
上海交通大学学报(医学版) ›› 2025, Vol. 45 ›› Issue (5): 585-596.doi: 10.3969/j.issn.1674-8115.2025.05.007
收稿日期:2024-12-30
接受日期:2025-02-26
出版日期:2025-05-28
发布日期:2025-05-21
通讯作者:
艾松涛,主任医师,博士;电子信箱: ai.songtao@qq.com。作者简介:张钲佳(1999—),女,硕士生;电子信箱: GeorgiaZhang@sjtu.edu.cn。
基金资助:
ZHANG Zhengjia, LI Xiaomin, ZHOU Xin, MA Hairong, AI Songtao( )
)
Received:2024-12-30
Accepted:2025-02-26
Online:2025-05-28
Published:2025-05-21
Contact:
AI Songtao, E-mail: ai.songtao@qq.com.Supported by:摘要:
目的·初步探讨高阶磁共振功能成像在评估骨与软组织肿瘤良恶性及化学治疗(化疗)效果中的应用价值。方法·纳入2014年10月至2024年12月在上海交通大学医学院附属第九人民医院骨科接受治疗且临床确诊为骨与软组织肿瘤的患者,根据患者磁共振检查方法,分为常规组和酰胺质子转移加权成像(amide proton transfer-weighted imaging,APTw)组。所有患者术前均行常规磁共振成像(magnetic resonance imaging,MRI)、弥散加权成像(diffusion-weighted imaging,DWI)及动态增强成像(dynamic contrast-enhanced imaging,DCE),APTw组患者在此基础上额外接受APTw成像。2组患者根据病理结果各分为非恶性病变组和恶性病变组;APTw组中的恶性病变患者根据入组前是否接受化疗,进一步分为未化疗组和化疗组。收集患者临床信息、影像学资料,分析肿瘤最大截面的APT值、表观弥散系数(apparent diffusion coefficient,ADC)及时间信号强度曲线(time intensity curve,TIC),以比较磁共振APTw、DWI及DCE在肿瘤诊断及评估化疗后改变中的应用价值。结果·共入组85例患者(男性51例,女性34例),年龄10~84岁,平均(43.05±17.62)岁。常规组51例(非恶性病变16例,恶性病变35例),APTw组34例(非恶性病变5例,恶性病变29例;恶性病变患者中未化疗者23例,化疗者6例)。临床和影像学特征中,仅常规组的边界是否清楚与APTw组的肿瘤最大直径在各自的恶性与非恶性病变患者间差异具有统计学意义( P<0.05)。在APTw组中,恶性病变与非恶性病变患者的APT值差异具有统计学意义( P<0.001);进一步分析,恶性病变未化疗组的APT值显著低于恶性病变化疗组( P<0.001),但恶性病变化疗组与非恶性病变组的APT值差异无统计学意义( P>0.05)。常规组与APTw组的ADC值及TIC分型在2组各自的恶性病变与非恶性病变组间差异均无统计学意义( P>0.05)。APTw组诊断模型(常规MRI+DWI+DCE+APTw)对骨与软组织恶性与非恶性病变的诊断效能曲线下面积(area under curve,AUC)大于常规组诊断模型(常规MRI+DWI+DCE),差异具有统计学意义( P<0.05),且APTw组诊断模型的约登指数及特异度均更高。结论·APTw成像作为一种高阶磁共振功能成像,可以评估骨与软组织肿瘤的良恶性及化疗后改变,是常规MRI、DWI及DCE成像评估的有益补充,为骨与软组织肿瘤的无创诊疗评估提供了新的临床工具。
中图分类号:
张钲佳, 李小敏, 周鑫, 马海荣, 艾松涛. 高阶磁共振功能成像评估骨与软组织肿瘤价值初探[J]. 上海交通大学学报(医学版), 2025, 45(5): 585-596.
ZHANG Zhengjia, LI Xiaomin, ZHOU Xin, MA Hairong, AI Songtao. Preliminary study on the value of high-order functional magnetic resonance imaging in the evaluation of bone and soft tissue tumors[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2025, 45(5): 585-596.
