
上海交通大学学报(医学版) ›› 2023, Vol. 43 ›› Issue (7): 923-930.doi: 10.3969/j.issn.1674-8115.2023.07.015
收稿日期:2022-10-18
接受日期:2023-06-20
出版日期:2023-07-28
发布日期:2023-07-28
通讯作者:
董 平,电子信箱:dongping1050@163.com。作者简介:马 奔(1998—),男,硕士生;电子信箱:jsxzmaben@163.com。
基金资助:
MA Ben( ), ZHAO Cheng, SHU Yijun, DONG Ping(
), ZHAO Cheng, SHU Yijun, DONG Ping( )
)
Received:2022-10-18
Accepted:2023-06-20
Online:2023-07-28
Published:2023-07-28
Contact:
DONG Ping, E-mail: dongping1050@163.com.Supported by:摘要:
胃肠道间质瘤(gastrointestinal stromal tumor,GIST)是胃肠道最常见的间叶源性肿瘤,其生物学特征复杂,危险度不等,且不同危险度患者的治疗方法和预后差异较大,因此早期诊断及危险度评估对于该病的精准治疗至关重要。近年来,CT影像组学作为一种新兴的影像学技术,可以将传统的CT图像特征转变为大量数据,从而反映GIST的内在异质性,甚至与其基因表达特征相关联。该文回顾了CT影像组学在机器学习的助力下应用于GIST诊断、预测的研究进展。目前的CT影像组学不仅可用于GIST与其他胃部疾病的鉴别诊断,并且为GIST的危险度评估提供了新的方式,甚至可以根据CT影像图像进行病理分析及基因诊断,进而对其一线治疗效果及远期预后进行预测。目前CT影像组学通过与临床信息结合构建的多种预测模型在不同临床问题的具体实践中得到了良好的验证,展现了广阔的应用前景。但是在具体的临床应用过程中,样本数据采集及处理方式的不同、机器学习算法选择的差异、二维或三维图像的选择等,都影响到CT影像组学的具体效能,因此统一、规范的影像组学应用规则还有待建立。
