
上海交通大学学报(医学版) ›› 2025, Vol. 45 ›› Issue (9): 1079-1098.doi: 10.3969/j.issn.1674-8115.2025.09.001
• 指南与共识 • 下一篇
超声引导儿童神经阻滞中国专家共识(2025版)编写组
收稿日期:2025-05-05
接受日期:2025-08-19
出版日期:2025-09-28
发布日期:2025-09-30
通讯作者:
许 涛,主任医师,博士;电子信箱:balor@sjtu.edu.cn。基金资助:Writing Group of Chinese Expert Consensus on Ultrasound-Guided Pediatric Nerve Blocks in Children (2025 edition)
Received:2025-05-05
Accepted:2025-08-19
Online:2025-09-28
Published:2025-09-30
Contact:
XU Tao, E-mail: balor@sjtu.edu.cn.Supported by:摘要:
超声引导儿童神经阻滞的研究近年来取得重要进展,其安全性和有效性的提高得益于高精度超声可视化技术。超声技术在临床上的应用和普及,使得临床医师能够清晰、个体化地辨识儿童的神经结构和周围组织,能实时地观察到药物的扩散,显著降低了传统盲穿法带来的并发症风险。该共识基于循证医学证据和临床实践经验,结合超声引导儿童神经阻滞的发展历程和现状,系统论述儿童神经解剖学特点及其对阻滞技术的影响;明确儿童神经阻滞的适应证和禁忌证;规范实施神经阻滞前的设备准备、药物配置和儿童镇静方案;详细阐述不同部位神经阻滞的实施步骤和技术要点,包括探头选择、进针路径和局部麻醉药物扩散的实时监测;分析了主要并发症及相应的预防处理策略。经专家组深入讨论,根据共同决定的规则形成了推荐意见,最终制定了共识,以期对临床麻醉和疼痛诊疗中超声引导儿童神经阻滞的实施提供实践参考,从而推动超声引导儿童神经阻滞在临床实践中更安全有效的应用,最终实现减轻儿童痛苦、加速术后康复的目标。
中图分类号:
超声引导儿童神经阻滞中国专家共识(2025版)编写组. 超声引导儿童神经阻滞中国专家共识(2025版)[J]. 上海交通大学学报(医学版), 2025, 45(9): 1079-1098.
Writing Group of Chinese Expert Consensus on Ultrasound-Guided Pediatric Nerve Blocks in Children (2025 edition). Chinese expert consensus on ultrasound-guided nerve blocks in children (2025 edition)[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2025, 45(9): 1079-1098.
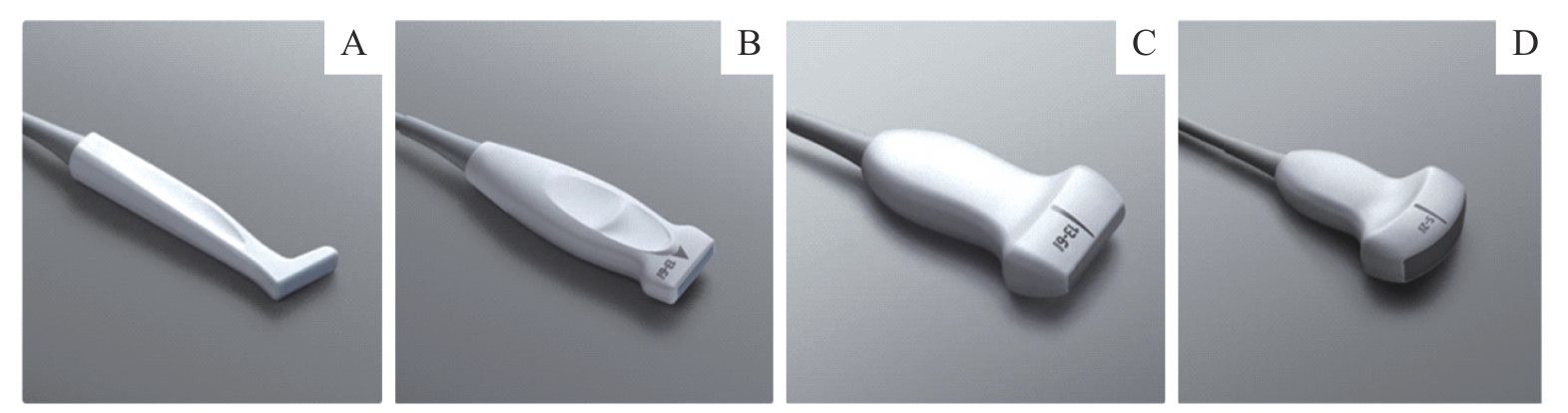
图1 儿童神经阻滞常用超声探头Note: A. 2.5 cm高频线阵探头(L型)/2.5 cm L-type high-frequency linear array probe. B. 2.5 cm高频线阵探头/2.5 cm high-frequency linear array probe. C. 3.5 cm高频线阵探头/3.5 cm high-frequency linear array probe. D. 低频凸阵探头/low-frequency convex array probe.
Fig 1 Ultrasound probes commonly used for nerve blocks in children
阻滞区域 Block region | 首选方案 Primary plan | 升级方案 Advanced plan |
|---|---|---|
上肢 Upper limb | ||
肩部以下 Below shoulder | 腋路臂丛阻滞 Axillary brachial plexus block | 锁骨上臂丛阻滞、锁骨下臂丛阻滞 Supraclavicular brachial plexus block; infraclavicular brachial plexus block |
肘部以下 Below elbow | 肘平面阻滞 Elbow blocks | |
下肢 Lower limb | ||
髋部 Hip | 股神经阻滞 Femoral nerve block | 髂筋膜阻滞、腰丛阻滞 Fascia iliaca block; lumbar plexus block |
大腿及膝部 Thigh and knee | 收肌管阻滞 Adductor canal block | |
膝下至足踝 Below knee | 腘窝坐骨神经阻滞 Sciatic nerve block of popliteal fossa | 踝部阻滞 Ankle block |
躯干 Trunk | ||
胸壁 Chest wall | 尚无推荐 No recommendations | 竖脊肌阻滞、椎旁阻滞、前锯肌平面阻滞 Erector spinae plane block; paravertebral block; serratus anterior plane block |
腹部、腹股沟区 Abdomen,groin | 腹直肌鞘阻滞、腰方肌外侧平面阻滞、阴茎背神经阻滞 Rectus sheath block; lateral quadratus lumborum block; dorsal penile nerve block | 前路腰方肌阻滞、腹横肌平面阻滞、阴部神经阻滞 Anterior quadratus lumborum block; transversus abdominis plane block; pudendal nerve block |