| Parameter | T1WI | T2WI | T2-SPAIR | DWI | DCE | APTw |
|---|---|---|---|---|---|---|
| Sequence | TSE | TSE | TSE | EPI | TSE | TSE |
| Plane | Axial | Axial | Coronal | Axial | Axial | Axial |
| Fat saturation | NO | NO | SPAIR | SPAIR | NO | SPIR |
| Time to repeat/ms | 672 | 3 000 | 3 200 | 3 048 | 638 | 7 300 |
| Time to echo/ms | 13 | 75 | 60 | 56 | 15 | 8.3 |
| Thickness/mm | 4 | 4 | 4 | 5 | 4 | 6 |
| FOV/mm | 250×400 | 300×379 | 280×350 | 300×450 | 300×379 | 230×180 |
| Matrix | 312×418 | 352×375 | 352×368 | 152×197 | 352×402 | 128×100 |
| Slice gap/mm | 0.4 | 0.4 | 0.4 | 0.5 | 0.4 | 0 |
| NSA | 1 | 1 | 1 | 1 | 1 | 1 |
| b value/(s·mm -2) | ‒ | ‒ | ‒ | 0, 1 000 | ‒ | ‒ |
| Scan time | 2 min 5 s | 2 min 30 s | 2 min 14 s | 1 min 41 s | 2 min 32 s | 3 min 37 s |
表1 MRI扫描参数
Tab 1 MRI scanning parameters
| Parameter | T1WI | T2WI | T2-SPAIR | DWI | DCE | APTw |
|---|---|---|---|---|---|---|
| Sequence | TSE | TSE | TSE | EPI | TSE | TSE |
| Plane | Axial | Axial | Coronal | Axial | Axial | Axial |
| Fat saturation | NO | NO | SPAIR | SPAIR | NO | SPIR |
| Time to repeat/ms | 672 | 3 000 | 3 200 | 3 048 | 638 | 7 300 |
| Time to echo/ms | 13 | 75 | 60 | 56 | 15 | 8.3 |
| Thickness/mm | 4 | 4 | 4 | 5 | 4 | 6 |
| FOV/mm | 250×400 | 300×379 | 280×350 | 300×450 | 300×379 | 230×180 |
| Matrix | 312×418 | 352×375 | 352×368 | 152×197 | 352×402 | 128×100 |
| Slice gap/mm | 0.4 | 0.4 | 0.4 | 0.5 | 0.4 | 0 |
| NSA | 1 | 1 | 1 | 1 | 1 | 1 |
| b value/(s·mm -2) | ‒ | ‒ | ‒ | 0, 1 000 | ‒ | ‒ |
| Scan time | 2 min 5 s | 2 min 30 s | 2 min 14 s | 1 min 41 s | 2 min 32 s | 3 min 37 s |
| Variable | Control group ( n=51) | APTw group ( n=34) | P value | ||||
|---|---|---|---|---|---|---|---|
| Non-malignant lesion ( n=16) | Malignant lesion ( n=35) | P value | Non-malignant lesion ( n=5) | Malignant lesion ( n=29) | P value | ||
| Gender/ n(%) | 0.068 | 0.618 | 0.119 | ||||
| Male | 5 (31.3) | 22 (62.9) | 3 (60.0) | 21 (72.4) | |||
| Female | 11 (68.8) | 13 (37.1) | 2 (40.0) | 8 (27.6) | |||
| Age/year | 39.00±12.87 | 47.40±17.57 | 0.111 | 41.80±12.46 | 40.24±20.10 | 0.925 | 0.317 |
| Maximum diameter/cm | 4.80 (5.28) | 7.69±3.13 | 0.082 | 4.24±0.83 | 8.14±4.33 | 0.038 | 0.986 |
| Margin/ n(%) | 0.001 | 0.146 | 0.509 | ||||
