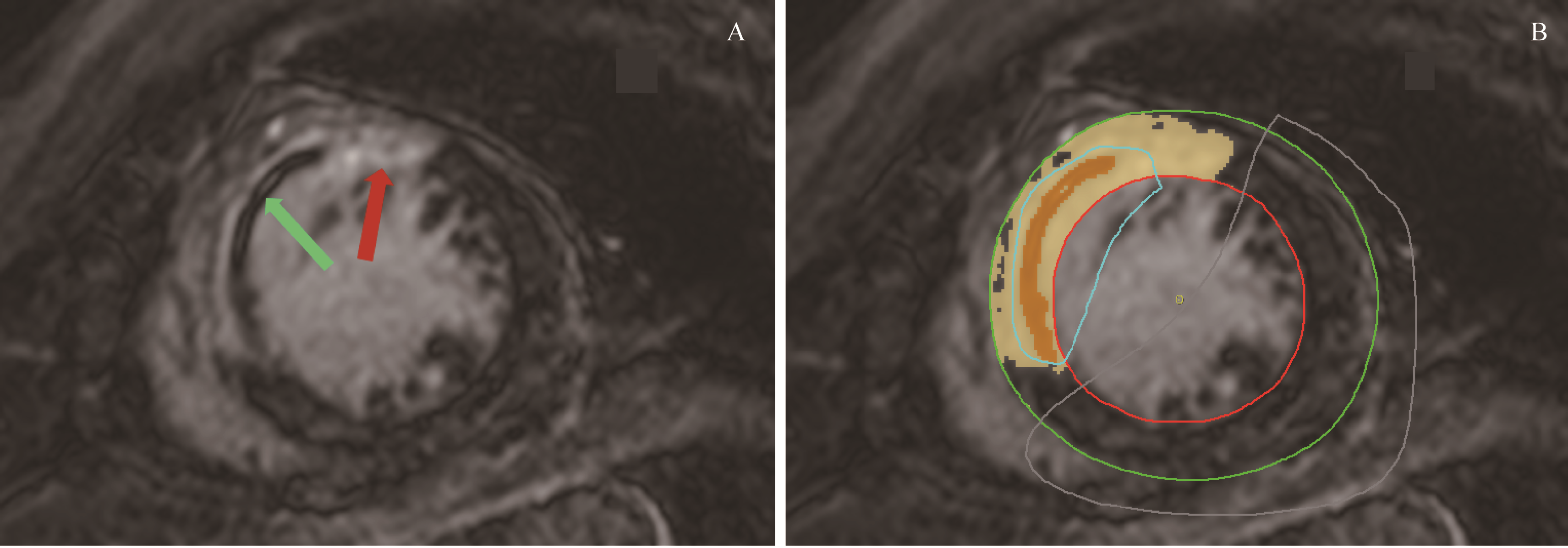
图1 CVI 42软件识别心肌梗死区和心肌MVO区Note:A. Original CMR image. Red arrow is pointing at the myocardial infarction region, and green arrow is pointing at the myocardial MVO region. B. CVI 42 software marked the myocardial infarction region as golden yellow, and the myocardial MVO region as orange. Colored lines were drawn by software operator.