头颈部 Head and neck | ||
颈前区 Anterior region of neck | 颈浅丛阻滞 Superficial cervical plexus block | 尚无推荐 No recommendations |
耳 Ear | 耳大神经阻滞 Great auricular nerve block |
表1 超声引导儿童神经阻滞推荐方案的分级
Tab 1 Grading of recommended protocols for ultrasound-guided pediatric nerve blocks
阻滞区域 Block region | 首选方案 Primary plan | 升级方案 Advanced plan |
|---|---|---|
上肢 Upper limb | ||
肩部以下 Below shoulder | 腋路臂丛阻滞 Axillary brachial plexus block | 锁骨上臂丛阻滞、锁骨下臂丛阻滞 Supraclavicular brachial plexus block; infraclavicular brachial plexus block |
肘部以下 Below elbow | 肘平面阻滞 Elbow blocks | |
下肢 Lower limb | ||
髋部 Hip | 股神经阻滞 Femoral nerve block | 髂筋膜阻滞、腰丛阻滞 Fascia iliaca block; lumbar plexus block |
大腿及膝部 Thigh and knee | 收肌管阻滞 Adductor canal block | |
膝下至足踝 Below knee | 腘窝坐骨神经阻滞 Sciatic nerve block of popliteal fossa | 踝部阻滞 Ankle block |
躯干 Trunk | ||
胸壁 Chest wall | 尚无推荐 No recommendations | 竖脊肌阻滞、椎旁阻滞、前锯肌平面阻滞 Erector spinae plane block; paravertebral block; serratus anterior plane block |
腹部、腹股沟区 Abdomen,groin | 腹直肌鞘阻滞、腰方肌外侧平面阻滞、阴茎背神经阻滞 Rectus sheath block; lateral quadratus lumborum block; dorsal penile nerve block | 前路腰方肌阻滞、腹横肌平面阻滞、阴部神经阻滞 Anterior quadratus lumborum block; transversus abdominis plane block; pudendal nerve block |
头颈部 Head and neck | ||
颈前区 Anterior region of neck | 颈浅丛阻滞 Superficial cervical plexus block | 尚无推荐 No recommendations |
耳 Ear | 耳大神经阻滞 Great auricular nerve block |
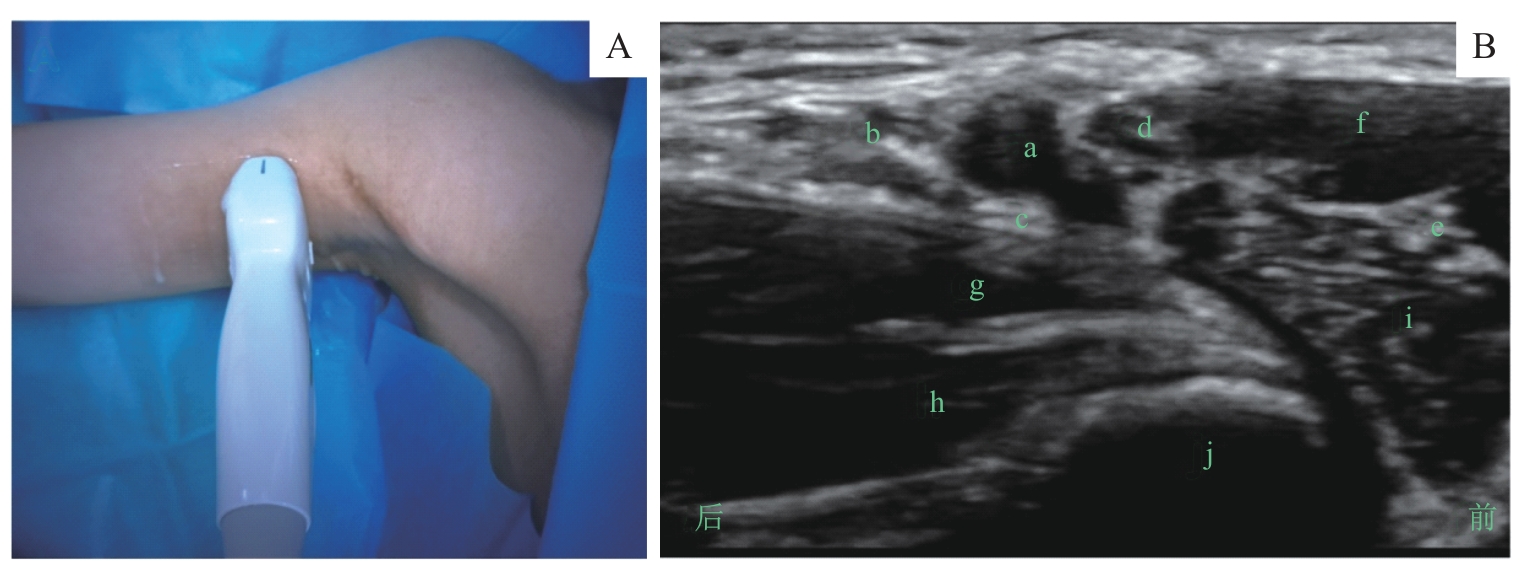
图2 腋路臂丛阻滞的超声定位和影像Note: A. 超声探头体表扫描定位/Surface scanning for ultrasound probe positioning. B. 探头处于图A位置时的腋路臂丛超声影像/Ultrasound image of the axillary brachial plexus obtained with the probe positioned as shown in figure A. a—腋动脉/axillary artery; b—尺神经/ulnar nerve; c—桡神经/radial nerve; d—正中神经/median nerve; e—肌皮神经/musculocutaneous nerve; f—肱二头肌/biceps brachii muscle; g—背阔肌大圆肌联合腱/the latissimus dorsi and teres major tendons; h—肱三头肌/triceps brachii muscle; i—喙肱肌/brachii muscle; j—肱骨/brachialis muscle.
Fig 2 Ultrasound positioning and imaging of the axillary brachial plexus block
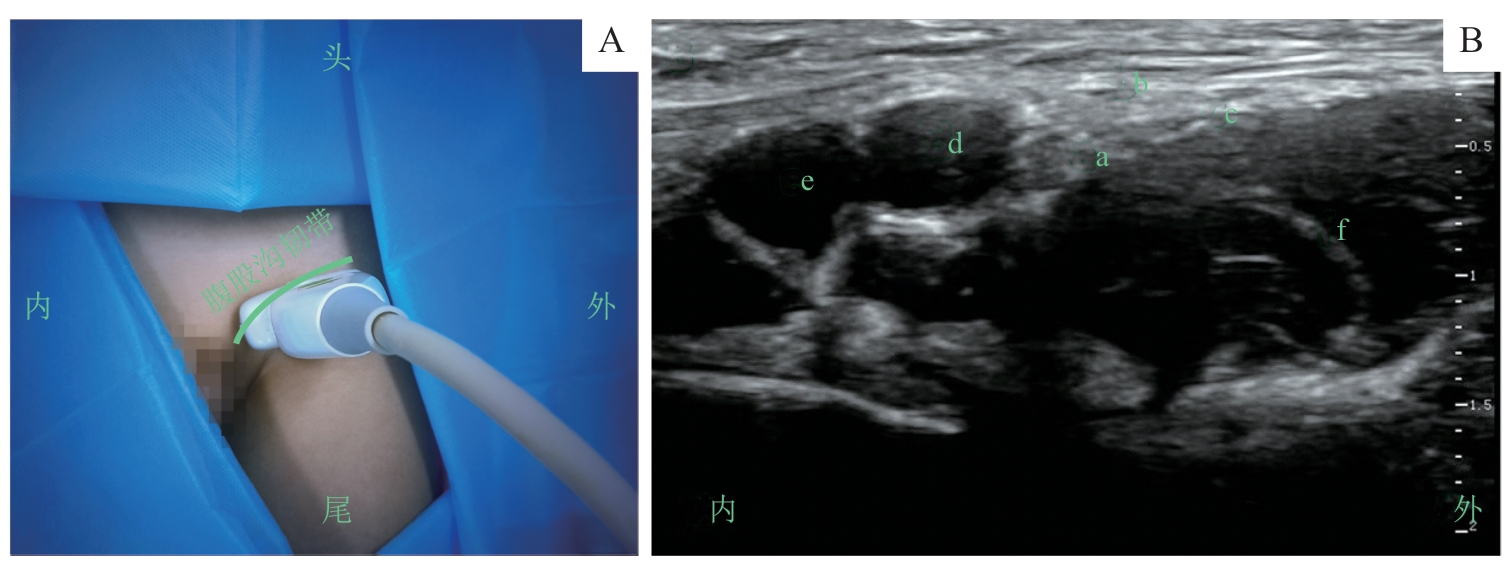
图3 股神经阻滞的超声定位和影像Note: A. 超声探头体表扫描定位/Surface scanning for ultrasound probe positioning. B. 探头处于图A位置时的股神经超声影像/Ultrasound image of the femoral nerve obtained with the probe positioned as shown in figure A. a—股神经/femoral nerve; b—阔筋膜/fascia lata; c—髂筋膜/fascia iliac; d—股动脉/femoral artery; e—股静脉/femoral vein; f—髂腰肌/iliopsoas muscle.