中图分类号:
马奔, 赵成, 束翌俊, 董平. CT影像组学在胃肠道间质瘤中的应用进展[J]. 上海交通大学学报(医学版), 2023, 43(7): 923-930.
MA Ben, ZHAO Cheng, SHU Yijun, DONG Ping. Application progress of CT radiomics in gastrointestinal stromal tumor[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2023, 43(7): 923-930.
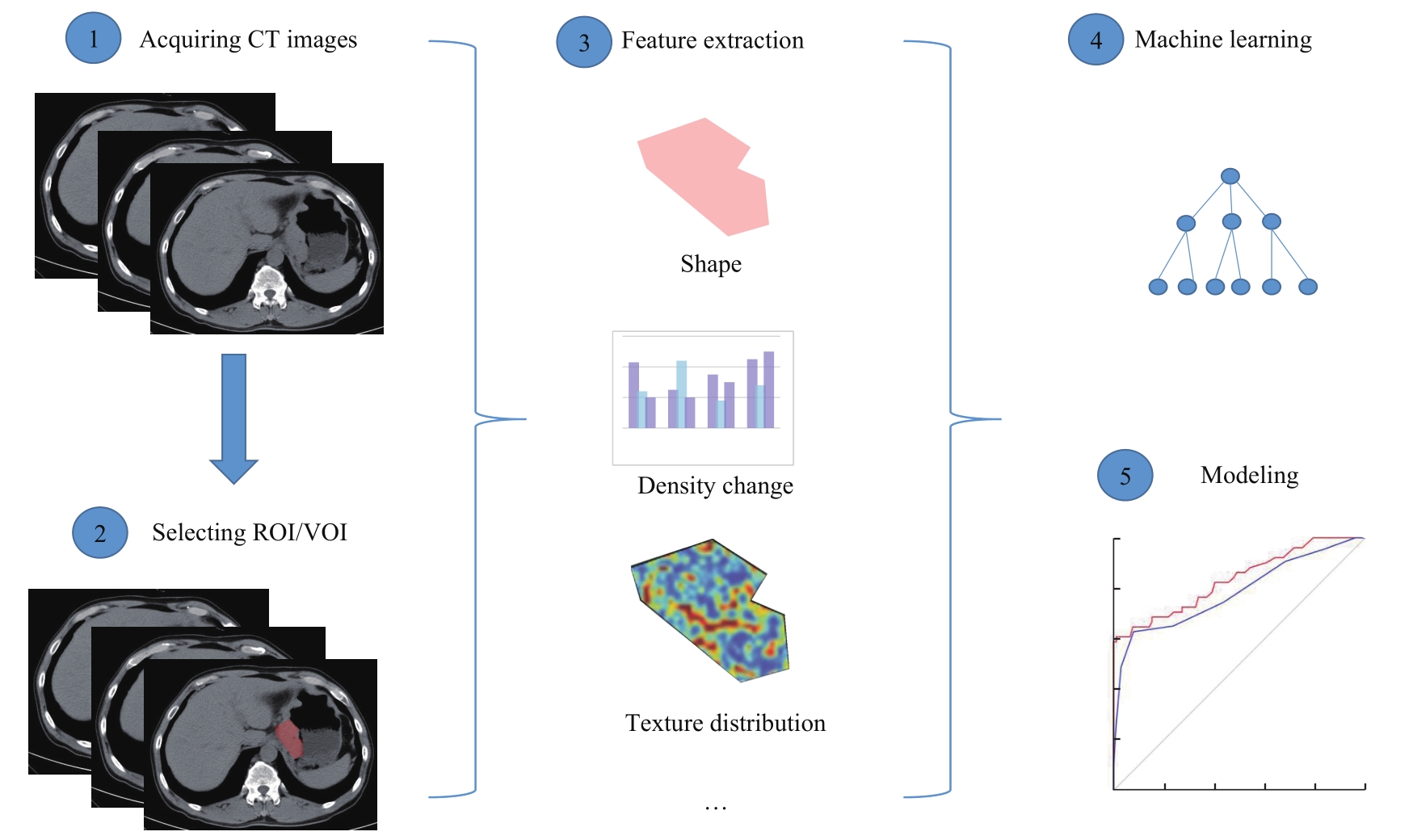
图1 CT影像组学模式的基本流程Note: The basic flow of CT radiomics mode consists of ① acquiring CT images, ② selecting ROI/VOI, ③ extracting features such as shape, density change, and texture distribution, ④ machine learning process using different classifiers such as Logistic regression, support vector machine, and random forest, and⑤ making different models such as radiomics model, radiomics and clinical data models, and radiomics nomogram.