Fig 1 Identification of myocardial infarction region and myocardial MVO region by CVI 42 software
| Characteristic | MVO (+) group (N=82) | MVO (-) group (N=42) | P value |
|---|---|---|---|
| Age/year | 58.6±7.9 | 58.7±8.4 | 0.958 |
| Gender/n (%) | 0.098 | ||
| Male | 76 (92.7) | 34 (81.0) | |
| Female | 6 (7.3) | 8 (19.0) | |
| Smoking history/n (%) | 65 (79.3) | 30 (71.4) | 0.329 |
| Drinking history/n (%) | 22 (26.8) | 13 (31.0) | 0.629 |
| Hypertension/n (%) | 48 (58.5) | 19 (45.2) | 0.160 |
| Diabetes mellitus/n (%) | 30 (36.6) | 12 (28.6) | 0.372 |
| Hypercholesterolemia/n (%) | 46 (56.1) | 19 (45.2) | 0.252 |
| Previous angina/n (%) | 42 (51.2) | 25 (59.5) | 0.380 |
| Renal dysfunction/n (%) | 3 (3.7) | 0 (0) | 0.524 |
| Previous stroke/n (%) | 0 (0) | 1 (2.4) | 0.732 |
| Pain-to-balloon time/h | 5.5±3.2 | 4.9±1.6 | 0.166 |
| Reperfusion therapy/n (%) | 1.000 | ||
| PPCI | 41 (50.0) | 21 (50.0) | |
| PCI after thrombolysis | 41 (50.0) | 21 (50.0) | |
| Culprit vessel/n (%) | 0.398 | ||
| LAD | 47 (57.3) | 25 (59.5) | |
| LCX | 10 (12.2) | 2 (4.8) | |
| RCA | 25 (30.5) | 15 (35.7) | |
| Killip class/n (%) | 1.000 | ||
| Ⅰ | 74 (90.2) | 38 (90.5) | |
| Ⅱ | 7 (8.5) | 3 (7.1) | |
| Ⅲ | 1 (1.2) | 1 (2.4) | |
| Time delay from the onset of chest pain to CMR/d | 5.2±2.2 | 5.3±1.8 | 0.863 |
表1 2组患者的基线特征比较
Tab 1 Comparison of baseline characteristics between the two groups
| Characteristic | MVO (+) group (N=82) | MVO (-) group (N=42) | P value |
|---|---|---|---|
| Age/year | 58.6±7.9 | 58.7±8.4 | 0.958 |
| Gender/n (%) | 0.098 | ||
| Male | 76 (92.7) | 34 (81.0) | |
| Female | 6 (7.3) | 8 (19.0) | |
| Smoking history/n (%) | 65 (79.3) | 30 (71.4) | 0.329 |
| Drinking history/n (%) | 22 (26.8) | 13 (31.0) | 0.629 |
| Hypertension/n (%) | 48 (58.5) | 19 (45.2) | 0.160 |
| Diabetes mellitus/n (%) | 30 (36.6) | 12 (28.6) | 0.372 |
| Hypercholesterolemia/n (%) | 46 (56.1) | 19 (45.2) | 0.252 |
| Previous angina/n (%) | 42 (51.2) | 25 (59.5) | 0.380 |
| Renal dysfunction/n (%) | 3 (3.7) | 0 (0) | 0.524 |
| Previous stroke/n (%) | 0 (0) | 1 (2.4) | 0.732 |
| Pain-to-balloon time/h | 5.5±3.2 | 4.9±1.6 | 0.166 |
| Reperfusion therapy/n (%) | 1.000 | ||
| PPCI | 41 (50.0) | 21 (50.0) | |
| PCI after thrombolysis | 41 (50.0) | 21 (50.0) | |
| Culprit vessel/n (%) | 0.398 | ||
| LAD | 47 (57.3) | 25 (59.5) | |
| LCX | 10 (12.2) | 2 (4.8) | |
| RCA | 25 (30.5) | 15 (35.7) | |
| Killip class/n (%) | 1.000 | ||
| Ⅰ | 74 (90.2) | 38 (90.5) | |