| Clear | 14 (87.5) | 13 (37.1) | 4 (80.0) | 11 (37.9) | |||
| Unclear | 2 (12.5) | 22 (62.9) | 1 (20.0) | 18 (62.1) | |||
| Signal/ n(%) | 0.187 | 0.570 | 0.624 | ||||
| Homogeneous | 7 (43.8) | 8 (22.9) | 2 (40.0) | 6 (20.7) | |||
| Heterogeneous | 9 (56.3) | 27 (77.1) | 3 (60.0) | 23 (79.3) | |||
| Shape/ n(%) | 0.157 | 0.205 | 0.595 | ||||
| Regular | 6 (37.5) | 6 (17.1) | 2 (40.0) | 4 (13.8) | |||
| Irregular | 10 (62.5) | 29 (82.9) | 3 (60.0) | 25 (86.2) | |||
| Peritumoral edema/ n(%) | 0.115 | 0.591 | 0.632 | ||||
| No | 8 (50.0) | 9 (25.7) | 2 (40.0) | 7 (24.1) | |||
| Yes | 8 (50.0) | 26 (74.3) | 3 (60.0) | 22 (75.9) | |||
| Cortical bone destruction/ n(%) | 1.000 | 1.000 | 0.257 | ||||
| No | 1 (6.3) | 2 (5.7) | 1 (20.0) | 4 (13.8) | |||
| Yes | 15 (93.8) | 33 (94.3) | 4 (80.0) | 25 (86.2) | |||
表2 患者临床及常规影像学资料
Tab 2 Patients′ clinical and conventional imaging characteristics
| Variable | Control group ( n=51) | APTw group ( n=34) | P value | ||||
|---|---|---|---|---|---|---|---|
| Non-malignant lesion ( n=16) | Malignant lesion ( n=35) | P value | Non-malignant lesion ( n=5) | Malignant lesion ( n=29) | P value | ||
| Gender/ n(%) | 0.068 | 0.618 | 0.119 | ||||
| Male | 5 (31.3) | 22 (62.9) | 3 (60.0) | 21 (72.4) | |||
| Female | 11 (68.8) | 13 (37.1) | 2 (40.0) | 8 (27.6) | |||
| Age/year | 39.00±12.87 | 47.40±17.57 | 0.111 | 41.80±12.46 | 40.24±20.10 | 0.925 | 0.317 |
| Maximum diameter/cm | 4.80 (5.28) | 7.69±3.13 | 0.082 | 4.24±0.83 | 8.14±4.33 | 0.038 | 0.986 |
| Margin/ n(%) | 0.001 | 0.146 | 0.509 | ||||
| Clear | 14 (87.5) | 13 (37.1) | 4 (80.0) | 11 (37.9) | |||
| Unclear | 2 (12.5) | 22 (62.9) | 1 (20.0) | 18 (62.1) | |||
| Signal/ n(%) | 0.187 | 0.570 | 0.624 | ||||
| Homogeneous | 7 (43.8) | 8 (22.9) | 2 (40.0) | 6 (20.7) | |||
| Heterogeneous | 9 (56.3) | 27 (77.1) | 3 (60.0) | 23 (79.3) | |||
| Shape/ n(%) | 0.157 | 0.205 | 0.595 | ||||
| Regular | 6 (37.5) | 6 (17.1) | 2 (40.0) | 4 (13.8) | |||
| Irregular | 10 (62.5) | 29 (82.9) | 3 (60.0) | 25 (86.2) | |||
| Peritumoral edema/ n(%) | 0.115 | 0.591 | 0.632 | ||||
| No | 8 (50.0) | 9 (25.7) | 2 (40.0) | 7 (24.1) | |||
| Yes | 8 (50.0) | 26 (74.3) | 3 (60.0) | 22 (75.9) | |||
| Cortical bone destruction/ n(%) | 1.000 | 1.000 | 0.257 | ||||