Fig 1 Basic flow of CT radiomics mode
| Disease | Group | Sample size/n | Result | Reference |
|---|---|---|---|---|
| GIST/gastric adenocarcinoma/gastric lymphoma | Turkey | 26/125/12 | GIST vs gastric lymphoma: Sensitivity=98%, Specificity=75% GIST vs gastric adenocarcinoma: Sensitivity=91%, Specificity=77% | [ |
| GIST/gastric cancer | China | 40/60 | Subjective CT signs model: AUC=0.806 (0.696‒0.917), Accuracy=75% Radiomic signature model: AUC=0.886 (0.809‒0.963), Accuracy=81% Combined model: AUC=0.903 (0.831‒0.975), Accuracy=86% | [ |
| GIST/gastric adenocarcinoma/gastric lymphoma | Austria | Arterial phase: 15/31/5 Venous phase: 17/23/8 | Arterial phase misclassification rate: Gastric adenocarcinoma vs gastric lymphoma=3.1% GIST vs gastric lymphoma=0 Venous phase misclassification rate: Gastric adenocarcinoma vs gastric lymphoma=9.7% GIST vs gastric lymphoma=8.0% GIST vs gastric adenocarcinoma=10.0% | [ |
表1 CT影像组学应用于GIST与胃癌、胃淋巴瘤鉴别诊断的研究
Tab 1 Studies on differential diagnosis of GIST from gastric cancer and gastric lymphoma by CT radiomics
| Disease | Group | Sample size/n | Result | Reference |
|---|---|---|---|---|
| GIST/gastric adenocarcinoma/gastric lymphoma | Turkey | 26/125/12 | GIST vs gastric lymphoma: Sensitivity=98%, Specificity=75% GIST vs gastric adenocarcinoma: Sensitivity=91%, Specificity=77% | [ |
| GIST/gastric cancer | China | 40/60 | Subjective CT signs model: AUC=0.806 (0.696‒0.917), Accuracy=75% Radiomic signature model: AUC=0.886 (0.809‒0.963), Accuracy=81% Combined model: AUC=0.903 (0.831‒0.975), Accuracy=86% | [ |
| GIST/gastric adenocarcinoma/gastric lymphoma | Austria | Arterial phase: 15/31/5 Venous phase: 17/23/8 | Arterial phase misclassification rate: Gastric adenocarcinoma vs gastric lymphoma=3.1% GIST vs gastric lymphoma=0 Venous phase misclassification rate: Gastric adenocarcinoma vs gastric lymphoma=9.7% GIST vs gastric lymphoma=8.0% GIST vs gastric adenocarcinoma=10.0% | [ |
| Group | Sample size/n | Cutoff value of Ki-67/% | Result | Reference |
|---|---|---|---|---|
| China | 339 | 10 | Radiomic signature AUC: Training cohort: 0.787 (95%CI 0.632‒0.801) Internal validation cohort: 0.765 (95%CI 0.683‒0.847) External validation cohort: 0.754 (95%CI 0.666‒0.842) Radiomic nomogram AUC: Training cohort: 0.801 (95%CI 0.726‒0.876) Internal validation cohort: 0.828 (95%CI 0.681‒0.974) External validation cohort: 0.784 (95%CI 0.701‒0.868) | [ |
| China | 344 | 8 | Generated radiomic model AUC: Training cohort: 0.835 (95%CI 0.761‒0.908) External validation cohort: 0.784 (95%CI 0.691‒0.874) | [ |
| Japan | 64 | 5 | Fractal dimension: Sensitivity=66.7%, Specificity=69.8% | [ |
表2 CT影像组学对GIST免疫组化分析的研究
Tab 2 Studies on immunohistochemical analysis of GIST by CT radiomics
| Group | Sample size/n | Cutoff value of Ki-67/% | Result | Reference |
|---|---|---|---|---|
| China | 339 | 10 | Radiomic signature AUC: Training cohort: 0.787 (95%CI 0.632‒0.801) Internal validation cohort: 0.765 (95%CI 0.683‒0.847) External validation cohort: 0.754 (95%CI 0.666‒0.842) Radiomic nomogram AUC: Training cohort: 0.801 (95%CI 0.726‒0.876) Internal validation cohort: 0.828 (95%CI 0.681‒0.974) External validation cohort: 0.784 (95%CI 0.701‒0.868) | [ |
