
上海交通大学学报(医学版) ›› 2025, Vol. 45 ›› Issue (8): 1017-1026.doi: 10.3969/j.issn.1674-8115.2025.08.009
收稿日期:2025-02-26
接受日期:2025-05-22
出版日期:2025-08-28
发布日期:2025-08-14
通讯作者:
沈国芳,主任医师,博士;电子信箱:shengf1428@sjtu.edu.cn作者简介:第一联系人:为共同第一作者(co-first authors)。
基金资助:
YU Zuyin, LIU Yiyun, XIE Jiahui, CAI Ming( ), SHEN Guofang(
), SHEN Guofang( )
)
Received:2025-02-26
Accepted:2025-05-22
Online:2025-08-28
Published:2025-08-14
Contact:
SHEN Guofang, Email: shengf1428@sjtu.edu.cnSupported by:摘要:
目的·探索黏性骨[脱蛋白猪骨矿物颗粒联合高级富血小板纤维蛋白(advanced platelet-rich fibrin,A-PRF)与液态富血小板纤维蛋白(liquid platelet-rich fibrin,L-PRF)]在单侧牙槽突裂修复中的临床效果和安全性。方法·招募2023年12月1日—2024年8月31日确诊为单侧牙槽突裂且符合纳入标准的患者。将患者随机分为2组,分别采用黏性骨或自体髂骨松质骨移植进行牙槽突裂植骨术,黏性骨组设为试验组,髂骨组设为对照组。主要疗效指标为术后6个月的骨吸收率,通过收集患者术前、术后即刻及术后半年的计算机断层扫描数据,利用Simplant Pro 17.01软件测量术后即刻与术后半年的移植骨量以计算该指标。次要疗效指标包括术后6个月的骨密度、患者术后并发症发生情况以及口腔健康质量量表得分。运用Prism 10软件进行数据分析,采用t检验及Pearson相关性分析方法。结果·试验组纳入17名单侧牙槽突裂患者,对照组纳入15名患者。试验组术后6个月剩余骨量多于对照组,试验组骨吸收率为33.24%±17.16%,显著低于对照组的66.31%±17.98%(P<0.001)。试验组有1名患者在术后2周出现前庭侧黏膜裂开,并伴有骨粉排出;对照组有3名患者在术后1个月出现前庭侧黏膜裂开伴松质骨排出,其中1名患者在术后4个月出现移植骨坏死。试验组术后 6个月骨密度显著高于对照组(P<0.001),且口腔健康质量量表得分更低。结论·相较于髂骨松质骨,黏性骨用于单侧牙槽突裂患者的治疗时,展现出更低的骨吸收率与更高的骨密度,表明其成骨能力更佳。较少的并发症例数与更低的口腔健康量表得分,提示其安全性更高,因而具有较好的临床推广应用价值。
中图分类号:
虞祖音, 刘逸云, 解嘉慧, 蔡鸣, 沈国芳. 黏性骨与自体髂骨松质骨移植修复单侧牙槽突裂成骨效果的临床研究[J]. 上海交通大学学报(医学版), 2025, 45(8): 1017-1026.
YU Zuyin, LIU Yiyun, XIE Jiahui, CAI Ming, SHEN Guofang. Clinical study on osteogenic effect of sticky bone and autologous iliac cancellous bone graft in repairing unilateral alveolar cleft[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2025, 45(8): 1017-1026.
