
上海交通大学学报(医学版) ›› 2022, Vol. 42 ›› Issue (3): 312-322.doi: 10.3969/j.issn.1674-8115.2022.03.008
收稿日期:2021-12-24
出版日期:2022-03-28
发布日期:2022-05-09
通讯作者:
王红霞,电子信箱:whx365@126.com。作者简介:许静轩(1996—),女,硕士生;电子信箱:zzxjx1996@163.com。
基金资助:
XU Jingxuan( ), DU Shaoqian, CAO Yuan, WANG Hongxia(
), DU Shaoqian, CAO Yuan, WANG Hongxia( ), HUANG Weiyi(
), HUANG Weiyi( )
)
Received:2021-12-24
Online:2022-03-28
Published:2022-05-09
Contact:
WANG Hongxia, E-mail: whx365@126.com.Supported by:摘要:
目的·探究基质金属蛋白酶14(matrix metalloproteinase 14,MMP14)在胰腺癌组织中的表达及其与临床特征的相关性,并分析其与胰腺癌肿瘤免疫微环境特征的相关性。方法·通过GEPIA(Gene Expression Profiling Interactive Analysis)数据平台分析MMP家族成员在30种常见肿瘤组织中的表达情况。通过R语言整合GTEx(Genotype-Tissue Expression)数据库中167例胰腺正常组织和TCGA(The Cancer Genome Atlas)数据库中178例胰腺癌组织及4例配对癌旁组织的转录组数据,比较MMP14在胰腺癌与正常组织及癌旁组织中的表达差异。使用GEPIA数据平台对不同MMP14表达水平胰腺癌患者进行生存分析。从TCGA数据库中下载178例胰腺癌患者的相关临床信息,应用Perl和R语言分析MMP14的表达与临床特征的相关性。应用R语言和GSEA v3.0进行京都基因与基因组百科全书(Kyoto Encyclopedia of Genes and Genomes,KEGG)通路富集分析和基因本体论(Gene Ontology,GO)功能富集分析。采用CIBERSORT反卷积算法计算胰腺癌免疫微环境中各类免疫细胞亚群比例,分析MMP14的表达与各免疫细胞亚群比例的相关性。收集6例新鲜胰腺癌组织和配对癌旁组织,流式细胞术检测各类免疫细胞亚群;通过t-SNE降维与统计学分析,描述胰腺癌免疫微环境的特征。利用胰腺癌组织芯片进行多色荧光免疫组织化学实验,检测MMP14的表达与免疫细胞亚群的比例,验证生物信息学分析结果。结果·在生物信息学数据库中,与MMP家族其他成员相比,MMP14在多种肿瘤中高表达,且胰腺癌中MMP14的表达水平高于其他肿瘤;MMP14在胰腺癌中表达水平显著高于胰腺正常组织和癌旁组织(P=0.000),TNM分期Ⅱ期肿瘤MMP14表达水平显著高于Ⅰ期(P=0.012),病理组织学分级G2和G3期肿瘤MMP14显著高于G1期(均P=0.000)。MMP14低表达组患者生存预后显著优于高表达组(P=0.033)。KEGG和GO分析结果显示MMP14主要富集在胰腺癌和免疫相关通路。MMP14的表达水平与CD8+ T细胞、单核细胞的比例呈负相关(均P<0.05),与巨噬细胞的比例呈正相关(P=0.000)。流式细胞实验结果提示胰腺癌肿瘤微环境呈现免疫抑制性。多色荧光免疫组织化学实验结果显示,MMP14在肿瘤组织中表达水平显著高于癌旁组织(P=0.000),TNM分期较晚及病理组织学分级较高的肿瘤MMP14的表达水平也相对较高(均P<0.05)。在MMP14高表达的肿瘤组织中,CD8+ T细胞比例降低(P=0.001),巨噬细胞比例升高(P=0.000),与生物信息学分析结果一致。结论·与正常胰腺组织和癌旁组织相比,MMP14在胰腺癌中的表达显著升高且与患者不良预后相关;MMP14高表达的胰腺癌组织中CD8+ T细胞比例降低,巨噬细胞比例升高;高表达MMP14的胰腺癌肿瘤微环境呈现高度免疫抑制性。
中图分类号:
许静轩, 杜少倩, 曹源, 王红霞, 黄伟翼. MMP14在胰腺癌中的表达及其与肿瘤免疫微环境特征的相关性研究[J]. 上海交通大学学报(医学版), 2022, 42(3): 312-322.