| China | 344 | 8 | Generated radiomic model AUC: Training cohort: 0.835 (95%CI 0.761‒0.908) External validation cohort: 0.784 (95%CI 0.691‒0.874) | [ |
| Japan | 64 | 5 | Fractal dimension: Sensitivity=66.7%, Specificity=69.8% | [ |
| 1 | JEMAL A, BRAY F, CENTER M M, et al. Global cancer statistics[J]. CA Cancer J Clin, 2011, 61(2): 69-90. |
| 2 | LEE I S, PARK Y S, LEE J H, et al. Pathologic discordance of differentiation between endoscopic biopsy and postoperative specimen in mucosal gastric adenocarcinomas[J]. Ann Surg Oncol, 2013, 20(13): 4231-4237. |
| 3 | JOENSUU H. Risk stratification of patients diagnosed with gastrointestinal stromal tumor[J]. Hum Pathol, 2008, 39(10): 1411-1419. |
| 4 | JOENSUU H, HOHENBERGER P, CORLESS C L. Gastrointestinal stromal tumour[J]. Lancet, 2013, 382(9896): 973-983. |
| 5 | DEMETRI G D, VON MEHREN M, BLANKE C D, et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors[J]. N Engl J Med, 2002, 347(7): 472-480. |
| 6 | VERWEIJ J, CASALI P G, ZALCBERG J, et al. Progression-free survival in gastrointestinal stromal tumours with high-dose imatinib: randomised trial[J]. Lancet, 2004, 364(9440): 1127-1134. |
| 7 | MIETTINEN M, SOBIN L H, LASOTA J. Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1 765 cases with long-term follow-up[J]. Am J Surg Pathol, 2005, 29(1): 52-68. |
| 8 | GILLIES R J, KINAHAN P E, HRICAK H. Radiomics: images are more than pictures, they are data[J]. Radiology, 2016, 278(2): 563-577. |
| 9 | YIP S S F, AERTS H J W L. Applications and limitations of radiomics[J]. Phys Med Biol, 2016, 61(13): R150-R166. |
| 10 | ZHANG L J, KANG L Q, LI G C, et al. Computed tomography-based radiomics model for discriminating the risk stratification of gastrointestinal stromal tumors[J]. Radiol Med, 2020, 125(5): 465-473. |
| 11 | LAMBIN P, RIOS-VELAZQUEZ E, LEIJENAAR R, et al. Radiomics: extracting more information from medical images using advanced feature analysis[J]. Eur J Cancer, 2012, 48(4): 441-446. |
| 12 | CHEN T, LIU S Q, LI Y, et al. Developed and validated a prognostic nomogram for recurrence-free survival after complete surgical resection of local primary gastrointestinal stromal tumors based on deep learning[J]. EBioMedicine, 2019, 39: 272-279. |
| 13 | SUN Z Q, HU S D, LI J, et al. Radiomics study for differentiating gastric cancer from gastric stromal tumor based on contrast-enhanced CT images[J]. J Xray Sci Technol, 2019, 27(6): 1021-1031. |
| 14 | ZHENG J, XIA Y, XU A Q, et al. Combined model based on enhanced CT texture features in liver metastasis prediction of high-risk gastrointestinal stromal tumors[J]. Abdom Radiol (NY), 2022, 47(1): 85-93. |
| 15 | STARMANS M P A, TIMBERGEN M J M, VOS M, et al. Differential diagnosis and molecular stratification of gastrointestinal stromal tumors on CT images using a radiomics approach[J]. J Digit Imaging, 2022, 35(2): 127-136. |
| 16 | 李定杰, 吴慧, 刘如, 等. 基于诊断CT影像组学对食管癌放疗疗效早期评估[J]. 中华放射肿瘤学杂志, 2019, 28(10): 731-734. |
| LI D J, WU H, LIU R, et al. Early evaluation of radiotherapy effect of esophageal cancer based on diagnostic CT imaging histology[J]. Chinese Journal of Radiation Oncology, 2019, 28(10): 731-734. | |