| Ⅱ | 7 (8.5) | 3 (7.1) | |
| Ⅲ | 1 (1.2) | 1 (2.4) | |
| Time delay from the onset of chest pain to CMR/d | 5.2±2.2 | 5.3±1.8 | 0.863 |
| Index | MVO (+) group (N=82) | MVO (-) group (N=42) | P value |
|---|---|---|---|
| Blood biochemical index | |||
| CRP/(mg·L-1) | 5.92 (1.52, 22.03) | 3.95 (2.42, 12.53) | 0.720 |
| WBC/(×109·L-1) | 11.95 (10.01, 13.95) | 10.21 (7.92, 12.85) | 0.016 |
| Hb/(g·L-1) | 145.23±16.16 | 140.31±14.37 | 0.109 |
| PLT/(×109·L-1) | 195.85±48.77 | 211.36±49.15 | 0.097 |
| FBG/(g·L-1) | 2.81±0.71 | 2.88±0.58 | 0.588 |
| PT/s | 10.70 (10.00, 11.83) | 10.60 (10.10, 11.70) | 0.755 |
| APTT/s | 32.10 (28.70, 36.30) | 33.65 (29.15, 36.18) | 0.748 |
| INR | 0.94 (0.88, 0.99) | 0.93 (0.88, 1.01) | 0.919 |
| Scr/(μmol·L-1) | 71.70±19.35 | 70.11±14.27 | 0.640 |
| BUN/(mmol·L-1) | 5.60±1.65 | 5.32±1.76 | 0.375 |
| Glu/(mmol·L-1) | 5.72 (5.09, 6.61) | 5.29 (4.80, 6.16) | 0.093 |
| TAG/(mmol·L-1) | 1.37 (0.96, 2.51) | 1.31 (0.95, 1.63) | 0.240 |
| TC/(mmol·L-1) | 5.21±1.10 | 4.77±1.05 | 0.039 |
| HDL-Ch/(mmol·L-1) | 1.17±0.26 | 1.16±0.27 | 0.920 |
| LDL-Ch/(mmol·L-1) | 3.21±0.86 | 3.09±0.88 | 0.450 |
| CPK/(U·L-1) | 3 632.00 (2 547.00, 5 151.25) | 1 565.00 (1 074.50, 3 228.00) | 0.000 |
| CK-MB/(U·L-1) | 370.75 (241.43, 480.45) | 201.60 (120.95, 288.25) | 0.000 |
| cTnI/(ng·mL-1) | 26.34 (1.54, 80.85) | 10.33 (0.93, 28.40) | 0.022 |
| BNP/(pg·mL-1) | 101.50 (37.95, 275.00) | 93.80 (17.38, 203.00) | 0.202 |
| CMR index | |||
| LVEF/% | 47.07±8.94 | 53.95±5.79 | 0.000 |
| Percentage of myocardial infarction/% | 23.09 (17.41, 30.46) | 11.25 (6.40, 18.14) | 0.000 |
表2 2组患者的血生化指标及CMR指标比较
Tab 2 Comparison of blood biochemical indexes and CMR indexes between the two groups
| Index | MVO (+) group (N=82) | MVO (-) group (N=42) | P value |
|---|---|---|---|
| Blood biochemical index | |||
| CRP/(mg·L-1) | 5.92 (1.52, 22.03) | 3.95 (2.42, 12.53) | 0.720 |
| WBC/(×109·L-1) | 11.95 (10.01, 13.95) | 10.21 (7.92, 12.85) | 0.016 |
| Hb/(g·L-1) | 145.23±16.16 | 140.31±14.37 | 0.109 |
| PLT/(×109·L-1) | 195.85±48.77 | 211.36±49.15 | 0.097 |
| FBG/(g·L-1) | 2.81±0.71 | 2.88±0.58 | 0.588 |
| PT/s | 10.70 (10.00, 11.83) | 10.60 (10.10, 11.70) | 0.755 |
| APTT/s | 32.10 (28.70, 36.30) | 33.65 (29.15, 36.18) | 0.748 |
| INR | 0.94 (0.88, 0.99) | 0.93 (0.88, 1.01) | 0.919 |
| Scr/(μmol·L-1) | 71.70±19.35 | 70.11±14.27 | 0.640 |
| BUN/(mmol·L-1) | 5.60±1.65 | 5.32±1.76 | 0.375 |
| Glu/(mmol·L-1) | 5.72 (5.09, 6.61) | 5.29 (4.80, 6.16) | 0.093 |