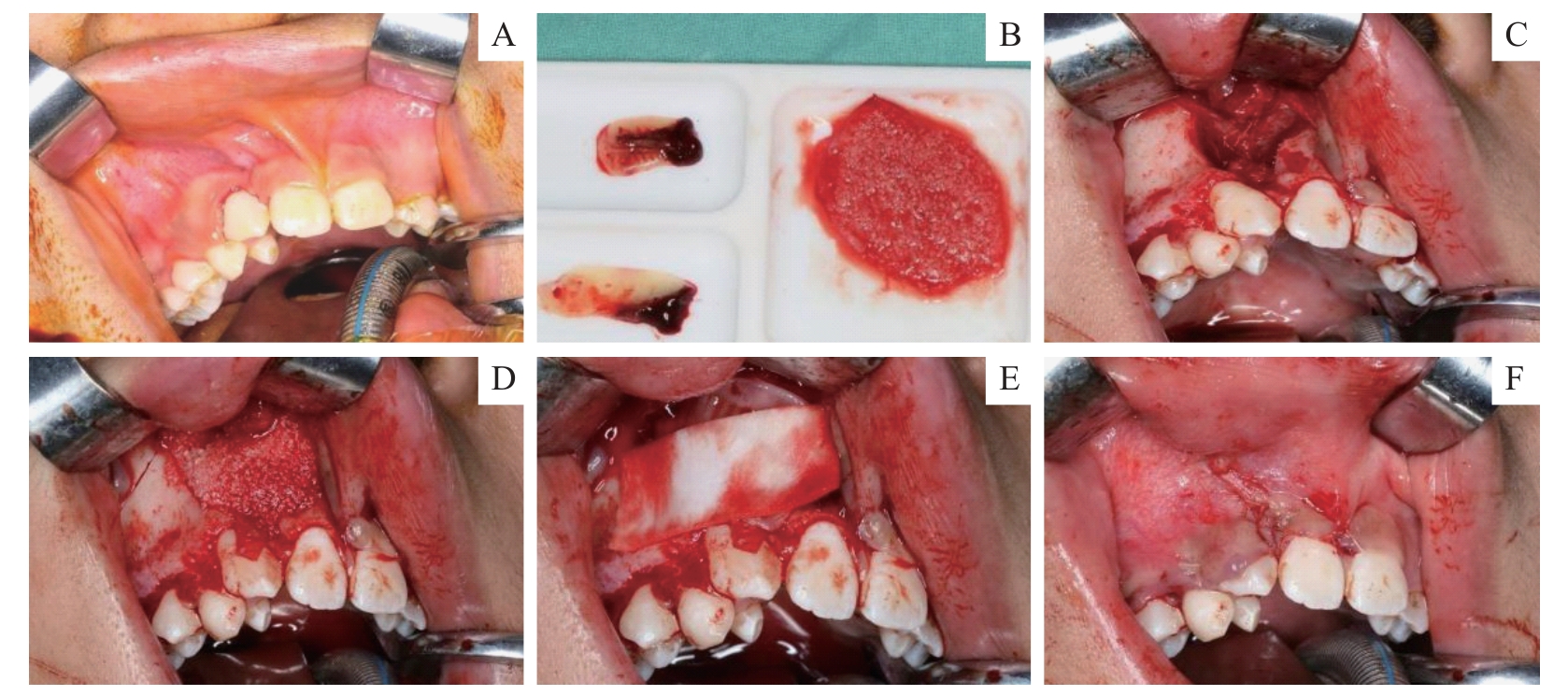
图1 黏性骨修复牙槽突裂手术Note: A. Alveolar cleft before surgery. B. Preparation of sticky bone and A-PRF membrane. C. Preparation of the bone grafting area. D. The prepared sticky bone and A - PRF membrane were implanted into the cleft. E. Another Bio-Gide film was placed on the labial side. F. The bone grafting area was tightly closed with absorbable thread.
Fig 1 Surgery for repairing alveolar cleft with sticky bone
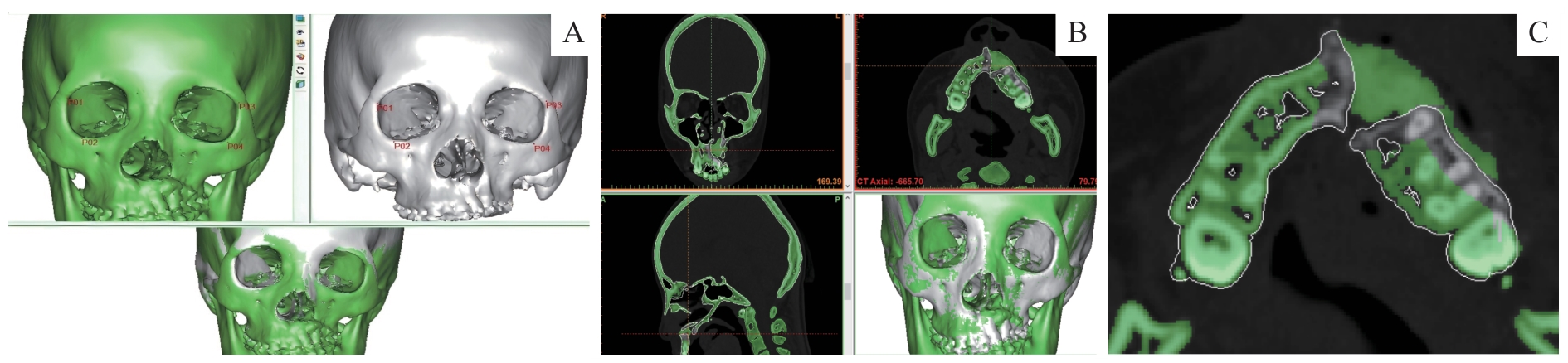
图2 术后移植骨量测定方法Note: A. Matching of 3D reconstruction: the cranio-maxillary complex, reconstructed in 3D before and after surgery, was aligned based on bone surface landmarks. B. 3D reconstruction registration: adjustment and alignment were carried out in the coronal, sagittal, and horizontal planes to ensure overlap of preoperative and postoperative alveolar bones at corresponding anatomical locations. C. Grafted bone extraction: after the alignment was completed, the preoperative alveolar bone contour was used as reference to separate the grafted bone from the surrounding bone in each plane, ultimately identifying the region of interest.