Fig 3 Ultrasound positioning and imaging of the femoral nerve block
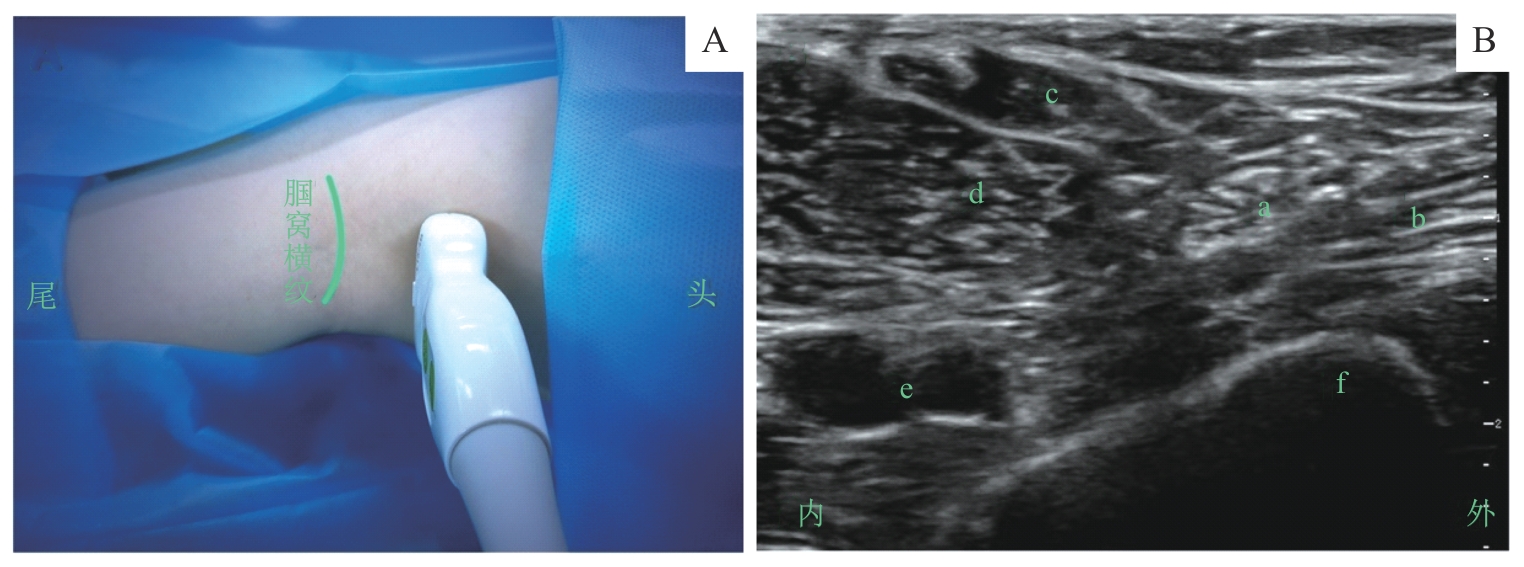
图4 腘窝坐骨神经阻滞的超声定位和影像Note: A. 超声探头体表扫描定位/Surface scanning for ultrasound probe positioning. B. 探头处于图A位置时的腘窝坐骨神经超声影像/Ultrasound image of the sciatic nerve in the popliteal fossa obtained with the probe positioned as shown in figure A. a—坐骨神经/sciatic nerve; b—股二头肌/biceps femoris muscle; c—半腱肌/semitendinosus muscle; d—半膜肌/semimembranosus muscle; e—腘动、静脉/popliteal artery and vein; f—股骨/femur.
Fig 4 Ultrasound positioning and imaging of the sciatic nerve block via the popliteal fossa
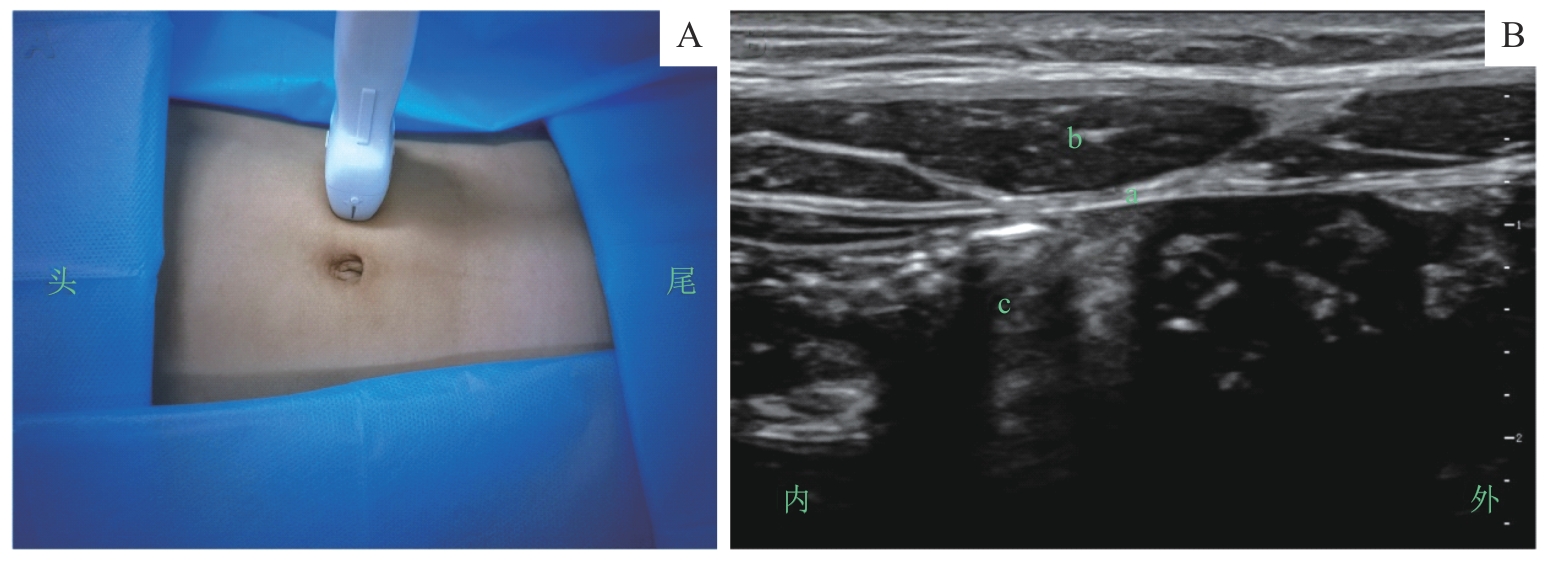
图5 腹直肌鞘阻滞的超声定位和影像Note: A. 超声探头体表扫描定位/Surface scanning for ultrasound probe positioning. B. 探头处于图A位置时的腹直肌鞘超声影像/Ultrasound image of the rectus sheath obtained with the probe positioned as shown in figure A. a—腹直肌后鞘/posterior sheath of rectus abdominis muscle; b—腹直肌/rectus abdominis muscle; c—腹腔/abdominal cavity.
Fig 5 Ultrasound positioning and imaging of the rectus sheath block
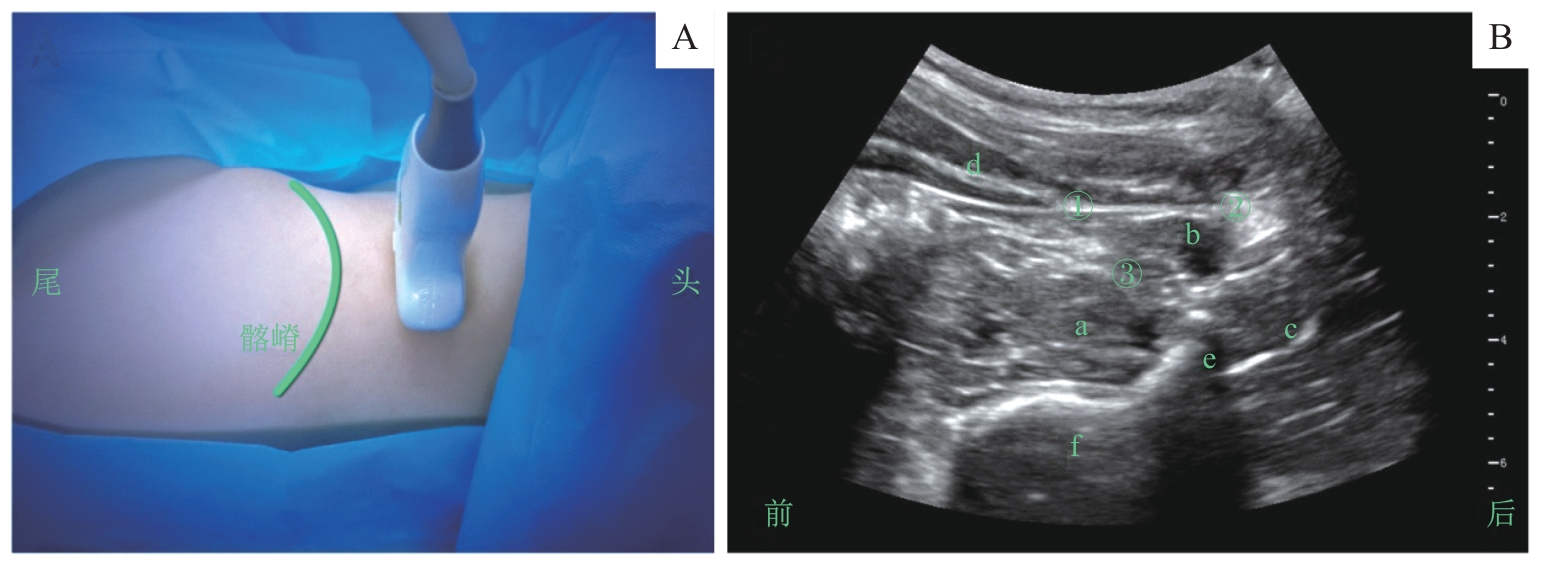
图6 腰方肌阻滞的超声定位和影像Note: A.超声探头体表扫描定位/Surface scanning for ultrasound probe positioning. B. 探头处于图A位置时的腰方肌超声影像/Ultrasound image of the quadratus lumborum obtained with the probe positioned as shown in figure A. a—腰大肌/psoas muscle; b—腰方肌/quadratus lumborum muscle; c—竖脊肌/quadratus lumborum muscle; d—腹肌/abdominal muscle; e—横突/transverse process; f—椎体/vertebral body; ① 腰方肌阻滞外侧点/needle insertion site for lateral quadratus lumborum block; ② 腰方肌阻滞后点/needle insertion site for posterior quadratus lumborum block; ③ 腰方肌阻滞前点/needle insertion site for anterior quadratus lumborum block.