XU Jingxuan, DU Shaoqian, CAO Yuan, WANG Hongxia, HUANG Weiyi. MMP14 expression in pancreatic cancer and its correlation with characteristics of tumor immune microenvironment[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2022, 42(3): 312-322.
| Antibody | Source | Identifier | Usage |
|---|---|---|---|
| Anti-CD45 | BD Biosciences | Cat# 564585 | Flow cytometry |
| Anti-CD3 | BD Biosciences | Cat# 566517 | Flow cytometry |
| Anti-CD4 | BD Biosciences | Cat# 560909 | Flow cytometry |
| Anti-CD8 | BD Biosciences | Cat# 612943 | Flow cytometry |
| Anti-TCRγδ | BD Biosciences | Cat# 562511 | Flow cytometry |
| Anti-CD19 | BD Biosciences | Cat# 612917 | Flow cytometry |
| Anti-CD56 | BD Biosciences | Cat# 557919 | Flow cytometry |
| Anti-CD16 | BD Biosciences | Cat# 748850 | Flow cytometry |
| Anti-CD11b | BD Biosciences | Cat# 747357 | Flow cytometry |
| Anti-CD14 | BD Biosciences | Cat# 566465 | Flow cytometry |
| Anti-CD66b | BD Biosciences | Cat# 561645 | Flow cytometry |
| Anti-CD11c | BD Biosciences | Cat# 612968 | Flow cytometry |
| Anti-CD123 | BD Biosciences | Cat# 563072 | Flow cytometry |
| Anti-HLA-DR | BD Biosciences | Cat# 561358 | Flow cytometry |
| Anti-CD206 | BD Biosciences | Cat# 741860 | Flow cytometry |
| Anti-CD45 | Santa Cruz Biotechnology | Cat# sc-19597 | mIHC |
| Anti-CD8 | Abcam | Cat# ab237709 | mIHC |
| Anti-CD14 | Abcam | Cat# ab133335 | mIHC |
| Anti-CD68 | Abcam | Cat# ab955 | mIHC |
| Anti-MMP14 | Abcam | Cat# ab51074 | mIHC |
表1 抗体信息
Tab 1 Information of antibodies
| Antibody | Source | Identifier | Usage |
|---|---|---|---|
| Anti-CD45 | BD Biosciences | Cat# 564585 | Flow cytometry |
| Anti-CD3 | BD Biosciences | Cat# 566517 | Flow cytometry |
| Anti-CD4 | BD Biosciences | Cat# 560909 | Flow cytometry |
| Anti-CD8 | BD Biosciences | Cat# 612943 | Flow cytometry |
| Anti-TCRγδ | BD Biosciences | Cat# 562511 | Flow cytometry |
| Anti-CD19 | BD Biosciences | Cat# 612917 | Flow cytometry |
| Anti-CD56 | BD Biosciences | Cat# 557919 | Flow cytometry |
| Anti-CD16 | BD Biosciences | Cat# 748850 | Flow cytometry |
| Anti-CD11b | BD Biosciences | Cat# 747357 | Flow cytometry |