Fig 2 Method for measuring post operative grafted bone volume
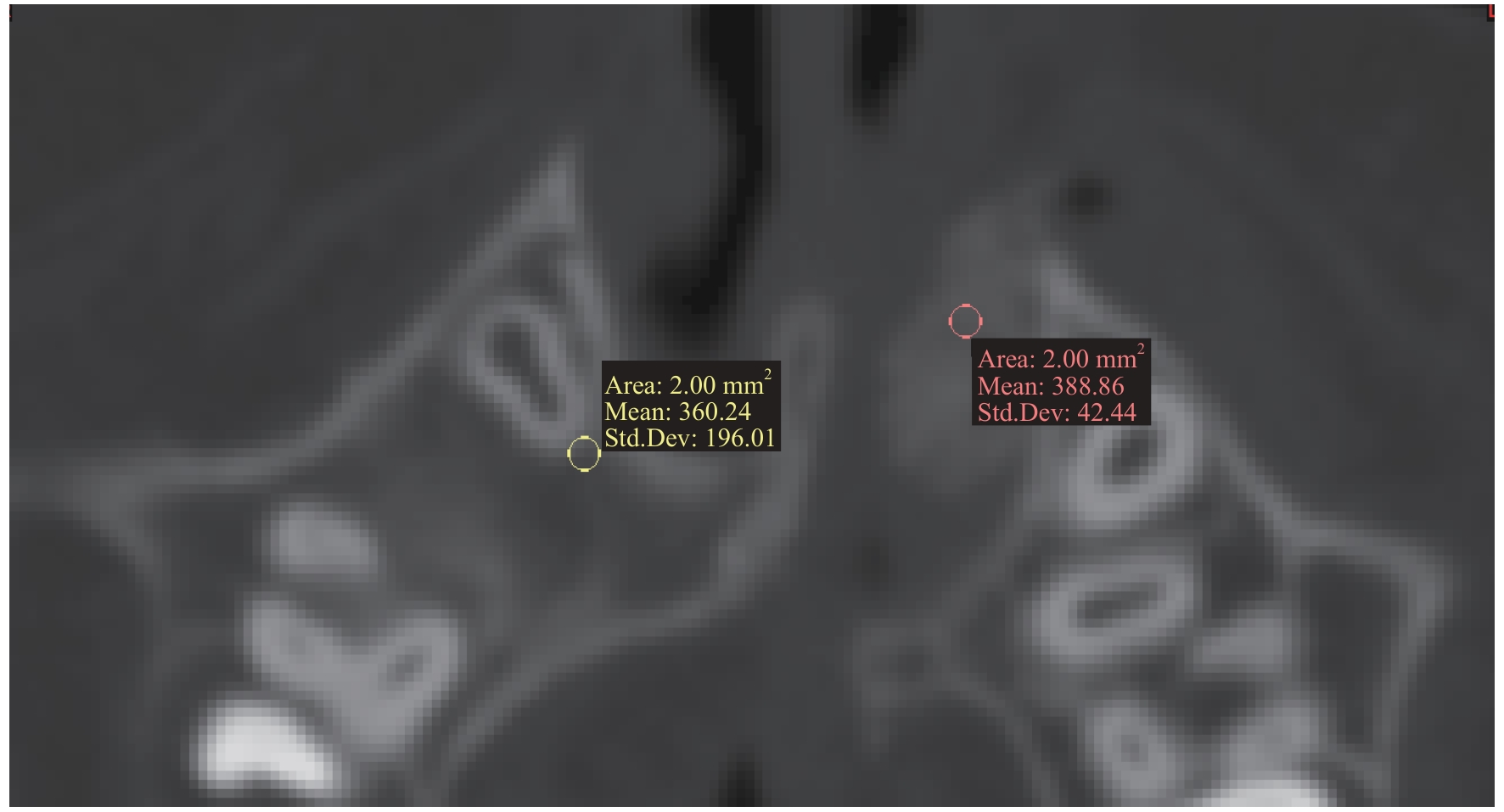
图3 牙槽骨骨密度的测量Note: A 2-mm² circular ROI was drawn. Using the root tips of adjacent teeth in the mesial-distal direction of the fracture area and the canines on the normal side as references, gray values were measured from 3 mm below the enamel-bone junction down to the root tip.