| No | 1 (6.3) | 2 (5.7) | 1 (20.0) | 4 (13.8) | |||
| Yes | 15 (93.8) | 33 (94.3) | 4 (80.0) | 25 (86.2) | |||
| Variable | Radiologist 1 | Radiologist 2 | ICC/ κ | 95% CI |
|---|---|---|---|---|
| APT | 2.50% (1.23%) | 2.63% (1.09%) | 0.977 | 0.954‒0.988 |
| ADC/(10 -3·mm 2·s -1) | 1.01 (0.67) | 1.08 (0.69) | 0.964 | 0.929‒0.982 |
| TIC (Ⅰ/Ⅱ/Ⅲ)/ n(%) | 17 (50.0)/14 (41.2)/3 (8.8) | 16 (47.1)/15 (44.1)/3 (8.8) | 0.847 | 0.678‒1.000 |
表3 APTw组 2名医师的组内相关系数检验
Tab 3 ICCs between the two radiologists in the APTw group
| Variable | Radiologist 1 | Radiologist 2 | ICC/ κ | 95% CI |
|---|---|---|---|---|
| APT | 2.50% (1.23%) | 2.63% (1.09%) | 0.977 | 0.954‒0.988 |
| ADC/(10 -3·mm 2·s -1) | 1.01 (0.67) | 1.08 (0.69) | 0.964 | 0.929‒0.982 |
| TIC (Ⅰ/Ⅱ/Ⅲ)/ n(%) | 17 (50.0)/14 (41.2)/3 (8.8) | 16 (47.1)/15 (44.1)/3 (8.8) | 0.847 | 0.678‒1.000 |
| Variable | Non-malignant lesions group ( n=5) | Malignant lesions group ( n=29) | U/ χ2 | P value |
|---|---|---|---|---|
| APT | 4.52%±0.76% | 2.47% (0.56%) | 5.00 | <0.001 |
| ADC/(10 -3·mm 2·s -1) | 1.37±0.52 | 1.03 (0.66) | 44.00 | 0.527 |
| TIC(Ⅰ/Ⅱ/Ⅲ)/ n(%) | 3 (60.0)/1 (20.1)/1 (20.0) | 14 (48.3)/13 (44.8)/2 (6.9) | 1.59 | 0.453 |
表4 APTw组中非恶性与恶性病变患者的 APT、 ADC值及 TIC分型
Tab 4 APT and ADC values, and TIC classifications between non-malignant and malignant lesions in the APTw group
| Variable | Non-malignant lesions group ( n=5) | Malignant lesions group ( n=29) | U/ χ2 | P value |
|---|---|---|---|---|
| APT | 4.52%±0.76% | 2.47% (0.56%) | 5.00 | <0.001 |
| ADC/(10 -3·mm 2·s -1) | 1.37±0.52 | 1.03 (0.66) | 44.00 | 0.527 |
| TIC(Ⅰ/Ⅱ/Ⅲ)/ n(%) | 3 (60.0)/1 (20.1)/1 (20.0) | 14 (48.3)/13 (44.8)/2 (6.9) | 1.59 | 0.453 |
| Variable | Non-chemotherapy group ( n=23) | Chemotherapy group ( n=6) | U/ χ2 | P value |
|---|---|---|---|---|
| APT | 2.43%±0.23% | 3.67%±0.24% | 138.00 | <0.001 |
| ADC/(10 -3·mm 2·s -1) | 1.00 (0.66) | 1.31±0.65 | 75.00 | 0.643 |
| TIC(Ⅰ/Ⅱ/Ⅲ)/ n(%) | 13 (56.5)/9 (39.1)/1 (4.3) | 1 (16.7)/4 (66.7)/1 (16.7) | 3.42 | 0.181 |
表5 APTw组恶性病变患者中化疗者与未化疗者的 APT、 ADC值及 TIC分型
Tab 5 APT and ADC values, and TIC classifications in APTw group patients with malignant lesions, comparing those who received chemotherapy with those who did not
| Variable | Non-chemotherapy group ( n=23) | Chemotherapy group ( n=6) | U/ χ2 | P value |