Fig 6 Ultrasound positioning and imaging of the quadratus lumborum block
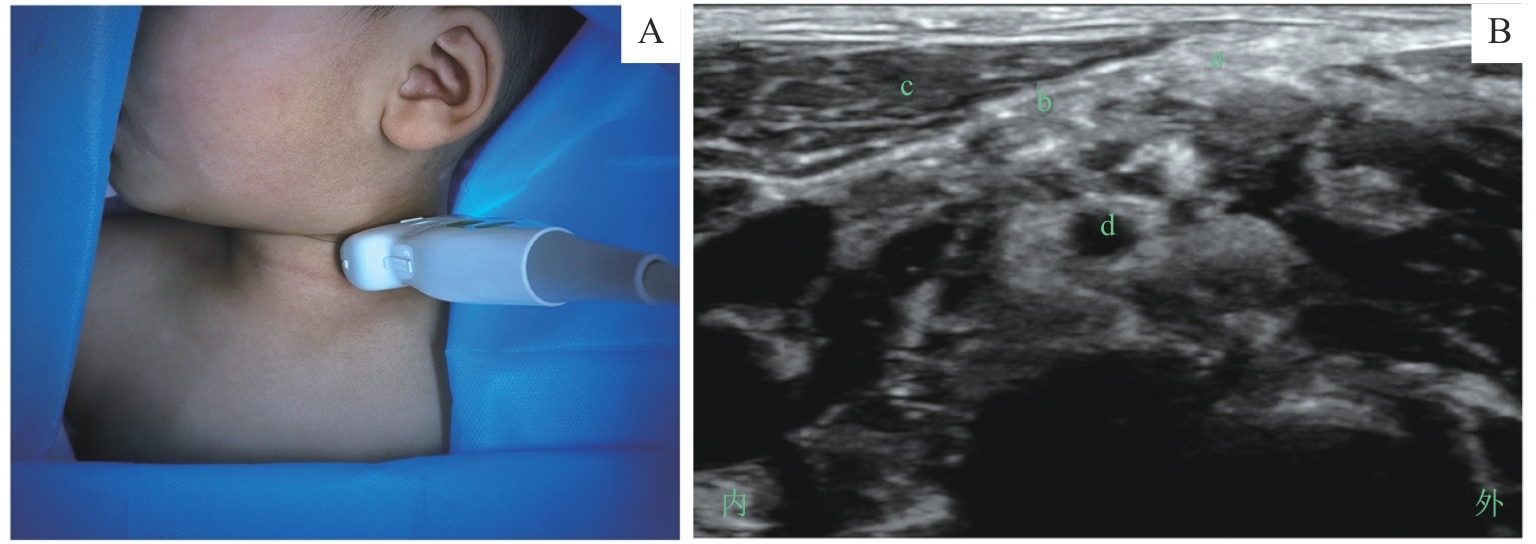
图7 颈浅丛阻滞的超声定位和影像Note: A. 超声探头体表扫描定位/Surface scanning for ultrasound probe positioning. B. 探头处于图A位置时的颈浅丛超声影像/Ultrasound image of the superficial cervical plexus obtained with the probe positioned as shown in figure A. a—颈浅丛/superficial cervical plexus; b—颈深筋膜/deep cervical fascia; c—胸锁乳突肌/sternocleidomastoid muscle; d—C5神经根/C5-nerve root.
Fig 7 Ultrasound positioning and imaging of the superficial cervical plexus block
局麻药 Local anaesthetics | 最大剂量/(mg·kg-1) Maximum allowable dose/(mg·kg-1) | 外周神经和躯干阻滞单次推注 Bolus for peripheral and truncal block | 连续阻滞持续推注 Infusion for continuous block | ||
|---|---|---|---|---|---|
质量浓度/[g·(100 mL)-1] Mass concentration/ [g·(100 mL)-1] | 容量/(mg·kg-1) Volume/(mg·kg-1) | 质量浓度/[g·(100 mL)-1] Mass concentration/ [g·(100 mL)-1] | 速率/[mg·(kg·h)-1] Rate/[mg·(kg·h)-1] | ||
罗哌卡因 Ropivacaine | 2.5 | 0.2 | 0.5 | 0.2/0.1 | 0.4 |
左旋布比卡因 Levobupivacaine | 2.5 | 0.25 | 0.5 | 0.125 | 0.4 |
表2 常用局麻药的推荐剂量[84]
Tab 2 Recommended dosages of common local anaesthetics[84]
局麻药 Local anaesthetics | 最大剂量/(mg·kg-1) Maximum allowable dose/(mg·kg-1) | 外周神经和躯干阻滞单次推注 Bolus for peripheral and truncal block | 连续阻滞持续推注 Infusion for continuous block | ||
|---|---|---|---|---|---|
质量浓度/[g·(100 mL)-1] Mass concentration/ [g·(100 mL)-1] | 容量/(mg·kg-1) Volume/(mg·kg-1) | 质量浓度/[g·(100 mL)-1] Mass concentration/ [g·(100 mL)-1] | 速率/[mg·(kg·h)-1] Rate/[mg·(kg·h)-1] | ||
罗哌卡因 Ropivacaine | 2.5 | 0.2 | 0.5 | 0.2/0.1 | 0.4 |
左旋布比卡因 Levobupivacaine | 2.5 | 0.25 | 0.5 | 0.125 | 0.4 |
常用神经阻滞方法 Common nerve block technique | 适应证 Indication | 0.2%罗哌卡因 0.2% Ropivacaine |
|---|---|---|
腋路臂丛阻滞 Axillary brachial plexus block | 肘切开复位内固定、前臂和手外科手术 Elbow open reduction and internal fixation; forearm and hand surgery | 0.2‒0.5 mL·kg-1 (最多15 mL/up to 15 mL) |
股神经阻滞 Femoral nerve block | 股骨骨折、股骨上段骨骺滑脱、股骨截骨术 Femoral fracture; slipped upper femoral epiphysis; femoral osteotomy | 0.2‒0.5 mL·kg-1 (最多15 mL/up to 15 mL) |
腘窝坐骨神经阻滞 Popliteal sciatic nerve block | 肌腱转移/延长、下肢创伤、胫骨截骨术、踝关节成形术、畸形足修复 Tendon transfers/lengthening; lower limb trauma; tibial osteotomy; ankle arthroplasty; club foot repair | 0.2‒0.3 mL·kg-1 (最多15 mL/up to 15 mL) |
腹直肌鞘阻滞 Rectus sheath block | 脐疝修补术、幽门环肌切开术、开放性胃造口术 Umbilical herniotomy; pyloromyotomy; open gastrostomy | 0.1‒0.3 mL·kg-1 (单侧/per side) |
外侧腰方肌入路阻滞 Lateral quadratus lumborum block | 腹股沟疝修补术、开放性阑尾切除术 Inguinalherniotomy; open appendicectomy | 0.5 mL·kg-1 (单侧最多20 mL/up to 20 mL per side) |
阴茎背神经阻滞 Dorsal penile nerve block | 包皮环切术、远端尿道下裂修复术 Circumcision; distal hypospadias repair | 0.1 mL·kg-1 (双侧最多5 mL/up to 5 mL both sides) |
表3 常用儿童神经阻滞的适应证及局麻药的推荐剂量[41]
Tab 3 Indications and recommended local anaesthetic doses for common pediatric nerve blocks[41]
常用神经阻滞方法 Common nerve block technique | 适应证 Indication | 0.2%罗哌卡因 0.2% Ropivacaine |
|---|---|---|
腋路臂丛阻滞 Axillary brachial plexus block | 肘切开复位内固定、前臂和手外科手术 Elbow open reduction and internal fixation; forearm and hand surgery | 0.2‒0.5 mL·kg-1 (最多15 mL/up to 15 mL) |
股神经阻滞 Femoral nerve block | 股骨骨折、股骨上段骨骺滑脱、股骨截骨术 Femoral fracture; slipped upper femoral epiphysis; femoral osteotomy | 0.2‒0.5 mL·kg-1 (最多15 mL/up to 15 mL) |
腘窝坐骨神经阻滞 Popliteal sciatic nerve block | 肌腱转移/延长、下肢创伤、胫骨截骨术、踝关节成形术、畸形足修复 Tendon transfers/lengthening; lower limb trauma; tibial osteotomy; ankle arthroplasty; club foot repair | 0.2‒0.3 mL·kg-1 (最多15 mL/up to 15 mL) |
腹直肌鞘阻滞 Rectus sheath block | 脐疝修补术、幽门环肌切开术、开放性胃造口术 Umbilical herniotomy; pyloromyotomy; open gastrostomy | 0.1‒0.3 mL·kg-1 (单侧/per side) |
外侧腰方肌入路阻滞 Lateral quadratus lumborum block | 腹股沟疝修补术、开放性阑尾切除术 Inguinalherniotomy; open appendicectomy | 0.5 mL·kg-1 (单侧最多20 mL/up to 20 mL per side) |
阴茎背神经阻滞 Dorsal penile nerve block | 包皮环切术、远端尿道下裂修复术 Circumcision; distal hypospadias repair | 0.1 mL·kg-1 (双侧最多5 mL/up to 5 mL both sides) |
| [1] | PINTO N, SAWARDEKAR A, SURESH S. Regional anesthesia: options for the pediatric patient[J]. Anesthesiol Clin, 2020, 38(3): 559-575. |
| [2] | HAMILL J K, RAHIRI J L, LILEY A, et al. Rectus sheath and transversus abdominis plane blocks in children: a systematic review and meta-analysis of randomized trials[J]. Paediatr Anaesth, 2016, 26(4): 363-371. |
| [3] | KENDALL M C, ALVES L J C, SUH E I, et al. Regional anesthesia to ameliorate postoperative analgesia outcomes in pediatric surgical patients: an updated systematic review of randomized controlled trials[J]. Local Reg Anesth, 2018, 11: 91-109. |
| [4] | HALL-BURTON D M, HUDSON M E, GRUDZIAK J S, et al. Regional anesthesia is cost-effective in preventing unanticipated hospital admission in pediatric patients having anterior cruciate ligament reconstruction[J]. Reg Anesth Pain Med, 2016, 41(4): 527-531. |
| [5] | ARENA S, DI FABRIZIO D, IMPELLIZZERI P, et al. Enhanced recovery after gastrointestinal surgery (ERAS) in pediatric patients: a systematic review and meta-analysis[J]. J Gastrointest Surg, 2021, 25(11): 2976-2988. |
| [6] | BARNETT N R, HAGEN J G, KATTAIL D. Pediatric regional anesthesia and acute pain management: state of the art[J]. Best Pract Res Clin Anaesthesiol, 2024, 38(2): 135-144. |
| [7] | DUMBARTON T C. Regional anesthesia in complex pediatric patients: advances in opioid-sparing analgesia[J]. Can J Anaesth, 2024, 71(6): 727-730. |
| [8] | MATHEW A, KEROLUS K, BITONTI N, et al. Back to the future: historic insights and recent innovations in pediatric regional anesthesia[J]. J Clin Med, 2024, 13(22): 6704. |
| [9] | GUYATT G H, OXMAN A D, VIST G E, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations[J]. BMJ, 2008, 336(7650): 924-926. |