| Anti-CD14 | BD Biosciences | Cat# 566465 | Flow cytometry |
| Anti-CD66b | BD Biosciences | Cat# 561645 | Flow cytometry |
| Anti-CD11c | BD Biosciences | Cat# 612968 | Flow cytometry |
| Anti-CD123 | BD Biosciences | Cat# 563072 | Flow cytometry |
| Anti-HLA-DR | BD Biosciences | Cat# 561358 | Flow cytometry |
| Anti-CD206 | BD Biosciences | Cat# 741860 | Flow cytometry |
| Anti-CD45 | Santa Cruz Biotechnology | Cat# sc-19597 | mIHC |
| Anti-CD8 | Abcam | Cat# ab237709 | mIHC |
| Anti-CD14 | Abcam | Cat# ab133335 | mIHC |
| Anti-CD68 | Abcam | Cat# ab955 | mIHC |
| Anti-MMP14 | Abcam | Cat# ab51074 | mIHC |
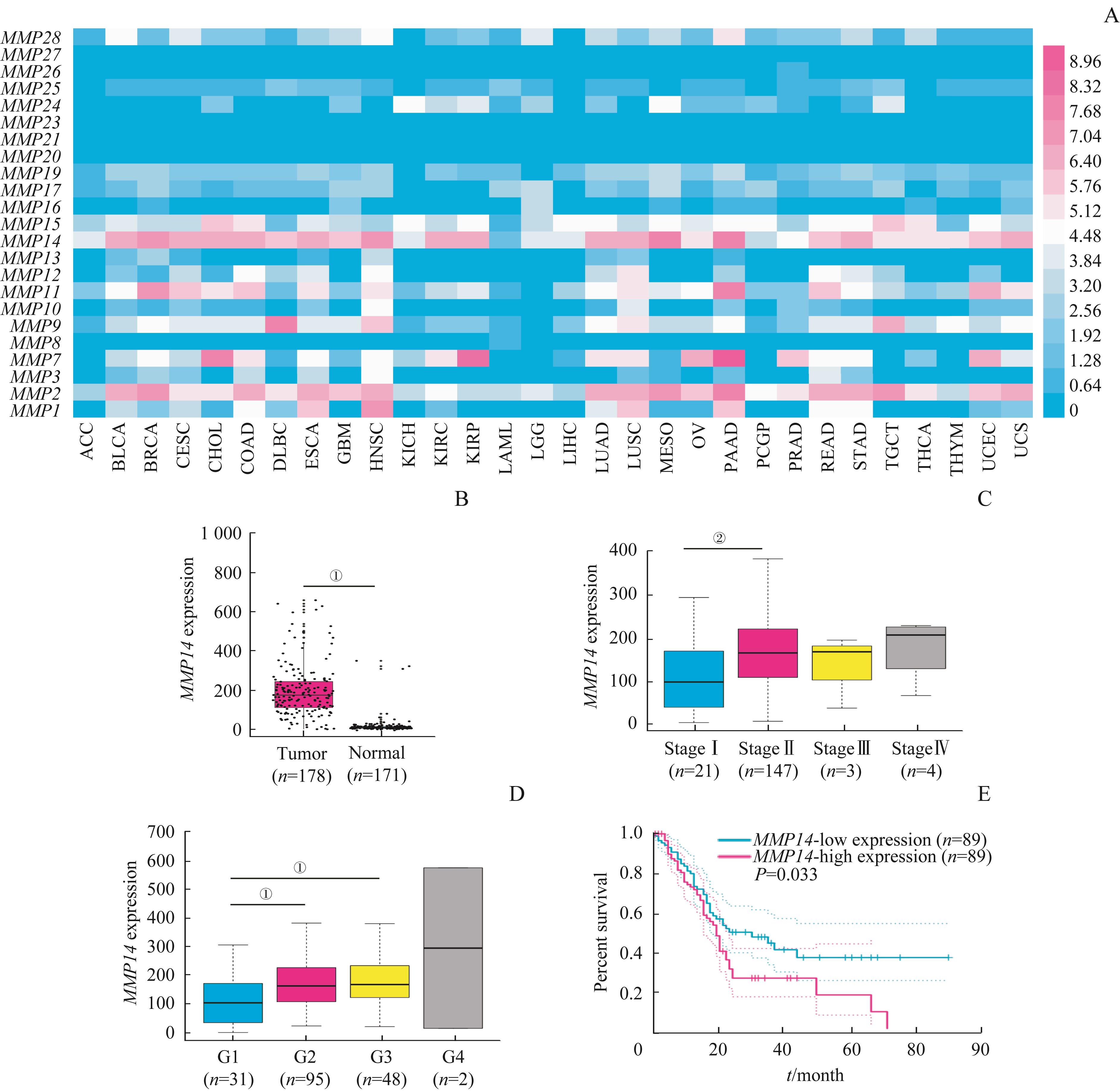
图1 生物信息学数据库中 MMP14 在胰腺癌组织中的表达情况及其与患者临床特征的相关性分析Note: A. Expression of MMPs in 30 common tumor tissues. B. MMP14 expression in the pancreatic cancer tissues and the normal tissues. C. Comparison of MMP14 expression among different TNM stages of the patients with pancreatic adenocarcinoma. D. Comparison of MMP14 expression among different grades of the patients with pancreatic adenocarcinoma. E. Overall survival analysis of MMP14-high expression group and MMP14-low expression group. ①P=0.000, ②P=0.012. ACC—adrenocortical carcinoma; BLCA—bladder urothelial carcinoma; BRCA—breast invasive carcinoma; CESC—cervical squamous cell carcinoma and endocervical adenocarcinoma; CHOL—cholangiolar carcinoma; COAD—colon adenocarcinoma; DLBC—lymphoid neoplasm diffuse large B-cell lymphoma; ESCA—esophageal carcinoma; GBM—glioblastoma multiforme; HNSC—head and neck squamous cell carcinoma; KICH—kidney chromophobe; KIRC—kidney renal clear cell carcinoma; KIRP—kidney renal papillary cell carcinoma; LAML—acute myeloid leukemia; LGG—brain lower grade glioma; LIHC—liver hepatocellular carcinoma; LUAD—lung adenocarcinoma; LUSC—lung squamous cell carcinoma; MESO—mesothelioma; OV—ovarian serous cystadenocarcinoma; PAAD—pancreatic adenocarcinoma; PCPG—pheochromocytoma and paraganglioma; PRAD—prostate adenocarcinoma; READ—rectum adenocarcinoma; STAD—stomach adenocarcinoma; TGCT—testicular germ cell tumor; THCA—thyroid carcinoma; THYM—thymoma; UCEC—uterine corpus endometrial carcinoma; UCS—uterine carcinosarcoma.