|---|---|---|---|---|
| APT | 2.43%±0.23% | 3.67%±0.24% | 138.00 | <0.001 |
| ADC/(10 -3·mm 2·s -1) | 1.00 (0.66) | 1.31±0.65 | 75.00 | 0.643 |
| TIC(Ⅰ/Ⅱ/Ⅲ)/ n(%) | 13 (56.5)/9 (39.1)/1 (4.3) | 1 (16.7)/4 (66.7)/1 (16.7) | 3.42 | 0.181 |
| Variable | Non-malignant lesions group ( n=16) | Malignant lesions group ( n=35) | U/ χ2 | P value |
|---|---|---|---|---|
| ADC/(10 -3·mm 2·s -1) | 1.33±0.55 | 1.00 (0.89) | 260.50 | 0.690 |
| TIC(Ⅰ/Ⅱ/Ⅲ)/ n(%) | 10 (62.5)/4 (25.0)/2 (12.5) | 17 (48.6)/13 (37.1)/5 (14.3) | 0.91 | 0.633 |
表6 常规组中非恶性与恶性病变患者的 ADC值及 TIC分型
Tab 6 ADC values and TIC classification between non-malignant and malignant lesions in the control group
| Variable | Non-malignant lesions group ( n=16) | Malignant lesions group ( n=35) | U/ χ2 | P value |
|---|---|---|---|---|
| ADC/(10 -3·mm 2·s -1) | 1.33±0.55 | 1.00 (0.89) | 260.50 | 0.690 |
| TIC(Ⅰ/Ⅱ/Ⅲ)/ n(%) | 10 (62.5)/4 (25.0)/2 (12.5) | 17 (48.6)/13 (37.1)/5 (14.3) | 0.91 | 0.633 |
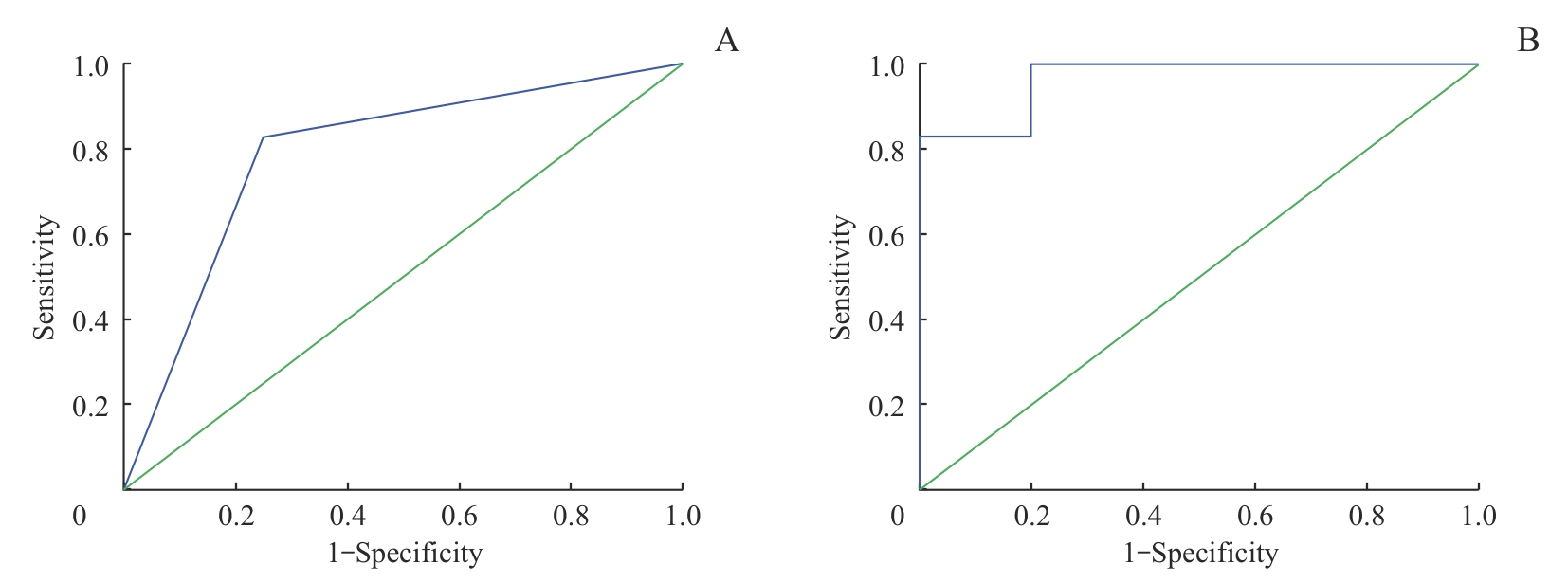
图3 骨与软组织恶性与非恶性病变诊断效能的 ROC曲线Note: A. The diagnostic model of the control group (MRI+DWI+DCE). B. The diagnostic model of the APTw group (MRI+DWI+DCE+APTw).
Fig 3 ROC curves showing the diagnostic efficacy of different models for distinguishing malignant from non-malignant bone and soft tissue lesions
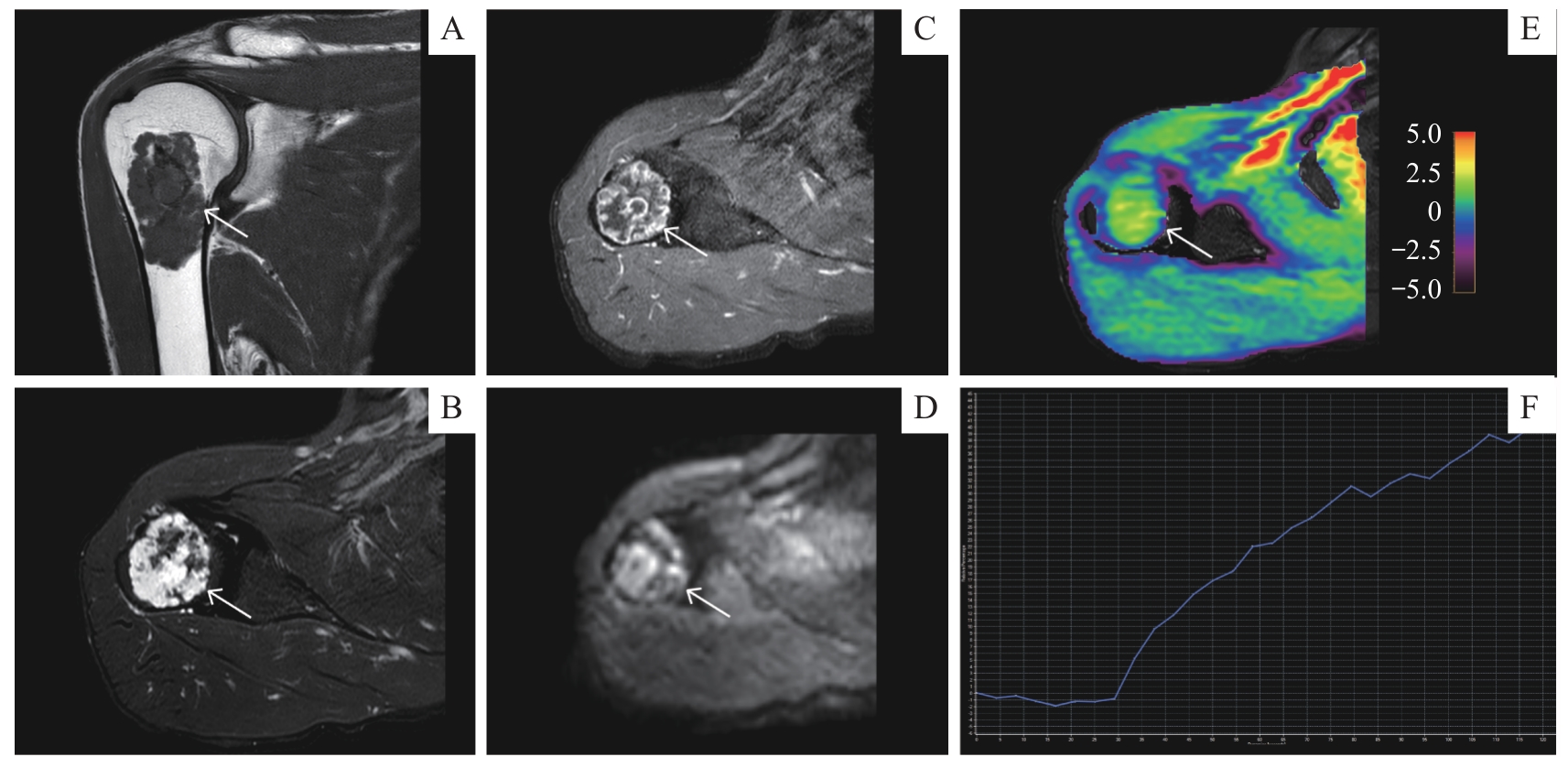
图4 APTw成像在恶性骨肿瘤中的应用Note: A 52-year-old male with chondrosarcoma of the right humerus. A. Coronal T1-weighted MRI sequence. B. Axial T2-weighted fat-saturated MRI sequence. C. Axial contrast-enhanced T1-weighted MRI sequence. D. Axial DWI ( b=1 000 s·mm -2) sequence. E. Axial APT image fused with axial T2WI (the color bar indicates the APT values). F. TIC classification (type Ⅰ).
Fig 4 Application of APTw imaging to malignant bone tumor
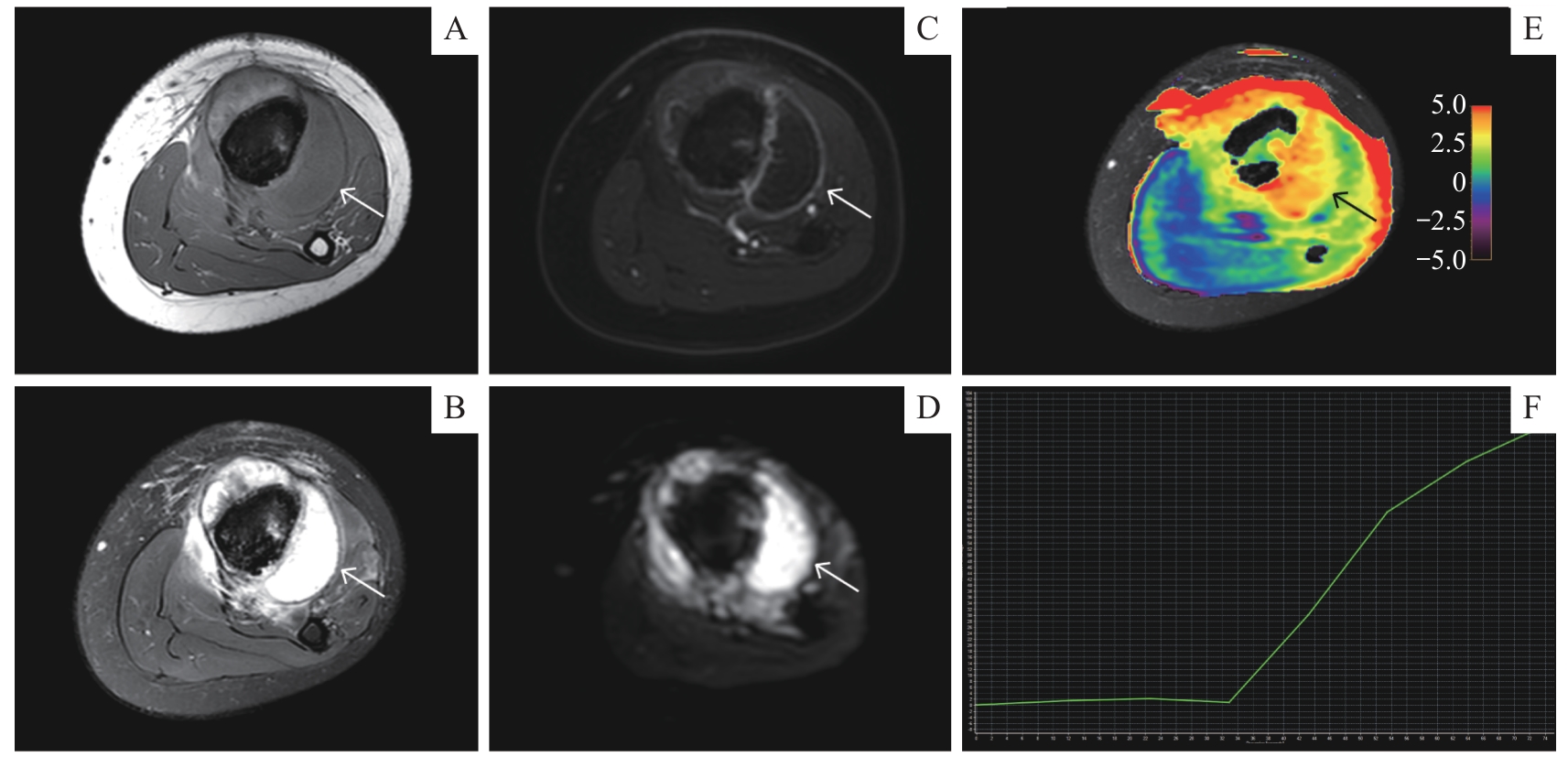
图5 APTw成像在恶性骨肿瘤新辅助化疗中的应用Note: A 12-year-old male with osteosarcoma in the left tibia showed chemotherapy-related changes. A. Axial T1-weighted MRI sequence. B. Axial T2-weighted fat-saturated MRI sequence. C. Axial contrast-enhanced T1-weighted MRI sequence. D. Axial DWI ( b=1 000 s·mm -2) sequence. E. Axial APT image fused with axial T2WI (the color bar indicates the APT values). F. TIC classification (type Ⅰ).