Fig 3 measurement of alveolar bone density
| Indicator | Test group | Control group | P value |
|---|---|---|---|
| Gender (male)/n(%) | 11 (64.7) | 8 (53.3) | 0.513 |
| Age/year | 15.47±6.00 | 13.93±4.85 | 0.518 |
| Side (left)/n(%) | 9 (52.9) | 9 (60.0) | 0.688 |
| Hospital day/d | 3.20±2.34 | 5.30±1.16 | 0.033 |
| Patients receiving orthodontic treatment/n(%) | 5 (29.41) | 4 (26.67) | 0.999 |
| Width of piriform aperture on cleft side/mm | 14.87±2.54 | 14.01±3.48 | 0.480 |
| Width of alveolar crest of cleft side/mm | 5.23±1.87 | 5.76±1.65 | 0.574 |
表1 2组患者的一般资料情况
Tab 1 General information of patients in the two groups
| Indicator | Test group | Control group | P value |
|---|---|---|---|
| Gender (male)/n(%) | 11 (64.7) | 8 (53.3) | 0.513 |
| Age/year | 15.47±6.00 | 13.93±4.85 | 0.518 |
| Side (left)/n(%) | 9 (52.9) | 9 (60.0) | 0.688 |
| Hospital day/d | 3.20±2.34 | 5.30±1.16 | 0.033 |
| Patients receiving orthodontic treatment/n(%) | 5 (29.41) | 4 (26.67) | 0.999 |
| Width of piriform aperture on cleft side/mm | 14.87±2.54 | 14.01±3.48 | 0.480 |
| Width of alveolar crest of cleft side/mm | 5.23±1.87 | 5.76±1.65 | 0.574 |
| Influence factor | Test group | Control group | |||
|---|---|---|---|---|---|
| r | P | r | P | ||
| Width of apertura piriformis | 0.427 | 0.146 | 0.516 | 0.086 | |
| Width of alveolar crest | 0.493 | 0.087 | 0.825 | 0.001 | |
| Gender | 0.327 | 0.254 | 0.564 | 0.089 | |
| Age | 0.040 | 0.890 | 0.519 | 0.084 | |
| Cleft side | 0.354 | 0.195 | 0.003 | 0.992 | |
| Orthodontic treatment | -0.200 | 0.474 | 0.287 | 0.367 | |
表2 术后即刻的移植骨量相关性分析
Tab 2 Correlation analysis of the grafted bone volume immediately after surgery
| Influence factor | Test group | Control group | |||
|---|---|---|---|---|---|
| r | P | r | P | ||
| Width of apertura piriformis | 0.427 | 0.146 | 0.516 | 0.086 | |
| Width of alveolar crest | 0.493 | 0.087 | 0.825 | 0.001 | |
| Gender | 0.327 | 0.254 | 0.564 | 0.089 | |
| Age | 0.040 | 0.890 | 0.519 | 0.084 | |
| Cleft side | 0.354 | 0.195 | 0.003 | 0.992 | |
| Orthodontic treatment | -0.200 | 0.474 | 0.287 | 0.367 | |
| Influence factor | Test group | Control group | |||
|---|---|---|---|---|---|
| r | P | r | P | ||
| Width of apertura piriformis | 0.184 | 0.547 | 0.184 | 0.547 | |
| Width of alveolar crest | 0.256 | 0.398 | 0.256 | 0.547 | |
| Gender | 0.514 | 0.050 | 0.009 | 0.977 | |
| Age | 0.080 | 0.778 | -0.048 | 0.883 | |
| Cleft side | 0.259 | 0.352 | -0.369 | 0.238 | |
| Orthodontic treatment | -0.145 | 0.621 | 0.390 | 0.203 | |
表3 术后6个月移植骨量的相关性分析
Tab 3 Correlation analysis of the grafted bone volume at 6 months post-operation
| Influence factor | Test group | Control group | |||
|---|---|---|---|---|---|
| r | P | r | P | ||
| Width of apertura piriformis | 0.184 | 0.547 | 0.184 | 0.547 | |
| Width of alveolar crest | 0.256 | 0.398 | 0.256 | 0.547 | |
| Gender | 0.514 | 0.050 | 0.009 | 0.977 | |
| Age | 0.080 | 0.778 | -0.048 | 0.883 | |
| Cleft side | 0.259 | 0.352 | -0.369 | 0.238 | |
| Orthodontic treatment | -0.145 | 0.621 | 0.390 | 0.203 | |