| TAG/(mmol·L-1) | 1.37 (0.96, 2.51) | 1.31 (0.95, 1.63) | 0.240 |
| TC/(mmol·L-1) | 5.21±1.10 | 4.77±1.05 | 0.039 |
| HDL-Ch/(mmol·L-1) | 1.17±0.26 | 1.16±0.27 | 0.920 |
| LDL-Ch/(mmol·L-1) | 3.21±0.86 | 3.09±0.88 | 0.450 |
| CPK/(U·L-1) | 3 632.00 (2 547.00, 5 151.25) | 1 565.00 (1 074.50, 3 228.00) | 0.000 |
| CK-MB/(U·L-1) | 370.75 (241.43, 480.45) | 201.60 (120.95, 288.25) | 0.000 |
| cTnI/(ng·mL-1) | 26.34 (1.54, 80.85) | 10.33 (0.93, 28.40) | 0.022 |
| BNP/(pg·mL-1) | 101.50 (37.95, 275.00) | 93.80 (17.38, 203.00) | 0.202 |
| CMR index | |||
| LVEF/% | 47.07±8.94 | 53.95±5.79 | 0.000 |
| Percentage of myocardial infarction/% | 23.09 (17.41, 30.46) | 11.25 (6.40, 18.14) | 0.000 |
| Adverse event | MVO (+) group (N=82) | MVO (-) group (N=42) | P value |
|---|---|---|---|
| All-cause mortality/n (%) | 1 (1.2) | 0 (0) | 1.000 |
| Myocardial reinfarction/n (%) | 2 (2.4) | 0 (0) | 0.548 |
| Recurrent angina/n (%) | 8 (9.8) | 3 (7.1) | 0.880 |
| Heart failure/n (%) | 14 (17.1) | 1 (2.4) | 0.018 |
表3 2组患者30 d内不良事件比较
Tab 3 Comparison of adverse events within 30 days between the two groups
| Adverse event | MVO (+) group (N=82) | MVO (-) group (N=42) | P value |
|---|---|---|---|
| All-cause mortality/n (%) | 1 (1.2) | 0 (0) | 1.000 |
| Myocardial reinfarction/n (%) | 2 (2.4) | 0 (0) | 0.548 |
| Recurrent angina/n (%) | 8 (9.8) | 3 (7.1) | 0.880 |
| Heart failure/n (%) | 14 (17.1) | 1 (2.4) | 0.018 |
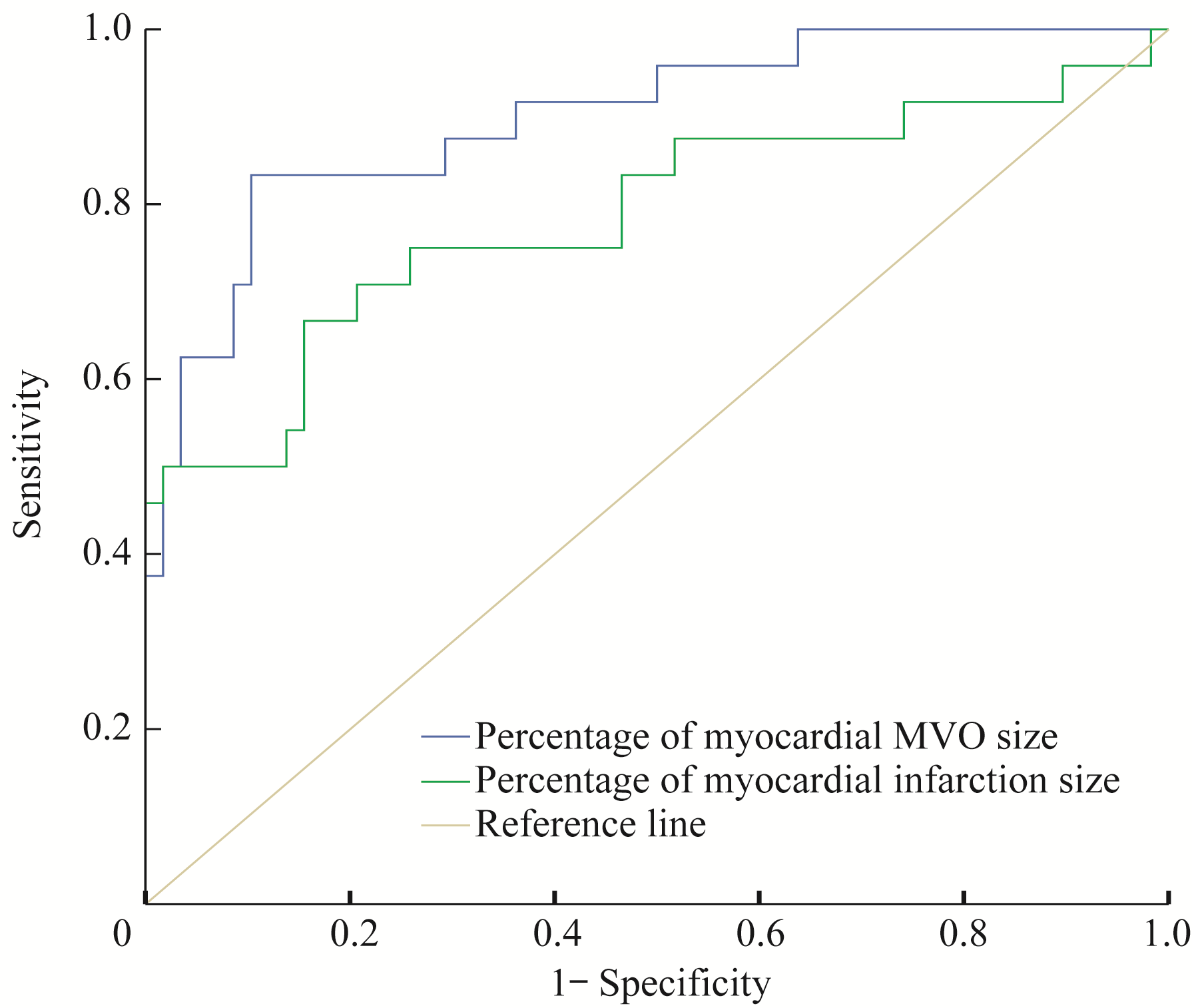
图3 心肌MVO百分比与心肌梗死百分比对MVO(+)患者30 d内不良事件预测价值的ROC曲线
Fig 3 ROC curve of predictive value of the percentage of myocardial MVO size and myocardial infarction size for adverse events within 30 days in the MVO(+) patients
| Index | AUC | 95%CI | Youden index | Cut-off value | Sensitivity/% | Specificity/% | P value |
|---|---|---|---|---|---|---|---|
| Percentage of myocardial MVO size | 0.899 | 0.823?0.975 | 0.730 | 2.99 | 83.3 | 89.7 | 0.000 |
| Percentage of myocardial infarction size | 0.785 | 0.660?0.911 | 0.512 | 29.70 | 66.7 | 84.5 | 0.000 |
表4 心肌MVO百分比与心肌梗死百分比预测价值的比较分析
Tab 4 Comparative analysis of predictive value of the percentage of myocardial MVO size and the percentage of myocardial infarction size
| Index | AUC | 95%CI | Youden index | Cut-off value | Sensitivity/% | Specificity/% | P value |
|---|---|---|---|---|---|---|---|
| Percentage of myocardial MVO size | 0.899 | 0.823?0.975 | 0.730 | 2.99 | 83.3 | 89.7 | 0.000 |
| Percentage of myocardial infarction size | 0.785 | 0.660?0.911 | 0.512 | 29.70 | 66.7 | 84.5 | 0.000 |