| 17 | 李华秀, 李振辉, 李鹍, 等. CT影像组学预测局部进展期直肠癌新辅助治疗的效果[J]. 中国医学影像学杂志, 2020, 28(1): 44-50. |
| LI H X, LI Z H, LI K, et al. Efficacy of CT radiomics in predicting neoadjuvant therapy of locally advanced rectal cancer[J]. Chinese Journal of Medical Imaging, 2020, 28(1): 44-50. | |
| 18 | ZHOU Y, HE L, HUANG Y Q, et al. CT-based radiomics signature: a potential biomarker for preoperative prediction of early recurrence in hepatocellular carcinoma[J]. Abdom Radiol, 2017, 42(6): 1695-1704. |
| 19 | GAO X J, MA T T, CUI J L, et al. A radiomics-based model for prediction of lymph node metastasis in gastric cancer[J]. Eur J Radiol, 2020, 129: 109069. |
| 20 | BA-SSALAMAH A, MUIN D, SCHERNTHANER R, et al. Texture-based classification of different gastric tumors at contrast-enhanced CT[J]. Eur J Radiol, 2013, 82(10): e537-e543. |
| 21 | ZEYDANLI T, KILIC H K. Performance of quantitative CT texture analysis in differentiation of gastric tumors[J]. Jpn J Radiol, 2022, 40(1): 56-65. |
| 22 | CASTELLANO G, BONILHA L, LI L M, et al. Texture analysis of medical images[J]. Clin Radiol, 2004, 59(12): 1061-1069. |
| 23 | BASHIR U, SIDDIQUE M M, MCLEAN E, et al. Imaging heterogeneity in lung cancer: techniques, applications, and challenges[J]. AJR Am J Roentgenol, 2016, 207(3): 534-543. |
| 24 | YE H, XIN H, ZHENG Q, et al. Prognostic role of the primary tumour site in patients with operable small intestine and gastrointestinal stromal tumours: a large population-based analysis[J]. Oncotarget, 2017, 9(8): 8147-8154. |
| 25 | MIETTINEN M, LASOTA J. Gastrointestinal stromal tumors: review on morphology, molecular pathology, prognosis, and differential diagnosis[J]. Arch Pathol Lab Med, 2006, 130(10): 1466-1478. |
| 26 | MIETTINEN M, LASOTA J. Gastrointestinal stromal tumors: pathology and prognosis at different sites[J]. Semin Diagn Pathol, 2006, 23(2): 70-83. |
| 27 | FLETCHER C D M, BRIDGE J A, HOGENDOORN P C W, et al. WHO classification of tumours of soft tissue and bone[M]. 4th ed. Lyon: IARC Press, 2013. |
| 28 | 中国临床肿瘤学会胃肠间质瘤专家委员会. 中国胃肠间质瘤诊断治疗共识(2017年版)[J]. 肿瘤综合治疗电子杂志, 2018, 4(1): 31-43. |
| Expert Committee on Gastrointestinal Stromal Tumor, Chinese Society of Clinical Oncology. Chinese consensus on diagnosis and treatment of gastrointestinal stromal tumor (2017 edition)[J]. Journal of Multidisciplinary Cancer Management (Electronic Version), 2018, 4(1): 31-43. | |
| 29 | CHOI I Y, YEOM S K, CHA J, et al. Feasibility of using computed tomography texture analysis parameters as imaging biomarkers for predicting risk grade of gastrointestinal stromal tumors: comparison with visual inspection[J]. Abdom Radiol (NY), 2019, 44(7): 2346-2356. |
| 30 | SONG Y C, LI J, WANG H X, et al. Radiomics nomogram based on contrast-enhanced CT to predict the malignant potential of gastrointestinal stromal tumor: a two-center study[J]. Acad Radiol, 2022, 29(6): 806-816. |
| 31 | DEMETRI G D, VON MEHREN M, ANTONESCU C R, et al. NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors[J]. J Natl Compr Canc Netw, 2010, 8(Suppl 2): S1-S44. |
| 32 | RUTKOWSKI P, PRZYBYŁ J, ZDZIENICKI M. Extended adjuvant therapy with imatinib in patients with gastrointestinal stromal tumors[J]. Mol Diagn Ther, 2013, 17(1): 9-19. |