Fig 5 Application of APTw imaging in neoadjuvant chemotherapy for malignant bone tumor
| 1 | CHOI J H, RO J Y. The 2020 WHO classification of tumors of bone: an updated review[J]. Adv Anat Pathol, 2021, 28(3): 119-138. |
| 2 | CHOI J H, RO J Y. The 2020 WHO classification of tumors of soft tissue: selected changes and new entities[J]. Adv Anat Pathol, 2021, 28(1): 44-58. |
| 3 | WANG Y A, YAN Q J, FAN C M, et al. Overview and countermeasures of cancer burden in China[J]. Sci China Life Sci, 2023, 66(11): 2515-2526. |
| 4 | COLE S, MATTHEW GIANFERANTE D, ZHU B, et al. Osteosarcoma: a surveillance, epidemiology, and end results program-based analysis from 1975 to 2017[J]. Cancer, 2022, 128(11): 2107-2118. |
| 5 | JAFARI F, JAVDANSIRAT S, SANAIE S, et al. Osteosarcoma: a comprehensive review of management and treatment strategies[J]. Ann Diagn Pathol, 2020, 49: 151654. |
| 6 | KUNISADA T, NAKATA E, FUJIWARA T, et al. Soft-tissue sarcoma in adolescents and young adults[J]. Int J Clin Oncol, 2023, 28(1): 1-11. |
| 7 | CHOI J H, RO J Y. The recent advances in molecular diagnosis of soft tissue tumors[J]. Int J Mol Sci, 2023, 24(6): 5934. |
| 8 | TANAKA K, OZAKI T. Adjuvant and neoadjuvant chemotherapy for soft tissue sarcomas: JCOG Bone and Soft Tissue Tumor Study Group[J]. Jpn J Clin Oncol, 2021, 51(2): 180-184. |
| 9 | YUAN W Z, YU Q Y, WANG Z, et al. Efficacy of diffusion-weighted imaging in neoadjuvant chemotherapy for osteosarcoma: a systematic review and meta-analysis[J]. Acad Radiol, 2022, 29(2): 326-334. |
| 10 | HABRE C, DABADIE A, LOUNDOU A D, et al. Diffusion-weighted imaging in differentiating mid-course responders to chemotherapy for long-bone osteosarcoma compared to the histologic response: an update[J]. Pediatr Radiol, 2021, 51(9): 1714-1723. |
| 11 | GUEDES A, NAKAGAWA S A. Biopsy of bone tumors: a literature review[J]. Rev Assoc Med Bras (1992), 2024, 70(suppl 1): e2024S131. |
| 12 | WHELAN J S, DAVIS L E. Osteosarcoma, chondrosarcoma, and chordoma[J]. J Clin Oncol, 2018, 36(2): 188-193. |
| 13 | LI J L, XU Y, XIANG Y S, et al. The value of amide proton transfer MRI in the diagnosis of malignant and benign urinary bladder lesions: comparison with diffusion-weighted imaging[J]. J Magn Reson Imaging, 2024, 60(3): 1124-1133. |
| 14 | SETIAWATI R, NOVARIYANTO B, RAHARDJO P, et al. Characteristic of apparent diffusion coefficient and time intensity curve analysis of dynamic contrast enhanced MRI in osteosarcoma histopathologic subtypes[J]. Int J Med Sci, 2023, 20(2): 163-171. |
| 15 | COSTA F M, CANELLA C, GASPARETTO E. Advanced magnetic resonance imaging techniques in the evaluation of musculoskeletal tumors[J]. Radiol Clin North Am, 2011, 49(6): 1325-1358, Ⅶ-Ⅷ. |
| 16 | KHALIFA F, SOLIMAN A, EL-BAZ A, et al. Models and methods for analyzing DCE-MRI: a review[J]. Med Phys, 2014, 41(12): 124301. |
| 17 | 赵傲, 武新英, 付彤, 等. DWI、DCE联合APT成像在鉴别乳腺良恶性病变中的价值研究[J]. 中国医疗设备, 2024, 39(6): 124-130, 155. |
| ZHAO A, WU X Y, FU T, et al. Value of DWI, DCE and APT imaging in identifying benign and malignant breast lesions[J]. China Medical Devices, 2024, 39(6): 124-130, 155. | |
| 18 | KUANG F, YAN Z P, LI H L, et al. Diagnostic accuracy of diffusion-weighted MRI for differentiation of cervical cancer and benign cervical lesions at 3.0T: comparison with routine MRI and dynamic contrast-enhanced MRI[J]. J Magn Reson Imaging, 2015, 42(4): 1094-1099. |
| 19 | ZHOU J Y, HEO H Y, KNUTSSON L, et al. APT-weighted MRI: techniques, current neuro applications, and challenging issues[J]. J Magn Reson Imaging, 2019, 50(2): 347-364. |
| 20 | WU M H, JIANG T L, GUO M, et al. Amide proton transfer-weighted imaging and derived radiomics in the classification of adult-type diffuse gliomas[J]. Eur Radiol, 2024, 34(5): 2986-2996. |