| 1 | Nabel EG, Braunwald E. A tale of coronary artery disease and myocardial infarction[J]. N Engl J Med, 2012, 366(1): 54-63. |
| 2 | Çağdaş M, Karakoyun S, Rencüzoğulları İ, et al. Assessment of the relationship between reperfusion success and T-peak to T-end interval in patients with ST elevation myocardial infarction treated with percutaneous coronary intervention[J]. Anatol J Cardiol, 2018, 19(1): 50-57. |
| 3 | Fajar JK, Heriansyah T, Rohman MS. The predictors of no reflow phenomenon after percutaneous coronary intervention in patients with ST elevation myocardial infarction: a meta-analysis[J]. Indian Heart J, 2018, 70 (): S406-S418. |
| 4 | Niccoli G, Burzotta F, Galiuto L, et al. Myocardial no-reflow in humans[J]. J Am Coll Cardiol, 2009, 54(4): 281-292. |
| 5 | Pu J, Ding S, Ge H, et al. Efficacy and safety of a pharmaco-invasive strategy with half-dose alteplase versus primary angioplasty in ST-segment-elevation myocardial infarction: EARLY-MYO trial (early routine catheterization after alteplase fibrinolysis versus primary PCI in acute ST-segment-elevation myocardial infarction)[J]. Circulation, 2017, 136(16): 1462-1473. |
| 6 | He J, Kong LC, Zeng JT, et al. Comparison of direct stenting with conventional strategy on myocardial impairments in ST-segment elevation myocardial infarction: a cardiac magnetic resonance imaging study[J]. Int J Cardiovasc Imaging, 2020, 36(6): 1167-1175. |
| 7 | de Waha S, Desch S, Eitel I, et al. Impact of early vs. late microvascular obstruction assessed by magnetic resonance imaging on long-term outcome after ST-elevation myocardial infarction: a comparison with traditional prognostic markers[J]. Eur Heart J, 2010, 31(21): 2660-2668. |
| 8 | Cochet AA, Lorgis L, Lalande A, et al. Major prognostic impact of persistent microvascular obstruction as assessed by contrast-enhanced cardiac magnetic resonance in reperfused acute myocardial infarction[J]. Eur Radiol, 2009, 19(9): 2117-2126. |
| 9 | Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018)[J]. J Am Coll Cardiol, 2018, 72(18): 2231-2264. |
| 10 | Ezekowitz JA, Kaul P, Bakal JA, et al. Declining in-hospital mortality and increasing heart failure incidence in elderly patients with first myocardial infarction[J]. J Am Coll Cardiol, 2009, 53(1): 13-20. |
| 11 | Weir RA, Murphy CA, Petrie CJ, et al. Microvascular obstruction remains a portent of adverse remodeling in optimally treated patients with left ventricular systolic dysfunction after acute myocardial infarction[J]. Circ Cardiovasc Imaging, 2010, 3(4): 360-367. |