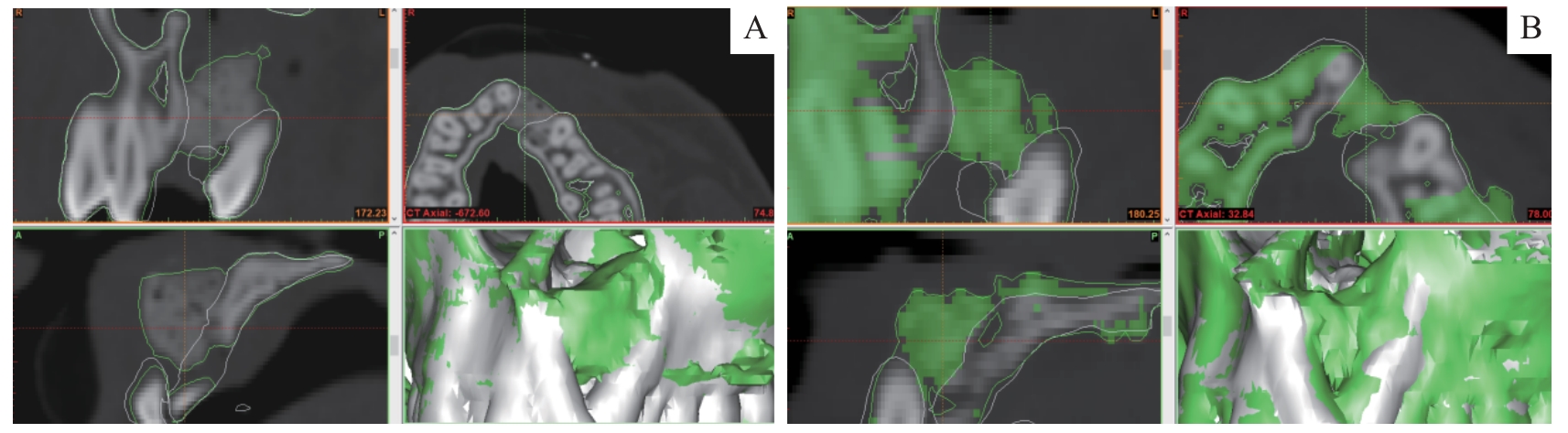
图4 试验组术后植骨效果Note: A. Effect immediately after surgery. B. Effect at 6 months post-operation.
Fig 4 Postoperative bone grafting effect in the test group
| Influence factor | Test group | Control group | |||
|---|---|---|---|---|---|
| r | P | r | P | ||
| Width of apertura piriformis | 0.337 | 0.260 | 0.265 | 0.406 | |
| Width of alveolar crest | 0.283 | 0.348 | 0.207 | 0.519 | |
| Gender | -0.393 | 0.165 | 0.249 | 0.434 | |
| Age | 0.056 | 0.842 | 0.549 | 0.067 | |
| Cleft side | -0.002 | 0.993 | 0.379 | 0.224 | |
| Orthodontic treatment | 0.086 | 0.770 | -0.276 | 0.386 | |
表4 术后6个月的骨吸收率相关性分析
Tab 4 Correlation analysis of bone resorption rate at 6 months post-operation
| Influence factor | Test group | Control group | |||
|---|---|---|---|---|---|
| r | P | r | P | ||
| Width of apertura piriformis | 0.337 | 0.260 | 0.265 | 0.406 | |
| Width of alveolar crest | 0.283 | 0.348 | 0.207 | 0.519 | |
| Gender | -0.393 | 0.165 | 0.249 | 0.434 | |
| Age | 0.056 | 0.842 | 0.549 | 0.067 | |
| Cleft side | -0.002 | 0.993 | 0.379 | 0.224 | |
| Orthodontic treatment | 0.086 | 0.770 | -0.276 | 0.386 | |
| Analytical dimension | Test group | Control group |
|---|---|---|
| Cleft side | ||
| Postoperative BMD at 6m of the cleft side/HU | 889.8±258.2 | 455.4±84.9 |
| Immediate postoperative BMD of the cleft side/HU | 692.9±123.6 | 420.8±57.5 |
| Correlation analysis | r=0.576, P=0.025 | r=0.348, P=0.269 |
| Normal side | ||
| Postoperative BMD at 6m of the normal side/ HU | 350.3±14.8 | 358.5±28.4 |
| Immediate postoperative BMD of the normal side/ HU | 355.2±19.5 | 368.4±27.4 |
| Correlation analysis | r=0.235, P=0.440 | r=0.272, P=0.390 |
表5 术后6个月的骨密度相关性检验
Tab 5 Correlation analysis of BMD at 6 months post-operation
| Analytical dimension | Test group | Control group |
|---|---|---|
| Cleft side | ||
| Postoperative BMD at 6m of the cleft side/HU | 889.8±258.2 | 455.4±84.9 |
| Immediate postoperative BMD of the cleft side/HU | 692.9±123.6 | 420.8±57.5 |
| Correlation analysis | r=0.576, P=0.025 | r=0.348, P=0.269 |
| Normal side | ||
| Postoperative BMD at 6m of the normal side/ HU | 350.3±14.8 | 358.5±28.4 |
| Immediate postoperative BMD of the normal side/ HU | 355.2±19.5 | 368.4±27.4 |
| Correlation analysis | r=0.235, P=0.440 | r=0.272, P=0.390 |
| [1] | SLEMAN N. Alveolar cleft reconstruction using iliac bone graft: a clinical case report[J]. Ann Med Surg (Lond), 2023, 85(11): 5776-5781. |
| [2] | KAURA A S, SRINIVASA D R, KASTEN S J. Optimal timing of alveolar cleft bone grafting for maxillary clefts in the cleft palate population[J]. J Craniofac Surg, 2018, 29(6): 1551-1557. |
| [3] | SANTIAGO P E, SCHUSTER L A, LEVY-BERCOWSKI D. Management of the alveolar cleft[J]. Clin Plast Surg, 2014, 41(2): 219-232. |
| [4] | STREET M, GAO R, MARTIS W, et al. The efficacy of local autologous bone dust: a systematic review[J]. Spine Deform, 2017, 5(4): 231-237. |
| [5] | HORSWELL B B, HENDERSON J M. Secondary osteoplasty of the alveolar cleft defect[J]. J Oral Maxillofac Surg, 2003, 61(9): 1082-1090. |