Fig 1 Bioinformatics analysis of MMP14 expression in the pancreatic cancer tissues and its correlation with the patients’ clinical characteristics

图2 TCGA数据库中MMP14信号通路和功能富集分析Note: A. KEGG pathway enrichment analysis. B. GO enrichment analysis.
Fig 2 KEGG analysis and GO analysis of MMP14 in TCGA database
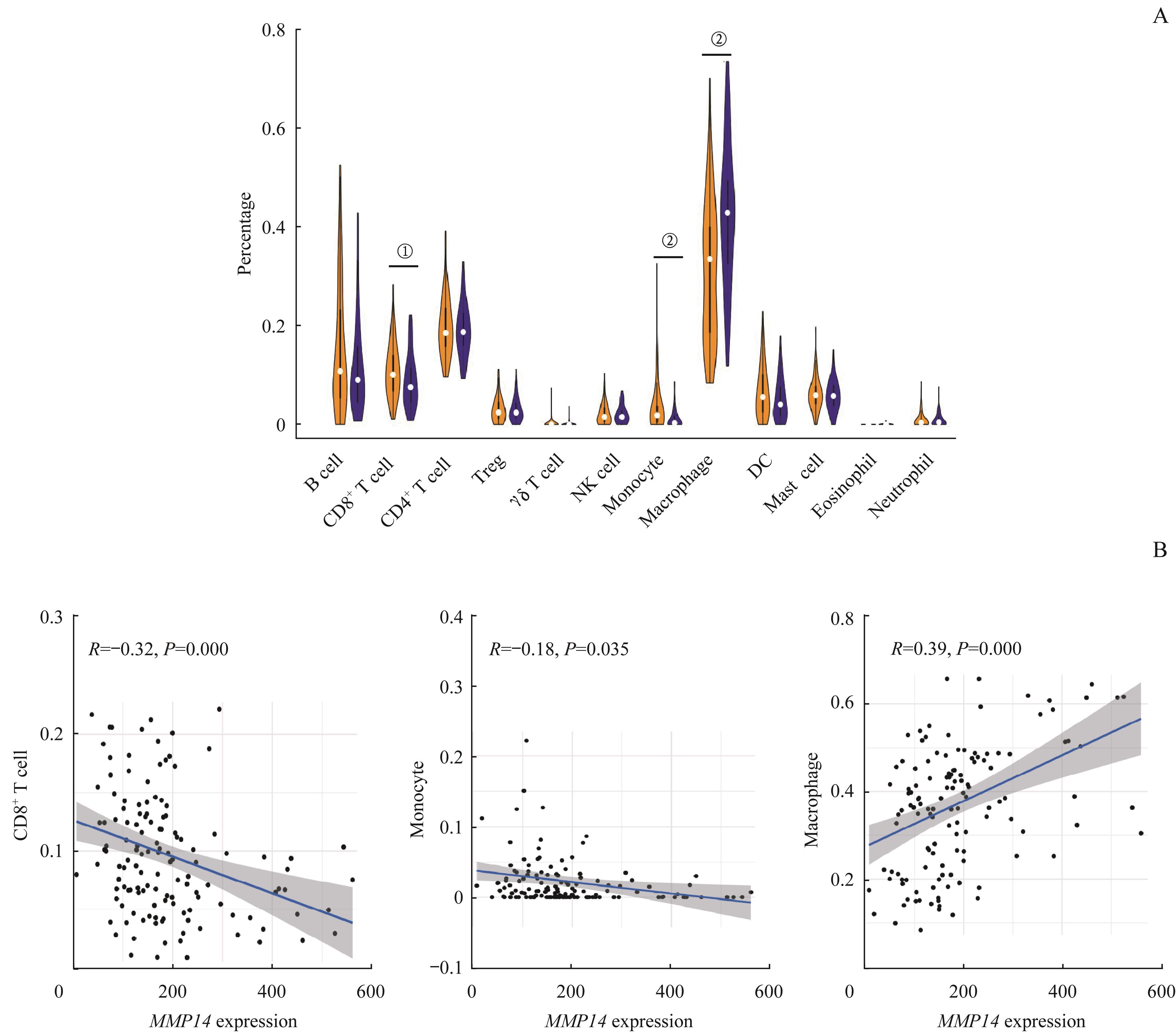
图3 TCGA数据库中胰腺癌 MMP14 不同表达水平组肿瘤浸润免疫细胞比例差异及其与 MMP14 表达的相关性Note: A. Percentage differences of immune cell subsets in MMP14-high expression group (blue) and MMP14-low expression group (yellow). B. Correlation analysis of MMP14 expression and percentage of three immune cell subsets. ①P=0.009, ②P=0.000.