| [10] | TEO E L, STROUSE P J, CHHEM R K. Musculoskeletal ultrasonography in children[J]. Can Assoc Radiol J, 2002, 53(1): 14-21. |
| [11] | MERELLA F, CANCHI-MURALI N, MOSSETTI V. General principles of regional anaesthesia in children[J]. BJA Educ, 2019, 19(10): 342-348. |
| [12] | HRYHORCZUK A L, RESTREPO R, LEE E Y. Pediatric musculoskeletal ultrasound: practical imaging approach[J]. AJR Am J Roentgenol, 2016, 206(5): W62-W72. |
| [13] | BORETSKY K R. Regional anesthesia in pediatrics: marching forward[J]. Curr Opin Anaesthesiol, 2014, 27(5): 556-560. |
| [14] | MARHOFER P, HARROP-GRIFFITHS W, KETTNER S C, et al. Fifteen years of ultrasound guidance in regional anaesthesia: part 1[J]. Br J Anaesth, 2010, 104(5): 538-546. |
| [15] | BOSENBERG A. Benefits of regional anesthesia in children[J]. Paediatr Anaesth, 2012, 22(1): 10-18. |
| [16] | TSUI B C, SURESH S. Ultrasound imaging for regional anesthesia in infants, children, and adolescents: a review of current literature and its application in the practice of neuraxial blocks[J]. Anesthesiology, 2010,112(3):719-728. |
| [17] | LÖNNQVIST P A. Is ultrasound guidance mandatory when performing paediatric regional anaesthesia?[J]. Curr Opin Anaesthesiol, 2010, 23(3): 337-341. |
| [18] | SURESH S, SCHALDENBRAND K, WALLIS B, et al. Regional anaesthesia to improve pain outcomes in paediatric surgical patients: a qualitative systematic review of randomized controlled trials[J]. Br J Anaesth, 2014, 113(3): 375-390. |
| [19] | SPLINTER W M, THOMSON M E. Somatic paravertebral block decreases opioid requirements in children undergoing appendectomy[J]. Can J Anaesth, 2010, 57(3): 206-210. |
| [20] | GUAY J, SURESH S, KOPP S. The use of ultrasound guidance for perioperative neuraxial and peripheral nerve blocks in children: a cochrane review[J]. Anesth Analg, 2017, 124(3): 948-958. |
| [21] | DADURE C, VEYCKEMANS F, BRINGUIER S, et al. Epidemiology of regional anesthesia in children: lessons learned from the European multi-institutional study APRICOT[J]. Paediatr Anaesth, 2019, 29(11): 1128-1135. |
| [22] | BOSENBERG A T. Regional anaesthesia in children: an update[J]. South Afr J Anaesth Analg, 2013, 19(6): 282-288. |
| [23] | DOHLMAN L E, KWIKIRIZA A, EHIE O. Benefits and barriers to increasing regional anesthesia in resource-limited settings[J]. Local Reg Anesth, 2020, 13: 147-158. |
| [24] | BRINDLE M E, MCDIARMID C, SHORT K, et al. Consensus guidelines for perioperative care in neonatal intestinal surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations[J]. World J Surg, 2020, 44(8): 2482-2492. |
| [25] | Association of Paediatric Anaesthetists of Great Britain and Ireland. Good practice in postoperative and procedural pain management, 2nd edition[J]. Paediatr Anaesth, 2012, 22(Suppl 1): 1-79. |
| [26] | LÖNNQVIST P A. Regional anaesthesia and analgesia in the neonate[J]. Best Pract Res Clin Anaesthesiol, 2010, 24(3): 309-321. |
| [27] | RICHMAN M, BERMAN J M, ROSS E M. Regional anesthesia use in pediatric burn surgery: a descriptive retrospective series[J]. Cureus, 2021, 13(10): e19063. |
| [28] | MONINGI S, PATKI A, PADHY N, et al. Enhanced recovery after surgery: an anesthesiologist's perspective[J]. J Anaesthesiol Clin Pharmacol, 2019, 35(Suppl 1): S5-S13. |
| [29] | BUGADA D, GHISI D, MARIANO E R. Continuous regional anesthesia: a review of perioperative outcome benefits[J]. Minerva Anestesiol, 2017, 83(10): 1089-1100. |
| [30] | LI T, DONG T T, CUI Y S, et al. Effect of regional anesthesia on the postoperative delirium: a systematic review and meta-analysis of randomized controlled trials[J]. Front Surg, 2022, 9: 937293. |
| [31] | SOMAINI M, SAHILLIOĞLU E, MARZORATI C, et al. Emergence delirium, pain or both? A challenge for clinicians[J]. Paediatr Anaesth, 2015, 25(5): 524-529. |
| [32] | KIM H S, KIM C S, KIM S D, et al. Fascia iliaca compartment block reduces emergence agitation by providing effective analgesic properties in children[J]. J Clin Anesth, 2011, 23(2): 119-123. |
| [33] | MESNIL M, DADURE C, CAPTIER G, et al. A new approach for peri-operative analgesia of cleft palate repair in infants: the bilateral suprazygomatic maxillary nerve block[J]. Paediatr Anaesth, 2010, 20(4): 343-349. |
| [34] | MERELLA F, MOSSETTI V. Ultrasound-guided upper and lower extremity nerve blocks in children[J]. BJA Educ, 2020, 20(2): 42-50. |
| [35] | CUCCHIARO G, CRAIG K, MARKS K, et al. Short- and long-term results of an inpatient programme to manage complex regional pain syndrome in children and adolescents[J]. Br J Pain, 2017, 11(2): 87-96. |
| [36] | WHITE W, BELLMAN L, LIU Y T. Ultrasound-guided pediatric nerve blocks in the emergency department: an evidence-based update[J]. Pediatr Emerg Med Pract, 2022, 19(5): 1-32. |
| [37] | 万里, 王云, 王庚, 等. 超声引导区域阻滞/镇痛的专家共识[M]//黄宇光, 邓小明. 2020版中国麻醉学指南与专家共识. 北京: 人民卫生出版社, 2022: 336-346. |
| WAN L, WANG Y, WANG G, et al. Expert consensus on ultrasound-guided regional block/analgesia[M]//HUANG Y G, DENG X M. Chinese anesthesiology guidelines and expert consensus (2020). Beijing: People's Medical Publishing House, 2022: 336-346. | |
| [38] | LÖNNQVIST P A, ECOFFEY C, BOSENBERG A, et al. The European Society of Regional Anesthesia and Pain Therapy and the American Society of Regional Anesthesia and Pain Medicine Joint Committee practice advisory on controversial topics in pediatric regional anesthesia Ⅰ and Ⅱ: what do they tell us?[J]. Curr Opin Anaesthesiol, 2017, 30(5): 613-620. |