| 12 | Hammer-Hansen S, Leung SW, Hsu LY, et al. Early gadolinium enhancement for determination of area at risk: a preclinical validation study[J]. JACC Cardiovasc Imaging, 2017, 10(2): 130-139. |
| 13 | Wu KC, Weiss RG, Thiemann DR, et al. Late gadolinium enhancement by cardiovascular magnetic resonance heralds an adverse prognosis in nonischemic cardiomyopathy[J]. J Am Coll Cardiol, 2008, 51(25): 2414-2421. |
| 14 | Hamirani YS, Wong A, Kramer CM, et al. Effect of microvascular obstruction and intramyocardial hemorrhage by CMR on LV remodeling and outcomes after myocardial infarction: a systematic review and meta-analysis[J]. JACC Cardiovasc Imaging, 2014, 7(9): 940-952. |
| 15 | Abbas A, Matthews GH, Brown IW, et al. Cardiac MR assessment of microvascular obstruction[J]. Br J Radiol, 2015, 88(1047): 20140470. |
| 16 | Yellon DM, Hausenloy DJ. Myocardial reperfusion injury[J]. N Engl J Med, 2007, 357(11): 1121-1135. |
| 17 | Mangold A, Alias S, Scherz T, et al. Coronary neutrophil extracellular trap burden and deoxyribonuclease activity in ST-elevation acute coronary syndrome are predictors of ST-segment resolution and infarct size[J]. Circ Res, 2015, 116(7): 1182-1192. |
| 18 | Lombardo A, Niccoli G, Natale L, et al. Impact of microvascular obstruction and infarct size on left ventricular remodeling in reperfused myocardial infarction: a contrast-enhanced cardiac magnetic resonance imaging study[J]. Int J Cardiovasc Imaging, 2012, 28(4): 835-842. |
| 19 | Mori H, Isobe S, Sakai S, et al. Microvascular obstruction on delayed enhancement cardiac magnetic resonance imaging after acute myocardial infarction, compared with myocardial (201)Tl and (123)I-BMIPP dual SPECT findings[J]. Eur J Radiol, 2015, 84(8): 1516-1524. |
| 20 | Wong DT, Leung MC, Richardson JD, et al. Cardiac magnetic resonance derived late microvascular obstruction assessment post ST-segment elevation myocardial infarction is the best predictor of left ventricular function: a comparison of angiographic and cardiac magnetic resonance derived measurements[J]. Int J Cardiovasc Imaging, 2012, 28(8): 1971-1981. |
| 21 | Roger VL. Epidemiology of heart failure[J]. Circ Res, 2013, 113(6): 646-659. |
| 22 | Durante A, Laricchia A, Benedetti G, et al. Identification of high-risk patients after ST-segment-elevation myocardial infarction: comparison between angiographic and magnetic resonance parameters[J]. Circ Cardiovasc Imaging, 2017, 10(6): e005841. |