Fig 3 Distribution differences of tumor-infiltrating immune cells in the pancreatic cancer with different MMP14 expression levels and the correlation between the percentage of immune cell subsets and MMP14 expression in TCGA database
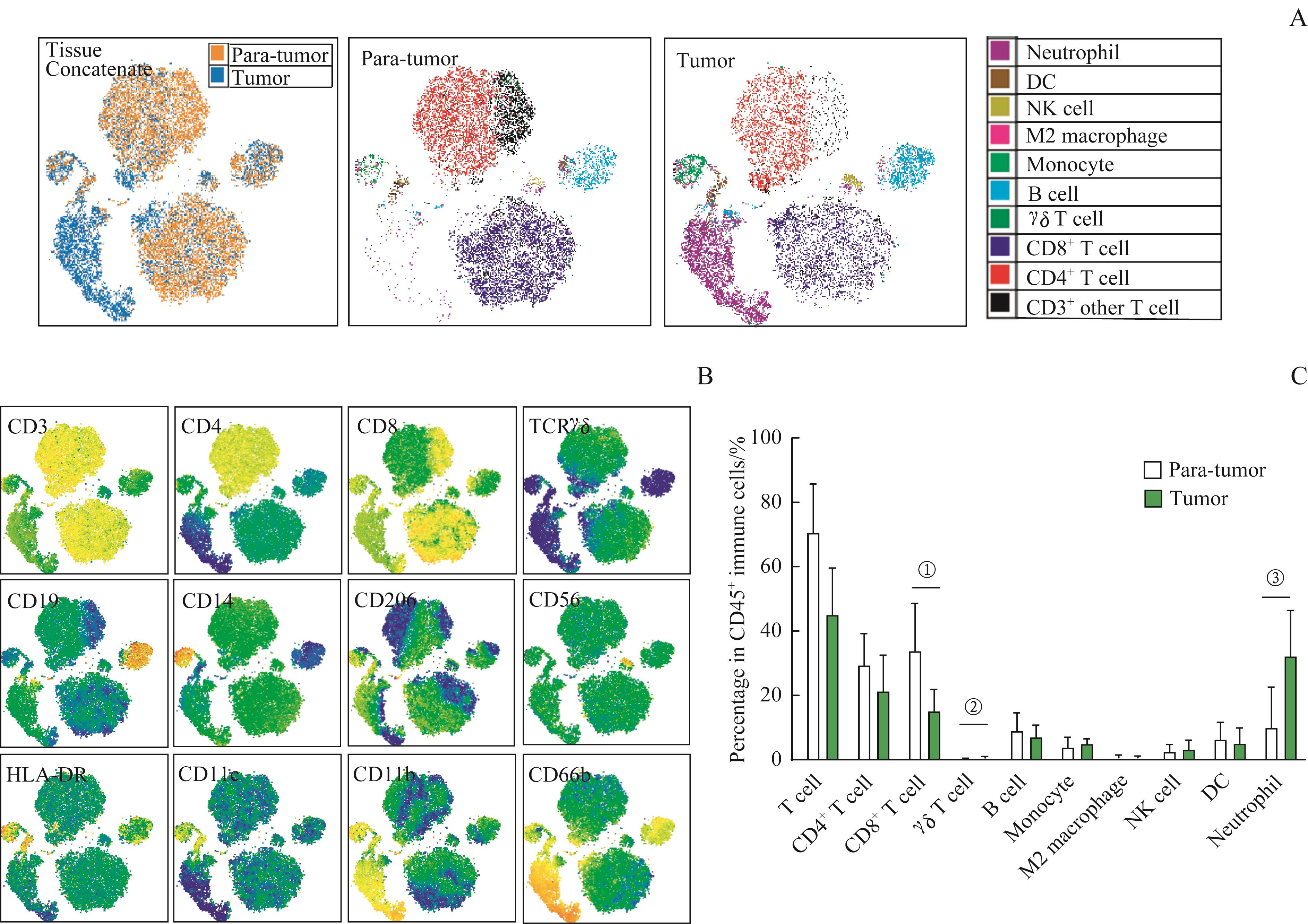
图4 胰腺癌和配对癌旁组织的免疫微环境流式细胞分析Note: A. t-SNE analysis of CD45+ immune cells from different tissues and colored by cell clusters. B. t-SNE plots of 24 000 CD45+ immune cells from a pair of tissues colored by relative expression of CD3, CD4, CD8, TCR γδ, CD19, CD14, CD206, CD56, HLA-DR, CD11c, CD11b and CD66b. C. Frequency analysis of all immune cell types for six pairs of pancreatic cancer and para-tumor tissues. ①P=0.025, ②P=0.021, ③P=0.037.