| [39] | IVANI G, SURESH S, ECOFFEY C, et al. The European Society of Regional Anaesthesia and Pain Therapy and the American Society of Regional Anesthesia and Pain Medicine Joint Committee practice advisory on controversial topics in pediatric regional anesthesia[J]. Reg Anesth Pain Med, 2015, 40(5): 526-532. |
| [40] | PONDE V C, RATH A, SINGH N. Expert's tips on regional blocks in neonates and infants[J]. Anesth Pain Med (Seoul), 2024, 19(Suppl 1): S73-S86. |
| [41] | PEARSON A E, ROBERTS S, TURBITT L R. New blocks on the kids: core basic nerve blocks in paediatric anaesthesia[J]. Anaesthesia, 2023, 78(1): 3-8. |
| [42] | YENTIS S M, HARTLE A J, BARKER I R, et al. AAGBI: consent for anaesthesia 2017[J]. Anaesthesia, 2017, 72(1): 93-105. |
| [43] | DISMA N, VEYCKEMANS F, VIRAG K, et al. Morbidity and mortality after anaesthesia in early life: results of the European prospective multicentre observational study, neonate and children audit of anaesthesia practice in Europe (NECTARINE)[J]. Br J Anaesth, 2021, 126(6): 1157-1172. |
| [44] | 中华医学会麻醉学分会区域麻醉镇静管理专家共识工作小组. 区域麻醉镇静管理专家共识[J]. 中华麻醉学杂志, 2017(1): 12-20. |
| Chinese Society of Anesthesiology Task Force on Sedation during Regional Anesthesia. Consensus on sedation during regional anesthesia[J]. Chinese Journal of Anesthesiology, 2017, 37(1): 12-20. | |
| [45] | PONDE V, PURI K, OSAZUWA M, et al. Principles of regional anaesthesia in children[EB/OL]. (2022-11-22)[2025-07-25]. https://resources.wfsahq.org/wp-content/uploads/atow-485.pdf. |
| [46] | HEWSON D W, BEDFORTH N M, HARDMAN J G. Peripheral nerve injury arising in anaesthesia practice[J]. Anaesthesia, 2018, 73(Suppl 1): 51-60. |
| [47] | WALKER B J, LONG J B, SATHYAMOORTHY M, et al. Complications in pediatric regional anesthesia: an analysis of more than 100,000 blocks from the Pediatric Regional Anesthesia Network[J]. Anesthesiology, 2018, 129(4): 721-732. |
| [48] | GADSDEN J C. The role of peripheral nerve stimulation in the era of ultrasound-guided regional anaesthesia[J]. Anaesthesia, 2021, 76(Suppl 1): 65-73. |
| [49] | Disinfection of ultrasound transducers used for percutaneous procedures[J]. J Ultrasound Med, 2021, 40(5): 895-897. |
| [50] | BOMBERG H, BAYER I, WAGENPFEIL S, et al. Prolonged catheter use and infection in regional anesthesia: a retrospective registry analysis[J]. Anesthesiology, 2018, 128(4): 764-773. |
| [51] | AZI L M T A, FONSECA N M, LINARD L G. SBA 2020: regional anesthesia safety recommendations update[J]. Braz J Anesthesiol, 2020, 70(4): 398-418. |
| [52] | YOSHIDA K, KAKINOUCHI K. Does a single ultrasound-guided peripheral nerve block always require a full aseptic technique?[J]. Reg Anesth Pain Med, 2024, 49(10): 775. |
| [53] | MARHOFER P. Upper extremity peripheral blocks[J]. Tech Reg Anesth Pain Manag, 2007, 11(4): 215-221. |
| [54] | TAENZER A, WALKER B J, BOSENBERG A T, et al. Interscalene brachial plexus blocks under general anesthesia in children: is this safe practice?[J]. Reg Anesth Pain Med, 2014, 39(6): 502-505. |
| [55] | GUZEL M, BINGUL E S, SALVIZ E A, et al. Comparison of ultrasound-guided supraclavicular and costoclavicular brachial plexus blocks in pediatric patients: a randomized clinical trial[J]. J Anesth, 2023, 37(2): 186-194. |
| [56] | CARIOCA F, SILVA M, BISPO C, et al. Costoclavicular brachial plexus block in paediatric anaesthesia: a retrospective pilot study[J]. J Clin Anesth, 2021, 69: 110113. |
| [57] | KARMAKAR M K, SALA-BLANCH X, SONGTHAMWAT B, et al. Benefits of the costoclavicular space for ultrasound-guided infraclavicular brachial plexus block: description of a costoclavicular approach[J]. Reg Anesth Pain Med, 2015, 40(3): 287-288. |
| [58] | 李品菲, 郭璇, 洪四名. 超声引导下改良肋锁间隙臂丛神经阻滞用于前臂手术的效果[J]. 中华麻醉学杂志, 2022, 42(2): 203-206. |
| LI P F, GUO X, HONG S M. Efficacy of ultrasound-guided modified brachial plexus block at costoclavicular space for forearm surgery[J]. Chinese Journal of Anesthesiology, 2022, 42(2): 203-206. | |
| [59] | 王伟涛, 涂友兵, 易祖港, 等. 超声引导下患儿肋锁间隙臂丛神经阻滞的研究进展[J]. 临床麻醉学杂志, 2024, 40(4): 424-428. |
| WANG W T, TU Y B, YI Z G, et al. Research progress on ultrasound-guided costoclavicular space brachial plexus block in pediatric patients[J]. Journal of Clinical Anesthesiology, 2024, 40(4): 424-428. | |
| [60] | OBERNDORFER U, MARHOFER P, BÖSENBERG A, et al. Ultrasonographic guidance for sciatic and femoral nerve blocks in children[J]. Br J Anaesth, 2007, 98(6): 797-801. |
| [61] | TURNER A L, STEVENSON M D, CROSS K P. Impact of ultrasound-guided femoral nerve blocks in the pediatric emergency department[J]. Pediatr Emerg Care, 2014, 30(4): 227-229. |
| [62] | KIRCHMAIR L, ENNA B, MITTERSCHIFFTHALER G, et al. Lumbar plexus in children. A sonographic study and its relevance to pediatric regional anesthesia[J]. Anesthesiology, 2004, 101(2): 445-450. |
| [63] | HORLOCKER T T, VANDERMEUELEN E, KOPP S L, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (fourth edition)[J]. Reg Anesth Pain Med, 2018, 43(3): 263-309. |
| [64] | HSU D T. Delayed retroperitoneal haematoma after failed lumbar plexus block[J]. Br J Anaesth, 2005, 94(3): 395-396. |
| [65] | KEPLINGER M, MARHOFER P, MORIGGL B, et al. Cutaneous innervation of the hand: clinical testing in volunteers shows high intra- and inter-individual variability[J]. Br J Anaesth, 2018, 120(4): 836-845. |
| [66] | LÖNNQVIST P A. Fascial plane blocks in children: scientifically supported or not?[J]. Paediatr Anaesth, 2024, 34(1): 13-18. |
| [67] | WINNIE L, KAO Y H, LIAO C C, et al. Comparative analgesic efficacies of ropivacaine and bupivacaine for postoperative rectus sheath block in paediatric abdominal surgery: a meta-analysis of randomized controlled trial and retrospective cohort studies[J]. Pain Res Manag, 2021, 2021: 5535730. |