| 23 | Zhang L, Mandry D, Chen B, et al. Impact of microvascular obstruction on left ventricular local remodeling after reperfused myocardial infarction[J]. J Magn Reson Imaging, 2018, 47(2): 499-510. |
| 24 | Ørn S, Manhenke C, Greve OJ, et al. Microvascular obstruction is a major determinant of infarct healing and subsequent left ventricular remodelling following primary percutaneous coronary intervention[J]. Eur Heart J, 2009, 30(16): 1978-1985. |
| 25 | Borlaug BA, Lam CS, Roger VL, et al. Contractility and ventricular systolic stiffening in hypertensive heart disease insights into the pathogenesis of heart failure with preserved ejection fraction[J]. J Am Coll Cardiol, 2009, 54(5): 410-418. |
| [1] | 何嘉音, 陈思远, 施晴, 张慕晨, 易红梅, 董磊, 钱樱, 王黎, 程澍, 许彭鹏, 赵维莅. 肾上腺累及的弥漫性大B细胞淋巴瘤患者临床病理特征、基因突变谱及预后分析[J]. 上海交通大学学报(医学版), 2025, 45(9): 1194-1201. |
| [2] | 陈思远, 施晴, 付迪, 王黎, 程澍, 许彭鹏, 赵维莅. 肺受累弥漫大B细胞淋巴瘤临床病理特征、基因突变谱及预后分析[J]. 上海交通大学学报(医学版), 2025, 45(9): 1214-1220. |
| [3] | 严治, 吴星玥, 姚卫芹, 颜灵芝, 金松, 商京晶, 施晓兰, 吴德沛, 傅琤琤. 免疫不全麻痹在新诊断多发性骨髓瘤患者中的动态变化及预后意义[J]. 上海交通大学学报(医学版), 2025, 45(7): 807-814. |
| [4] | 李卓杭, 于新迪, 任婧雅, 沈佳, 董素贞, 王伟. 主动脉缩窄端侧吻合纠治术后的神经系统预后分析[J]. 上海交通大学学报(医学版), 2025, 45(6): 753-759. |
| [5] | 汤开然, 冯成领, 韩邦旻. 基于单细胞测序与转录组测序构建M2巨噬细胞基因相关的前列腺癌预后模型[J]. 上海交通大学学报(医学版), 2025, 45(5): 549-561. |
| [6] | 许天芸, 沈奕茗, 姜萌. 射血分数改善型心力衰竭的临床管理: 治疗与维持[J]. 上海交通大学学报(医学版), 2025, 45(4): 493-499. |
| [7] | 刘田恬, 赵奕琳, 宁菁菁, 张育才, 王春霞. 儿童脓毒症预后相关长链非编码RNA筛选及竞争性内源RNA网络的构建[J]. 上海交通大学学报(医学版), 2025, 45(3): 282-291. |
| [8] | 王博恩, 陈思远, 施晴, 张慕晨, 易红梅, 董磊, 王黎, 程澍, 许彭鹏, 赵维莅. 肾脏累及的弥漫性大B细胞淋巴瘤患者临床病理特征[J]. 上海交通大学学报(医学版), 2024, 44(9): 1162-1168. |
| [9] | 宋晨璐, 向军, 杨惠忠. 血清肝素结合蛋白对重度烧伤患者预后及脓毒症发生的早期预警价值[J]. 上海交通大学学报(医学版), 2024, 44(4): 474-481. |
| [10] | 王桂杰, 杜传冲, 陆叶, 赵健, 沈勰, 金冬林, 耿佳财. 多发伤患者血清高迁移率族蛋白B1及可溶性髓样细胞触发受体-1水平变化及预后意义[J]. 上海交通大学学报(医学版), 2024, 44(3): 350-357. |
| [11] | 杜沚珊, 王玥, 石子旸, 施晴, 易红梅, 董磊, 王黎, 程澍, 许彭鹏, 赵维莅. 甲状腺弥漫性大B细胞淋巴瘤临床病理特征、基因突变谱及预后分析[J]. 上海交通大学学报(医学版), 2024, 44(1): 64-71. |
| [12] | 刘启明, 卢启帆, 柴烨子, 姜萌, 卜军. 心脏磁共振短轴电影成像影像组学鉴别肥厚型心肌病与健康对照[J]. 上海交通大学学报(医学版), 2024, 44(1): 79-86. |
| [13] | 刘启明, 卢启帆, 柴烨子, 姜萌, 卜军. 基于影像组学特征预测左室射血分数的可行性研究[J]. 上海交通大学学报(医学版), 2023, 43(9): 1162-1168. |
| [14] | 骆梦醒, 邹欣, 高雅娴, 吴小翠, 余方友, 胡洋, 曾奇兵, 刘忠华. 结核病合并基础疾病患者的抗结核治疗效果及肺部损伤分析[J]. 上海交通大学学报(医学版), 2023, 43(8): 1017-1023. |
| [15] | 李瑛, 谭阳霞, 尹虹心, 蒋雁翎, 陈立, 蒙国宇. ZNF384融合亚型急性白血病的发病机制及预后研究进展[J]. 上海交通大学学报(医学版), 2023, 43(5): 631-640. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||