Fig 4 Flow cytometry analysis of immune microenvironment in pancreatic cancer and paired para-tumor tissues

图5 MMP14在胰腺癌组织中的表达及其与免疫微环境相关性的分析Note: A. IHC analysis of MMP14 expression in the pancreatic cancer and paired para-tumor tissues of a representative patient. Scale bar=200 μm. B. IHC scores of MMP14 expression in pancreatic cancer and paired para-tumor tissues. C. Comparison of MMP14 expression among different TNM stages of patients. D. Comparison of MMP14 expression among different grades of patients. E. mIHC images of two representative patients with different MMP14 expression using MMP14 (green), CD45 (purple), CD8 (red), CD14 (orange), CD68 (yellow) and DNA (blue) markers. The white arrows show CD8+ T cells. The yellow arrows show CD68+ macrophages. Scale bar=200 μm (upper). Scale bar=20 μm (lower). F. Frequency analysis of CD8+ T cells, CD68+ macrophages and CD14+ monocytes in MMP14-high expression group and MMP14-low expression group. ①P=0.000, ②P=0.017, ③P=0.006, ④P=0.022, ⑤P=0.030, ⑥P=0.018,⑦P=0.001.
Fig 5 Analysis of MMP14 expression in the pancreatic cancer tissues and its correlation with immune microenvironment
| 1 | ANSARI D, TINGSTEDT B, ANDERSSON B, et al. Pancreatic cancer: yesterday, today and tomorrow[J]. Future Oncol, 2016, 12(16): 1929-1946. |
| 2 | PISHVAIAN M J, BLAIS E M, BRODY J R, et al. Overall survival in patients with pancreatic cancer receiving matched therapies following molecular profiling: a retrospective analysis of the Know Your Tumor registry trial[J]. Lancet Oncol, 2020, 21(4): 508-518. |
| 3 | 王超, 宁克, 胡欢欢, 等. 胰腺癌肿瘤微环境的研究进展[J]. 中华消化外科杂志, 2020, 19(1): 109-112. |
| 4 | LI H B, YANG Z H, GUO Q Q. Immune checkpoint inhibition for pancreatic ductal adenocarcinoma: limitations and prospects: a systematic review[J]. Cell Commun Signal, 2021, 19(1): 117. |
| 5 | DANGAJ D, BRUAND M, GRIMM A J, et al. Cooperation between constitutive and inducible chemokines enables T cell engraftment and immune attack in solid tumors[J]. Cancer Cell, 2019, 35(6): 885-900.e10. |
| 6 | SHI B, CHU J F, HUANG T, et al. The scavenger receptor MARCO expressed by tumor-associated macrophages are highly associated with poor pancreatic cancer prognosis[J]. Front Oncol, 2021, 11: 771488. |
| 7 | AGER C R, BODA A, RAJAPAKSHE K, et al. High potency STING agonists engage unique myeloid pathways to reverse pancreatic cancer immune privilege[J]. J Immunother Cancer, 2021, 9(8): e003246. |
| 8 | KAUR K, KO M W, CHEN F, et al. Defective NK cell expansion, cytotoxicity, and lack of ability to differentiate tumors from a pancreatic cancer patient in a long term follow-up: implication in the progression of cancer[J]. Cancer Immunol Immunother, 2021. DOI: 10.1007/s00262-021-03044-w. |