| [68] | CLAXTON H L, NEVINS E J, MCCALLUM I. Comparison of the effectiveness of thoracic epidural and rectus sheath catheter as analgesic modalities following laparotomy: a systematic review and meta-analysis[J]. J Perioper Pract, 2023, 33(11): 332-341. |
| [69] | GURNANEY H G, MAXWELL L G, KRAEMER F W, et al. Prospective randomized observer-blinded study comparing the analgesic efficacy of ultrasound-guided rectus sheath block and local anaesthetic infiltration for umbilical hernia repair[J]. Br J Anaesth, 2011, 107(5): 790-795. |
| [70] | UESHIMA H, OTAKE H, LIN J A. Ultrasound-guided quadratus lumborum block: an updated review of anatomy and techniques[J]. Biomed Res Int, 2017, 2017: 2752876. |
| [71] | HUSSEIN M M. Ultrasound-guided quadratus lumborum block in pediatrics: trans-muscular versus intra-muscular approach[J]. J Anesth, 2018, 32(6): 850-855. |
| [72] | ABU ELYAZED M M, MOSTAFA S F, ABDULLAH M A, et al. The effect of ultrasound-guided transversus abdominis plane (TAP) block on postoperative analgesia and neuroendocrine stress response in pediatric patients undergoing elective open inguinal hernia repair[J]. Paediatr Anaesth, 2016, 26(12): 1165-1171. |
| [73] | BRYSKIN R B, LONDERGAN B, WHEATLEY R, et al. Transversus abdominis plane block versus caudal epidural for lower abdominal surgery in children: a double-blinded randomized controlled trial[J]. Anesth Analg, 2015, 121(2): 471-478. |
| [74] | SURESH S, TAYLOR L J, DE OLIVEIRA G S Jr. Dose effect of local anesthetics on analgesic outcomes for the transversus abdominis plane (TAP) block in children: a randomized, double-blinded, clinical trial[J]. Paediatr Anaesth, 2015, 25(5): 506-510. |
| [75] | TEUNKENS A, VAN DE VELDE M, VERMEULEN K, et al. Dorsal penile nerve block for circumcision in pediatric patients: a prospective, observer-blinded, randomized controlled clinical trial for the comparison of ultrasound-guided vs landmark technique[J]. Paediatr Anaesth, 2018, 28(8): 703-709. |
| [76] | FUJIWARA T, KAGAWA T. Ultrasound-guided dorsal penile nerve block in children: in-plane technique[J]. Paediatr Anaesth, 2023, 33(6): 499. |
| [77] | ANTONY S, GURNANEY H, GANESH A. Pediatric ambulatory continuous peripheral nerve blocks[J]. Anesthesiol Clin, 2018, 36(3): 455-465. |
| [78] | ROCHETTE A, DADURE C, RAUX O, et al. A review of pediatric regional anesthesia practice during a 17-year period in a single institution[J]. Paediatr Anaesth, 2007, 17(9): 874-880. |
| [79] | RATHMELL J P, KEHLET H. Do we have the tools to prevent phantom limb pain?[J]. Anesthesiology, 2011, 114(5): 1021-1024. |
| [80] | MORGAN J, CHECKETTS M, ARANA A, et al. Prevention of perioperative venous thromboembolism in pediatric patients: guidelines from the Association of Paediatric Anaesthetists of Great Britain and Ireland (APAGBI)[J]. Paediatr Anaesth, 2018, 28(5): 382-391. |
| [81] | SURESH S, ECOFFEY C, BOSENBERG A, et al. The European Society of Regional Anaesthesia and Pain Therapy/American Society of Regional Anesthesia and Pain Medicine recommendations on local anesthetics and adjuvants dosage in pediatric regional anesthesia[J]. Reg Anesth Pain Med, 2018, 43(2): 211-216. |
| [82] | SURESH S, DE OLIVEIRA G S Jr. Local anaesthetic dosage of peripheral nerve blocks in children: analysis of 40 121 blocks from the Pediatric Regional Anesthesia Network database[J]. Br J Anaesth, 2018, 120(2): 317-322. |
| [83] | TAENZER A H, HERRICK M, HOYT M, et al. Variation in pediatric local anesthetic dosing for peripheral nerve blocks: an analysis from the Pediatric Regional Anesthesia Network (PRAN)[J]. Reg Anesth Pain Med, 2020, 45(12): 964-969. |
| [84] | PONDE V. Recent trends in paediatric regional anaesthesia[J]. Indian J Anaesth, 2019, 63(9): 746-753. |
| [85] | DESAI N, ALBRECHT E. Local anaesthetic adjuncts for peripheral nerve blockade[J]. Curr Opin Anaesthesiol, 2023, 36(5): 533-540. |
| [86] | LUNDBLAD M, TRIFA M, KAABACHI O, et al. Alpha-2 adrenoceptor agonists as adjuncts to peripheral nerve blocks in children: a meta-analysis[J]. Paediatr Anaesth, 2016, 26(3): 232-238. |
| [87] | TAFOYA S P, TUMBER S S. The use of multimodal perineural adjuvants in pediatric peripheral nerve blocks: technique and experiences[J]. Cureus, 2022, 14(3): e23186. |
| [88] | MIKJUNOVIKJ-DEREBANOVA L, KARTALOV A, KUZMANOVSKA B, et al. Epinephrine and dexamethasone as adjuvants in upper extremity peripheral nerve blocks in pediatric patients[J]. Pril (Makedon Akad Nauk Umet Odd Med Nauki), 2021, 42(3): 79-88. |
| [89] | TURCO A, CERULO M, DEL CONTE F, et al. Correlation between FLACC scale score and analgesic requirement in children undergoing minimally invasive surgery[J]. Pediatr Med Chir, 2023, 45(1). DOI: 10.4081/pmc.2023.288. |
| [90] | CHOI S, YOON S H, LEE H J. Beyond measurement: a deep dive into the commonly used pain scales for postoperative pain assessment[J]. Korean J Pain, 2024, 37(3): 188-200. |
| [91] | ECOFFEY C, LACROIX F, GIAUFRÉ E, et al. Epidemiology and morbidity of regional anesthesia in children: a follow-up one-year prospective survey of the French-Language Society of Paediatric Anaesthesiologists (ADARPEF)[J]. Paediatr Anaesth, 2010, 20(12): 1061-1069. |
| [92] | LÖNNQVIST P A. Toxicity of local anesthetic drugs: a pediatric perspective[J]. Paediatr Anaesth, 2012, 22(1): 39-43. |
| [93] | SINGARAVELU RAMESH A, BORETSKY K. Local anesthetic systemic toxicity in children: a review of recent case reports and current literature[J]. Reg Anesth Pain Med, 2021, 46(10): 909-914. |