| 21 | LI Y, LIN C Y, QI Y F, et al. Non-invasive differentiation of endometrial adenocarcinoma from benign lesions in the uterus by utilization of amide proton transfer-weighted MRI[J]. Mol Imaging Biol, 2021, 23(3): 446-455. |
| 22 | LIU Z, WEN J, WANG M, et al. Breast amide proton transfer imaging at 3 T: diagnostic performance and association with pathologic characteristics[J]. J Magn Reson Imaging, 2023, 57(3): 824-833. |
| 23 | DENG H Z, ZHANG H W, HUANG B, et al. Advances in diffuse glioma assessment: preoperative and postoperative applications of chemical exchange saturation transfer[J]. Front Neurosci, 2024, 18: 1424316. |
| 24 | QAMAR S, KING A D, AI Q H, et al. Pre-treatment amide proton transfer imaging predicts treatment outcome in nasopharyngeal carcinoma[J]. Eur Radiol, 2020, 30(11): 6339-6347. |
| 25 | ZHANG N, SONG Q W, LIANG H B, et al. Early prediction of pathological response to neoadjuvant chemotherapy of breast tumors: a comparative study using amide proton transfer-weighted, diffusion weighted and dynamic contrast enhanced MRI[J]. Front Med (Lausanne), 2024, 11: 1295478. |
| 26 | 史天亮, 杨崇双, 刘元早, 等. APT成像在宫颈癌同步根治性放化疗疗效评估中的价值[J]. 磁共振成像, 2024, 15(1): 132-136. |
| SHI T L, YANG C S, LIU Y Z, et al. The value of APT imaging in evaluating the therapeutic efficacy of concurrent chemoradiotherapy for cervical cancer[J]. Chinese Journal of Magnetic Resonance Imaging, 2024, 15(1): 132-136. | |
| 27 | 刘斯润, 蔡香然, 邱麟. 新版(2020)WHO骨肿瘤分类解读[J]. 磁共振成像, 2020, 11(12): 1086-1091. |
| LIU S R, CAI X R, QIU L. Interpretation of the new WHO classification of bone tumors (2020) [J]. Chinese Journal of Magnetic Resonance Imaging, 2020, 11(12): 1086-1091. | |
| 28 | 方三高, 魏建国, 陈真伟. WHO(2020)软组织肿瘤分类[J]. 临床与实验病理学杂志, 2020, 36(9): 1132-1134. |
| FANG S G, WEI J G, CHEN Z W. WHO classification of soft tissue tumors (2020) [J]. Chinese Journal of Clinical and Experimental Pathology, 2020, 36(9): 1132-1134. | |
| 29 | YABUUCHI H, FUKUYA T, TAJIMA T, et al. Salivary gland tumors: diagnostic value of gadolinium-enhanced dynamic MR imaging with histopathologic correlation[J]. Radiology, 2003, 226(2): 345-354. |
| 30 | CHOI Y J, LEE I S, SONG Y S, et al. Diagnostic performance of diffusion-weighted (DWI) and dynamic contrast-enhanced (DCE) MRI for the differentiation of benign from malignant soft-tissue tumors[J]. J Magn Reson Imaging, 2019, 50(3): 798-809. |
| 31 | HAYAKAWA K, MATSUMOTO S, AE K, et al. Definitive surgery of primary lesion should be prioritized over preoperative chemotherapy to treat high-grade osteosarcoma in patients aged 41‒65 years[J]. J Orthop Traumatol, 2020, 21(1): 13. |
| 32 | CAO Z Y, ZHANG Y L, XU Q, et al. The role of chemotherapy in the survival benefits of patients aged older than 40 years with osteosarcoma[J]. Technol Cancer Res Treat, 2021, 20: 15330338211066195. |
| 33 | GUO Z X, QIN X Y, MU R H, et al. Amide proton transfer could provide more accurate lesion characterization in the transition zone of the prostate[J]. J Magn Reson Imaging, 2022, 56(5): 1311-1319. |
| 34 | GAO Y T, ZHOU H, LIU G G, et al. Tumor microenvironment: lactic acid promotes tumor development[J]. J Immunol Res, 2022, 2022: 3119375. |
| 35 | TOGAO O, YOSHIURA T, KEUPP J, et al. Amide proton transfer imaging of adult diffuse gliomas: correlation with histopathological grades[J]. Neuro Oncol, 2014, 16(3): 441-448. |
| 36 | MENG N, WANG X J, SUN J, et al. Comparative study of amide proton transfer-weighted imaging and intravoxel incoherent motion imaging in breast cancer diagnosis and evaluation[J]. J Magn Reson Imaging, 2020, 52(4): 1175-1186. |
| 37 | KOIKE H, MORIKAWA M, ISHIMARU H, et al. Amide proton transfer-chemical exchange saturation transfer imaging of intracranial brain tumors and tumor-like lesions: our experience and a review[J]. Diagnostics (Basel), 2023, 13(5): 914. |