| [6] | COHEN M, FIGUEROA A A, HAVIV Y, et al. Iliac versus cranial bone for secondary grafting of residual alveolar clefts[J]. Plast Reconstr Surg, 1991, 87(3): 423-427; discussion428. |
| [7] | EICHHORN W, BLESSMANN M, POHLENZ P, et al. Primary osteoplasty using calvarian bone in patients with cleft lip, alveolus and palate[J]. J Craniomaxillofac Surg, 2009, 37(8): 429-433. |
| [8] | KALAAJI A, LILJA J, ELANDER A, et al. Tibia as donor site for alveolar bone grafting in patients with cleft lip and palate: long-term experience[J]. Scand J Plast Reconstr Surg Hand Surg, 2001, 35(1): 35-42. |
| [9] | BESLY W, WARD BOOTH P. Technique for harvesting tibial cancellous bone modified for use in children[J]. Br J Oral Maxillofac Surg, 1999, 37(2): 129-133. |
| [10] | BAUMHAUER J, PINZUR M S, DONAHUE R, et al. Site selection and pain outcome after autologous bone graft harvest[J]. Foot Ankle Int, 2014, 35(2): 104-107. |
| [11] | ENEMARK H, JENSEN J, BOSCH C. Mandibular bone graft material for reconstruction of alveolar cleft defects: long-term results[J]. Cleft Palate Craniofac J, 2001, 38(2): 155-163. |
| [12] | SINDET-PEDERSEN S, ENEMARK H. Reconstruction of alveolar clefts with mandibular or iliac crest bone grafts: a comparative study[J]. J Oral Maxillofac Surg, 1990, 48(6): 554-558; discussion 559-560. |
| [13] | KOOLE R, BOSKER H, VAN DER DUSSEN F N. Late secondary autogenous bone grafting in cleft patients comparing mandibular (ectomesenchymal) and iliac crest (mesenchymal) grafts[J]. J Cranio Maxillofac Surg, 1989, 17: 28-30. |
| [14] | BÄHR W, COULON J P. Limits of the mandibular symphysis as a donor site for bone grafts in early secondary cleft palate osteoplasty[J]. Int J Oral Maxillofac Surg, 1996, 25(5): 389-393. |
| [15] | IŞıK G, YÜCE M Ö, KOÇAK-TOPBAŞ N, et al. Guided bone regeneration simultaneous with implant placement using bovine-derived xenograft with and without liquid platelet-rich fibrin: a randomized controlled clinical trial[J]. Clin Oral Investig, 2021, 25(9): 5563-5575. |
| [16] | MIRON R J, MORASCHINI V, FUJIOKA-KOBAYASHI M, et al. Use of platelet-rich fibrin for the treatment of periodontal intrabony defects: a systematic review and meta-analysis[J]. Clin Oral Investig, 2021, 25(5): 2461-2478. |
| [17] | UZUN B C, ERCAN E, TUNALı M. Effectiveness and predictability of titanium-prepared platelet-rich fibrin for the management of multiple gingival recessions[J]. Clin Oral Investig, 2018, 22(3): 1345-1354. |
| [18] | THUAKSUBAN N, NUNTANARANONT T, PRIPATNANONT P. A comparison of autogenous bone graft combined with deproteinized bovine bone and autogenous bone graft alone for treatment of alveolar cleft[J]. Int J Oral Maxillofac Surg, 2010, 39(12): 1175-1180. |
| [19] | DA SILVA H F, GOULART D R, SVERZUT A T, et al. Comparison of two anorganic bovine bone in maxillary sinus lift: a split-mouth study with clinical, radiographical, and histomorphometrical analysis[J]. Int J Implant Dent, 2020, 6(1): 17. |