| 9 | GUO J, LIAO M F, HU X M, et al. Tumour-derived Reg3A educates dendritic cells to promote pancreatic cancer progression[J]. Mol Cells, 2021, 44(9): 647-657. |
| 10 | OSTIOS-GARCIA L, VILLAMAYOR J, GARCIA-LORENZO E, et al. Understanding the immune response and the current landscape of immunotherapy in pancreatic cancer[J]. World J Gastroenterol, 2021, 27(40): 6775-6793. |
| 11 | MÄÄTTÄ M, SOINI Y, LIAKKA A, et al. Differential expression of matrix metalloproteinase (MMP)-2, MMP-9, and membrane type 1-MMP in hepatocellular and pancreatic adenocarcinoma: implications for tumor progression and clinical prognosis[J]. Clin Cancer Res, 2000, 6(7): 2726-2734. |
| 12 | DECOTRET L R, WADSWORTH B J, LI L V, et al. Receptor-type protein tyrosine phosphatase alpha (PTPα) mediates MMP14 localization and facilitates triple-negative breast cancer cell invasion[J]. Mol Biol Cell, 2021, 32(7): 567-578. |
| 13 | YU J, HE Z, HE X W, et al. Comprehensive analysis of the expression and prognosis for MMPs in human colorectal cancer[J]. Front Oncol, 2021, 11: 771099. |
| 14 | HILLEBRAND L E, WICKBERG S M, GOMEZ-AULI A, et al. MMP14 empowers tumor-initiating breast cancer cells under hypoxic nutrient-depleted conditions[J]. FASEB J, 2019, 33(3): 4124-4140. |
| 15 | ULASOV I V, MIJANOVIC O, SAVCHUK S, et al. TMZ regulates GBM stemness via MMP14-DLL4-Notch3 pathway[J]. Int J Cancer, 2020, 146(8): 2218-2228. |
| 16 | QIANG L, CAO H, CHEN J, et al. Pancreatic tumor cell metastasis is restricted by MT1-MMP binding protein MTCBP-1[J]. J Cell Biol, 2019, 218(1): 317-332. |
| 17 | 袁蒙, 阿卜杜海拜尔·萨杜拉, 任思谦, 等. 胰腺癌免疫微环境特点与相关免疫治疗策略[J]. 中华医学杂志, 2021, 101(12): 831-835. |
| 18 | OH D Y, KWEK S S, RAJU S S, et al. Intratumoral CD4+ T cells mediate anti-tumor cytotoxicity in human bladder cancer[J]. Cell, 2020, 181(7): 1612-1625.e13. |
| 19 | DI PILATO M, KFURI-RUBENS R, PRUESSMANN J N, et al. CXCR6 positions cytotoxic T cells to receive critical survival signals in the tumor microenvironment[J]. Cell, 2021, 184(17): 4512-4530.e22. |
| 20 | DALEY D, ZAMBIRINIS C P, SEIFERT L, et al. γδ T cells support pancreatic oncogenesis by restraining αβ T cell activation[J]. Cell, 2016, 166(6): 1485-1499.e15. |
| 21 | MILLER-OCUIN J L, LIANG X Y, BOONE B A, et al. DNA released from neutrophil extracellular traps (NETs) activates pancreatic stellate cells and enhances pancreatic tumor growth[J]. Oncoimmunology, 2019, 8(9): e1605822. |
| 22 | POINCLOUX R, LIZÁRRAGA F, CHAVRIER P. Matrix invasion by tumour cells: a focus on MT1-MMP trafficking to invadopodia[J]. J Cell Sci, 2009, 122(Pt 17): 3015-3024. |
| 23 | SATHYAMOORTHY T, TEZERA L B, WALKER N F, et al. Membrane type 1 matrix metalloproteinase regulates monocyte migration and collagen destruction in tuberculosis[J]. J Immunol, 2015, 195(3): 882-891. |