| 38 | YANG L, WANG L, TAN Y C, et al. Amide Proton Transfer-weighted MRI combined with serum prostate-specific antigen levels for differentiating malignant prostate lesions from benign prostate lesions: a retrospective cohort study[J]. Cancer Imaging, 2023, 23(1): 3. |
| 39 | JIA G, ABAZA R, WILLIAMS J D, et al. Amide proton transfer MR imaging of prostate cancer: a preliminary study[J]. J Magn Reson Imaging, 2011, 33(3): 647-654. |
| 40 | ZHANG H W, LIU X L, ZHANG H B, et al. Differentiation of meningiomas and gliomas by amide proton transfer imaging: a preliminary study of brain tumour infiltration[J]. Front Oncol, 2022, 12: 886968. |
| 41 | 李莹, 程敬亮, 任翠萍, 等. 3D氨基质子转移加权成像联合弥散加权成像鉴别良、恶性骨与软组织肿瘤[J]. 中国医学影像技术, 2024, 40(10): 1572-1576. |
| LI Y,CHENG J L, REN C P, et al. 3D amide proton transfer weighted imaging combined with diffusion weighted imaging for differentiating benign and malignant bone and soft tissue tumors[J]. Chinese Journal of Medical Imaging Technology, 2024, 40(10): 1572-1576. | |
| 42 | LI Y, LIN L J, ZHANG Y, et al. Preliminary exploration of amide proton transfer weighted imaging in differentiation between benign and malignant bone tumors[J]. Front Oncol, 2024, 14: 1402628. |
| 43 | 刘记存, 崔建岭, 李石玲, 等. 表观扩散系数值鉴别良恶性骨肿瘤及肿瘤样病变的价值[J]. 中华放射学杂志, 2009, 43(6): 567-570. |
| LIU J C, CUI J L, LI S L, et al. The role of apparent diffusion coefficient in the differentiation between benign and malignant bone tumors[J]. Chinese Journal of Radiology, 2009, 43(6): 567-570. | |
| 44 | HAYASHIDA Y, HIRAI T, YAKUSHIJI T, et al. Evaluation of diffusion-weighted imaging for the differential diagnosis of poorly contrast-enhanced and T2-prolonged bone masses: initial experience[J]. J Magn Reson Imaging, 2006, 23(3): 377-382. |
| 45 | WANG T T, WU X R, CUI Y F, et al. Role of apparent diffusion coefficients with diffusion-weighted magnetic resonance imaging in differentiating between benign and malignant bone tumors[J]. World J Surg Oncol, 2014, 12: 365. |
| 46 | 王绍武, 孙美玉, 张丽娜, 等. 骨肿瘤的MR灌注和扩散加权成像研究[J]. 国际医学放射学杂志, 2008, 31(1): 6-10. |
| WANG S W, SUN M Y, ZHANG L N, et al. MR perfusion and diffusion imaging in diagnosing benign and malignant bone tumors[J]. International Journal of Medical Radiology, 2008, 31(1): 6-10. | |
| 47 | HISATOMI M, ASAUMI J I, YANAGI Y, et al. Diagnostic value of dynamic contrast-enhanced MRI in the salivary gland tumors[J]. Oral Oncol, 2007, 43(9): 940-947. |
| 48 | ZHOU J Y, ZAISS M, KNUTSSON L, et al. Review and consensus recommendations on clinical APT-weighted imaging approaches at 3T: application to brain tumors[J]. Magn Reson Med, 2022, 88(2): 546-574. |
| 49 | GUO H, LIU J, HU J J, et al. Diagnostic performance of gliomas grading and IDH status decoding A comparison between 3D amide proton transfer APT and four diffusion-weighted MRI models[J]. J Magn Reson Imaging, 2022, 56(6): 1834-1844. |
| [1] | 江怡, 黄晨浩, 李祉良, 吴珺玮, 赵任, 张弢. 1例KRAS突变的结直肠癌患者术前接受化疗联合免疫治疗的效果报道[J]. 上海交通大学学报(医学版), 2025, 45(9): 1256-1260. |
| [2] | 吴其蓁, 刘启明, 柴烨子, 陶政宇, 王依楠, 郭欣宁, 姜萌, 卜军. 机器学习预测乳腺癌新辅助治疗后炎症代谢状态改变的模型评价[J]. 上海交通大学学报(医学版), 2024, 44(9): 1169-1181. |
| [3] | 吴兵, 李小敏, 柳思宇, 赵露露, 武文, 郝永强, 艾松涛. 改良3D打印病理切片盒在骨肿瘤病理拼接中的应用初探[J]. 上海交通大学学报(医学版), 2023, 43(2): 180-187. |
| [4] | 邢正文, 吴滢, 王雪莉, 王庆煜, 王文婷, 李治, 张彬, 金晶. 儿童CIC重排肉瘤的临床病理特征[J]. 上海交通大学学报(医学版), 2022, 42(8): 1151-1157. |
| [5] | 陆艳青, 周兴, 李姣, 彭建平, 王传东, 张晓玲. 抗肿瘤药物依托泊苷促进间充质干细胞成骨分化的研究[J]. 上海交通大学学报(医学版), 2021, 41(7): 849-857. |
| [6] | 张珠晟, 刘琦, 鲍其远, 沈宇辉, 张伟滨, 万荣. 累及髋臼的原发良性与交界性骨肿瘤的术式选择与预后评估[J]. 上海交通大学学报(医学版), 2021, 41(11): 1470-1477. |
| [7] | 曲扬 1, 2,艾松涛 2,武文 1,王磊 1,李小敏 2,姜闻博 3,郝永强 1,戴尅戎 1. 3D打印个体化导板在骨肿瘤经皮穿刺活检中的初步应用[J]. 上海交通大学学报(医学版), 2018, 38(9): 1053-. |
| [8] | 何方舟 张伟滨 沈宇辉 . 定制型限制性全肘关节假体置换8例报告[J]. 上海交通大学学报(医学版), 2016, 36(8): 1205-. |
| [9] | 管雯斌,许恪淳,许艳春,等. 儿童横纹肌肉瘤的病理学研究[J]. 上海交通大学学报(医学版), 2014, 34(1): 70-. |
| [10] | 冯振中, 陈嘉薇, 赵 艳, 等. 骨外黏液样软骨肉瘤的临床病理学特征[J]. , 2009, 29(9): 1129-. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||