| [20] | LU J J, WANG Z S, ZHANG H Y, et al. Bone graft materials for alveolar bone defects in orthodontic tooth movement[J]. Tissue Eng Part B Rev, 2022, 28(1): 35-51. |
| [21] | LEE J H, YI G S, LEE J W, et al. Physicochemical characterization of porcine bone-derived grafting material and comparison with bovine xenografts for dental applications[J]. J Periodontal Implant Sci, 2017, 47(6): 388-401. |
| [22] | KIM D M, KANG H C, CHA H J, et al. Process development of a virally-safe dental xenograft material from porcine bones[J]. Korean J Microbiol, 2016, 52(2): 140-147. |
| [23] | BRACEY D N, SEYLER T M, JINNAH A H, et al. A decellularized porcine xenograft-derived bone scaffold for clinical use as a bone graft substitute: a critical evaluation of processing and structure[J]. J Funct Biomater, 2018, 9(3): 45. |
| [24] | LEE J S, SHIN H K, YUN J H, et al. Randomized clinical trial of maxillary sinus grafting using deproteinized porcine and bovine bone mineral[J]. Clin Implant Dent Relat Res, 2017, 19(1): 140-150. |
| [25] | SOHN D S, HEO J U, KWAK D H, et al. Bone regeneration in the maxillary sinus using an autologous fibrin-rich block with concentrated growth factors alone[J]. Implant Dent, 2011, 20(5): 389-395. |
| [26] | MOURÃO C F, VALIENSE H, MELO E R, et al. Obtention of injectable platelets rich-fibrin (i-PRF) and its polymerization with bone graft: technical note[J]. Rev Col Bras Cir, 2015, 42(6): 421-423. |
| [27] | SOHN D S, HUANG B, KIM J, et al. Utilization of autologous concentrated growth factors (CGF) enriched bone graft matrix (Sticky bone) and CGF-enriched fibrin membrane in Implant Dentistry[J]. Implant Adv. Clin. Dent. 2015;7:11-18. |
| [28] | TONY J B, PARTHASARATHY H, TADEPALLI A, et al. CBCT evaluation of sticky bone in horizontal ridge augmentation with and without collagen membrane-a randomized parallel arm clinical trial[J]. J Funct Biomater, 2022, 13(4): 194. |
| [29] | DARWISH M E D, ASKAR N A E, ABDEL-RASOUL M A, et al. Alveolar ridge preservation in mandibular molars using mixture of anorganic bovine bone (ABB) and autogenous particulate vs mixture of injectable platelets rich fibrin, ABB and autogenous particulates (sticky bone) (a randomized clinical trial)[J]. Act Scie Ortho, 2021, 4(2): 31-50. |
| [30] | 唐璟, 宋庆高. 影响牙槽突裂植骨术效果的相关因素[J]. 中国临床研究, 2021, 34(4): 554-557. |
| TANG J, SONG Q G. Factors influencing the effect of alveolar ridge bone grafting[J]. Chinese Journal of Clinical Research, 2021, 34(4): 554-557. | |
| [31] | 唐世杰, 石伦刚. 牙槽突裂植骨吸收的原因与对策[J]. 中国实用口腔科杂志, 2012, 5(6): 332-336. |
| TANG S J,SHI L G. The causes and countermeasures of bone absorption after alveolar cleft bone grafting[J].Chinese Journal of Practical Stomatology, 2012, 5(6): 332-336. | |
| [32] | 张勇, 杨育生, 吴忆来, 等. 牙槽突裂植骨吸收率的测量分析[J]. 上海口腔医学, 2012, 21(3): 308-311. |
| ZHANG Y, YANG Y S, WU Y L, et al. Measurement of the volume absorption of alveolar bone grafting[J].Shanghai Journal of Stomatology, 2012, 21(3): 308-311. | |
| [33] | JABBARI F, REISER E, THOR A, et al. Correlations between initial cleft size and dental anomalies in unilateral cleft lip and palate patients after alveolar bone grafting[J]. Upsala J Med Sci, 2016, 121(1): 33-37. |