| 24 | LING B B, WATT K, BANERJEE S, et al. A novel immunotherapy targeting MMP-14 limits hypoxia, immune suppression and metastasis in triple-negative breast cancer models[J]. Oncotarget, 2017, 8(35): 58372-58385. |
| 25 | ANDREOU T, WILLIAMS J, BROWNLIE R J, et al. Hematopoietic stem cell gene therapy targeting TGFβ enhances the efficacy of irradiation therapy in a preclinical glioblastoma model[J]. J Immunother Cancer, 2021, 9(3): e001143. |
| 26 | FARHOOD B, NAJAFI M, MORTEZAEE K. CD8+ cytotoxic T lymphocytes in cancer immunotherapy: a review[J]. J Cell Physiol, 2019, 234(6): 8509-8521. |
| 27 | XIA Q, JIA J, HU C P, et al. Tumor-associated macrophages promote PD-L1 expression in tumor cells by regulating PKM2 nuclear translocation in pancreatic ductal adenocarcinoma[J]. Oncogene, 2022, 41(6): 865-877. |
| 28 | HALBROOK C J, PONTIOUS C, KOVALENKO I, et al. Macrophage-released pyrimidines inhibit gemcitabine therapy in pancreatic cancer[J]. Cell Metab, 2019, 29(6): 1390-1399.e6. |
| 29 | CAO D J, SONG Q Q, LI J Q, et al. Opportunities and challenges in targeted therapy and immunotherapy for pancreatic cancer[J]. Expert Rev Mol Med, 2021, 23: e21. |
| [1] | 孙晨玮, 海汪溪, 屈骞, 席云. [18F]F-FMISO和[18F]F-FLT PET/CT双核素显像预测胰腺癌耐药性的体内研究[J]. 上海交通大学学报(医学版), 2025, 45(1): 60-68. |
| [2] | 胡飞, 蔡晓涵, 程睿, 季诗雨, 苗嘉欣, 朱晏, 范广建. 骨肉瘤免疫微环境及其免疫治疗临床转化研究进展[J]. 上海交通大学学报(医学版), 2024, 44(7): 814-821. |
| [3] | 俞思薇, 徐梓淇, 陶梦玉, 范广建. 脂肪酸代谢紊乱通过上调ZNF143促进胰腺癌进展的机制研究[J]. 上海交通大学学报(医学版), 2024, 44(10): 1255-1265. |
| [4] | 杜少倩, 陶梦玉, 曹源, 王红霞, 胡孝渠, 范广建, 臧丽娟. CXCL9在乳腺癌中的表达及其与肿瘤免疫浸润特征的相关性研究[J]. 上海交通大学学报(医学版), 2023, 43(7): 860-872. |
| [5] | 秦雅含, 张珂, 张梦雨, 沈洁, 彭美玉. MDSC靶向免疫治疗胰腺癌的研究进展[J]. 上海交通大学学报(医学版), 2023, 43(10): 1317-1323. |
| [6] | 马芳芳, 秦洁洁, 任灵杰, 唐笑梅, 刘佳, 施敏敏, 蒋玲曦. 基于水凝胶微球建立胰腺癌原代细胞的3D培养模型[J]. 上海交通大学学报(医学版), 2023, 43(1): 79-87. |
| [7] | 张修齐, 沈柏用. 胰腺导管腺癌神经侵袭的细胞学机制研究进展[J]. 上海交通大学学报(医学版), 2022, 42(6): 833-838. |
| [8] | 王建茹, 彭广操, 朱明军. 基于GEO数据库和生物信息学分析筛选小鼠心肌缺血再灌注损伤相关的潜在枢纽基因[J]. 上海交通大学学报(医学版), 2022, 42(1): 51-62. |
| [9] | 刘俐, 耿子龙, 陈嘉焕, 张沙沙, 张冰. 血管内皮生长因子A调控人脐静脉内皮细胞miRNA的全基因表达谱分析[J]. 上海交通大学学报(医学版), 2021, 41(9): 1183-1189. |
| [10] | 李静威, 王俐文, 蒋玲曦, 詹茜, 陈皓, 沈柏用. 胰腺癌免疫抑制性肿瘤微环境研究综述[J]. 上海交通大学学报(医学版), 2021, 41(8): 1103-1108. |
| [11] | 杨鹿笛, 王高明, 胡仁豪, 蒋小华, 崔然. 生物信息学方法筛选胰腺癌进展相关的核心基因[J]. 上海交通大学学报(医学版), 2021, 41(5): 571-578. |
| [12] | 徐康力1,马亚妮2,王筱金3,苗彦彦1,韩 达1#,谭蔚泓1#. 核酸适配体sgc8在急性白血病诊断中的应用研究[J]. 上海交通大学学报(医学版), 2020, 40(9): 1157-1167. |
| [13] | 高境泽,吴 霞. 卵巢肿瘤组织中CXCL9 mRNA表达与患者的预后、免疫微环境特征的相关性研究[J]. 上海交通大学学报(医学版), 2020, 40(4): 457-. |
| [14] | 张伟然1, 2,林雪峰3,李 鑫2,张 浩2,王 猛2,孙 伟2,韩兴鹏2,孙大强1, 4. 转录组分析鉴定肺腺癌潜在的生物标志物[J]. 上海交通大学学报(医学版), 2020, 40(12): 1598-1606. |
| [15] | 梁雨,江明杰,田聆. 前列腺素 E 2重塑胰腺肿瘤微环境的作用机制研究进展[J]. 上海交通大学学报(医学版), 2019, 39(8): 923-. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||