| [94] | ECOFFEY C, BOSENBERG A, LONNQVIST P A, et al. Practice advisory on the prevention and management of complications of pediatric regional anesthesia[J]. J Clin Anesth, 2022, 79: 110725. |
| [95] | WALKER B J, LONG J B, DE OLIVEIRA G S, et al. Peripheral nerve catheters in children: an analysis of safety and practice patterns from the pediatric regional anesthesia network (PRAN)[J]. Br J Anaesth, 2015, 115(3): 457-462. |
| [96] | POLANER D M, TAENZER A H, WALKER B J, et al. Pediatric Regional Anesthesia Network (PRAN): a multi-institutional study of the use and incidence of complications of pediatric regional anesthesia[J]. Anesth Analg, 2012, 115(6): 1353-1364. |
| [97] | Society for Pediatric Anesthesia. Pedi crisis checklist 2020[EB/OL]. [2025-07-25]. https://pedsanesthesia.org/checklists/. |
| [98] | PANESAR S S, JAVAD S, DE SILVA D, et al. The epidemiology of anaphylaxis in Europe: a systematic review[J]. Allergy, 2013, 68(11): 1353-1361. |
| [99] | VOLCHECK G W, MERTES P M. Local and general anesthetics immediate hypersensitivity reactions[J]. Immunol Allergy Clin North Am, 2014, 34(3): 525-546, viii. |
| [100] | DODD A, TURNER P J, SOAR J, et al. Emergency treatment of peri-operative anaphylaxis: Resuscitation Council UK algorithm for anaesthetists[J]. Anaesthesia, 2024, 79(5): 535-541. |
| [101] | GARVEY L H, DEWACHTER P, HEPNER D L, et al. Management of suspected immediate perioperative allergic reactions: an international overview and consensus recommendations[J]. Br J Anaesth, 2019, 123(1): e50-e64. |
| [102] | JENG C L, ROSENBLATT M A. Intraneural injections and regional anesthesia: the known and the unknown[J]. Minerva Anestesiol, 2011, 77(1): 54-58. |
| [103] | SONDEKOPPAM R V, TSUI B C H. Factors associated with risk of neurologic complications after peripheral nerve blocks: a systematic review[J]. Anesth Analg, 2017, 124(2): 645-660. |
| [104] | 万里, 王云, 王庚, 等. 外周神经阻滞并发症防治专家共识[M]// 黄宇光, 邓小明. 2020版中国麻醉学指南与专家共识. 北京: 人民卫生出版社, 2022: 244-253. |
| WAN L, WANG Y, WANG G, et al. Expert consensus on prevention and treatment of peripheral nerve block complications[M]// HUANG Y G, DENG X M. Chinese anesthesiology guidelines and expert consensus (2020). Beijing: People's Medical Publishing House, 2022: 244-253. | |
| [105] | KROL A, VALA A, PHYLACTIDES L, et al. Injection pressure mapping of intraneural vs. perineural injections: further lessons from cadaveric studies[J]. Minerva Anestesiol, 2018, 84(8): 907-918. |
| [106] | QUADRI C, SAPORITO A, CAPDEVILA X. Real-time continuous monitoring of injection pressure at the needle tip for peripheral nerve blocks: description of a new method[J]. Anaesthesia, 2018, 73(2): 187-194. |
| [107] | KRISHNA PRASAD G V, KHANNA S, JAISHREE S V. Review of adjuvants to local anesthetics in peripheral nerve blocks: current and future trends[J]. Saudi J Anaesth, 2020, 14(1): 77-84. |
| [108] | PULOS N, SHIN E H, SPINNER R J, et al. Management of iatrogenic nerve injuries[J]. J Am Acad Orthop Surg, 2019, 27(18): e838-e848. |
| [109] | 万里, 王云, 王庚, 等. 局部麻醉药全身毒性防治专家共识[M]// 黄宇光, 邓小明. 2020版中国麻醉学指南与专家共识. 北京: 人民卫生出版社, 2022: 235-243. |
| WAN L, WANG Y, WANG G, et al. Expert consensus on prevention and treatment of local anesthetic systemic toxicity[M]// HUANG Y G, DENG X M. Chinese anesthesiology guidelines and expert consensus (2020). Beijing: People's Medical Publishing House, 2022: 235-243. | |
| [110] | KIETAIBL S, FERRANDIS R, GODIER A, et al. Regional anaesthesia in patients on antithrombotic drugs: joint ESAIC/ESRA guidelines[J]. Eur J Anaesthesiol, 2022, 39(2): 100-132. |
| [111] | SIMIĆ D, STEVIĆ M, STANKOVIĆ Z, et al. The safety and efficacy of the continuous peripheral nerve block in postoperative analgesia of pediatric patients[J]. Front Med (Lausanne), 2018, 5: 57. |
| [112] | VIJ N, SINGHAL N R, TRIF D, et al. Continuous epidural analgesia versus continuous peripheral nerve block in unilateral lower extremity pediatric orthopedic surgery: a matched case comparison study[J]. Cureus, 2023, 15(6): e40412. |
| [1] | 王治琪, 王莹. 儿童炎症性肠病相关贫血的诊治研究进展[J]. 上海交通大学学报(医学版), 2025, 45(9): 1232-1238. |
| [2] | 蒋婕, 张泓, 伦赫远, 潘芬, 于方圆, 何平. 儿童肺炎克雷伯菌感染分子流行病学特征[J]. 上海交通大学学报(医学版), 2025, 45(8): 1027-1034. |
| [3] | 梁书源, 叶宝英, 程蔚蔚. 超声指标和血液指标预测胎儿生长受限的研究现状[J]. 上海交通大学学报(医学版), 2025, 45(8): 1059-1065. |
| [4] | 何晨, 颜斯蕾, 周维涛, 凌勇, 于宁宁, 蒋鲲, 钱莉玲. 囊性纤维化合并变应性支气管肺曲菌病的临床分析及文献整合研究[J]. 上海交通大学学报(医学版), 2025, 45(8): 1066-1073. |
| [5] | 陆晔峰, 高磊青, 倪晓筱, 富晶晶. 儿童肝移植术后早期血糖及血脂的多时间点监测与影响因素分析[J]. 上海交通大学学报(医学版), 2025, 45(4): 443-451. |
| [6] | 刘田恬, 赵奕琳, 宁菁菁, 张育才, 王春霞. 儿童脓毒症预后相关长链非编码RNA筛选及竞争性内源RNA网络的构建[J]. 上海交通大学学报(医学版), 2025, 45(3): 282-291. |
| [7] | 刘楚萱, 左佳鑫, 熊屏. 基于超声评分参数及临床指标的列线图鉴别原发性干燥综合征与IgG4相关唾液腺炎[J]. 上海交通大学学报(医学版), 2025, 45(3): 373-380. |
| [8] | 沈浩亮, 袁恺豪, 余磊, 阳娜娜, 王逸平, 赵宏胜, 郭凤梅, 孙晨靓. 膈肌联合肋间肌超声对脓毒症机械通气患者脱机评估的价值[J]. 上海交通大学学报(医学版), 2025, 45(2): 186-193. |
| [9] | 马瑞琳, 刘雨, 徐桂香, 史昊然, 崔俭俭, 杨泽俊, 毛艳, 赵茵. 子痫前期大鼠模型子宫动脉、脐动脉、大脑中动脉超声多普勒参数与胎盘血管病理及妊娠结局的关系[J]. 上海交通大学学报(医学版), 2024, 44(5): 543-551. |
| [10] | 刘美伶, 周亚兵, 王晓强. 儿童神经纤维瘤病1型颅内肿瘤性病变的治疗进展[J]. 上海交通大学学报(医学版), 2024, 44(3): 399-406. |
| [11] | 姜允丽, 李爱求, 肖艳赏, 李田田, 胡亚晨, 张潇潇, 吴蓓蓉. 基于EMS管理模式的延续性护理在学龄前喘息性疾病儿童中的应用观察[J]. 上海交通大学学报(医学版), 2024, 44(2): 228-236. |
| [12] | 胡灿芳, 钟传钰, 曹立. 神经调控技术在帕金森病治疗中的应用研究进展[J]. 上海交通大学学报(医学版), 2024, 44(2): 258-263. |
| [13] | 黄勤, 黄缨, 李文. 输卵管复合妊娠的超声检查时间探讨[J]. 上海交通大学学报(医学版), 2024, 44(12): 1545-1551. |
| [14] | 吴凌恒, 陈建雄, 张梦娇, 沙蕾, 曹萌萌, 沈崔琴, 杜联芳, 李朝军. 血糖控制不理想对2型糖尿病患者亚临床心肌收缩功能的影响研究[J]. 上海交通大学学报(医学版), 2023, 43(8): 1024-1031. |
| [15] | 贺玉洁, 樊琳蕊, 张翘楚, 张至立, 丁珺, 施超, 姚勇强, 任宏政. 现场快速评估法辅助超声引导下甲状腺细针穿刺的研究[J]. 上海交通大学学报(医学版), 2023, 43(8): 1032-1037. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||