| [34] | NART J, BARALLAT L, JIMENEZ D, et al. Radiographic and histological evaluation of deproteinized bovine bone mineral vs. deproteinized bovine bone mineral with 10% collagen in ridge preservation. A randomized controlled clinical trial[J]. Clin Oral Implants Res, 2017, 28(7): 840-848. |
| [35] | 王李娜, 王恩群. 牙源性颌骨囊肿术后自发性骨再生与Bio-Oss移植骨再生效果比较[J]. 医学信息, 2022, 35(5): 91-93. |
| WANG L N, WANG E Q. Comparison of the effect of spontaneous bone regeneration and Bio-Oss graft bone regeneration after odontogenic jaw cyst surgery[J]. Journal of Medical Information, 2022, 35(5): 91-93. | |
| [36] | 陈传鸿, 高丽荣, 张建全. 富自体浓缩生长因子结合Bio-Oss骨粉在颌骨囊肿术后骨缺损区的修复效果[J]. 江苏医药, 2022, 48(9): 926-930. |
| CHEN C H, GAO L R, ZHANG J Q. Repairing effect of autologous concentrated growth factor combined with Bio-Oss bone powder on the bone defect after jaw cyst surgery[J]. Jiangsu Medical Journal, 2022, 48(9): 926-930. | |
| [37] | RIZK M, NIEDERAU C, FLOREA A, et al. Periodontal ligament and alveolar bone remodeling during long orthodontic tooth movement analyzed by a novel user-independent 3D-methodology[J]. Sci Rep, 2023, 13(1): 19919. |
| [38] | 袁乐. 基于骨密度分布的牙槽松质骨本构模型研究[D]. 南京: 南京林业大学, 2024. |
| YUAN L, Study on the constitutive model of alveolar cancellous bone based onbone mineral density distribution[D]. Nan Jing: Nan Jing Forestry University, 2024. | |
| [39] | CHUGH T, GANESHKAR S V, REVANKAR A V, et al. Quantitative assessment of interradicular bone density in the maxilla and mandible: implications in clinical orthodontics[J]. Prog Orthod, 2013, 14(1): 38. |
| [40] | 康惠尹, 李春宏, 苏凯, 等. Bio-oss/富血小板纤维蛋白复合物修复牙槽骨缺损区后牙移动的效果及可行性[J]. 临床和实验医学杂志, 2020, 19(4): 394-397. |
| KANG H Y, LI C H, SU K, et al. Effect of Bio-oss/platelet-rich fibrin (PRF) complex in repair of alveolar bone defect on orthodontic tooth movement and its and feasibility[J]. Journal of Clinical and Experimental Medicine, 2020, 19(4): 394-397. | |
| [41] | ALOORKER S, SHETTY M, HEGDE C. Effect of osseodensification on bone density and crestal bone levels: a split-mouth study[J]. J Contemp Dent Pract, 2022, 23(2): 162-168. |
| [42] | 陶桃, 蒋勇. 锥形束CT评价种植区牙槽骨骨密度的应用研究[J]. 中国医疗美容, 2019, 9(8): 118-123. |
| TAO T, JIANG Y. Evaluation of Bone Mineral Density in Implant Area by CBCT[J]. China Medical Cosmetology, 2019, 9(8): 118-123. |
| [1] | 刘辰骏, 尹博浩, 孙辉, 张伟. 非侵入性影像学技术在骨质疏松症中的应用[J]. 上海交通大学学报(医学版), 2023, 43(3): 385-390. |
| [2] | 禹茜, 孙俊楠, 张姣姣, 高月, 王虎, 于洋, 王海嵘, 洪雯. 成人胸部CT胸骨皮质比例对骨量低下及骨质疏松诊断效能的探究[J]. 上海交通大学学报(医学版), 2023, 43(10): 1274-1281. |
| [3] | 常安瑾,钱莹,陈晓农,等. 维持性血液透析患者低骨密度发生及相关因素研究[J]. 上海交通大学学报(医学版), 2016, 36(1): 59-. |
| [4] | 董正杰,程 竑,王德芳,等. 术区锥形束CT颌骨密度与种植体植入扭矩的相关性研究[J]. 上海交通大学学报(医学版), 2014, 34(6): 894-. |
| [5] | 吴萌萌,陈芝国,陆金华,等. 老年男性单项血脂指标和血脂危险分层与骨密度的关系[J]. 上海交通大学学报(医学版), 2014, 34(6): 880-. |
| [6] | 朱金宏, 易诚青, 马春辉, 等. 骨小梁金属髋臼假体对人工全髋关节置换术后髋臼侧假体周围骨密度的影响[J]. , 2012, 32(12): 1540-. |
| [7] | 朱洁萍, 陶敏芳, 胡伟伟, 等. 围绝经期妇女骨密度与肌肉及脂肪含量的关系[J]. , 2009, 29(8): 1005-. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||