| 33 | ECKARDT A J, ADLER A, GOMES E M, et al. Endosonographic large-bore biopsy of gastric subepithelial tumors: a prospective multicenter study[J]. Eur J Gastroenterol Hepatol, 2012, 24(10): 1135-1144. |
| 34 | ZHAO Y L, FENG M B, WANG M H, et al. CT radiomics for the preoperative prediction of Ki67 index in gastrointestinal stromal tumors: a multi-center study[J]. Front Oncol, 2021, 11: 689136. |
| 35 | WANG C, LI H L, JIAERKEN Y, et al. Building CT radiomics-based models for preoperatively predicting malignant potential and mitotic count of gastrointestinal stromal tumors[J]. Transl Oncol, 2019, 12(9): 1229-1236. |
| 36 | BASILIO-DE-OLIVEIRA R P, PANNAIN V L N. Prognostic angiogenic markers (endoglin, VEGF, CD31) and tumor cell proliferation (Ki67) for gastrointestinal stromal tumors[J]. World J Gastroenterol, 2015, 21(22): 6924-6930. |
| 37 | ZHANG Q W, GAO Y J, ZHANG R Y, et al. Personalized CT-based radiomics nomogram preoperative predicting Ki-67 expression in gastrointestinal stromal tumors: a multicenter development and validation cohort[J]. Clin Transl Med, 2020, 9(1): 12. |
| 38 | KURATA Y, HAYANO K, OHIRA G, et al. Fractal analysis of contrast-enhanced CT images for preoperative prediction of malignant potential of gastrointestinal stromal tumor[J]. Abdom Radiol, 2018, 43(10): 2659-2664. |
| 39 | 朱从波, 廖国庆, 赵丁民. Ki-67对胃肠道间质瘤预后的评估价值[J]. 临床与病理杂志, 2018, 38(8): 1632-1639. |
| ZHU C B, LIAO G Q, ZHAO D M. Prognostic value of Ki-67 index in gastrointestinal stromal tumor[J]. Journal of Clinical and Pathological Research, 2018, 38(8): 1632-1639. | |
| 40 | XU F, MA X H, WANG Y C, et al. CT texture analysis can be a potential tool to differentiate gastrointestinal stromal tumors without KIT exon 11 mutation[J]. Eur J Radiol, 2018, 107: 90-97. |
| 41 | LIU X J, YIN Y, WANG X Z, et al. Gastrointestinal stromal tumors: associations between contrast-enhanced CT images and KIT exon 11 gene mutation[J]. Ann Transl Med, 2021, 9(19): 1496. |
| 42 | PALATRESI D, FEDELI F, DANTI G, et al. Correlation of CT radiomic features for GISTs with pathological classification and molecular subtypes: preliminary and monocentric experience[J]. Radiol Med, 2022, 127(2): 117-128. |
| 43 | CHEN T, NING Z Y, XU L L, et al. Radiomics nomogram for predicting the malignant potential of gastrointestinal stromal tumours preoperatively[J]. Eur Radiol, 2019, 29(3): 1074-1082. |
| 44 | CHU H R, PANG P P, HE J, et al. Value of radiomics model based on enhanced computed tomography in risk grade prediction of gastrointestinal stromal tumors[J]. Sci Rep, 2021, 11(1): 12009. |
| 45 | WANG M H, FENG Z, ZHOU L X, et al. Computed-tomography-based radiomics model for predicting the malignant potential of gastrointestinal stromal tumors preoperatively: a multi-classifier and multicenter study[J]. Front Oncol, 2021, 11: 582847. |
| 46 | REN C Y, WANG S P, ZHANG S J. Development and validation of a nomogram based on CT images and 3D texture analysis for preoperative prediction of the malignant potential in gastrointestinal stromal tumors[J]. Cancer Imaging, 2020, 20(1): 5. |
| 47 | ZHANG Q W, ZHOU X X, ZHANG R Y, et al. Comparison of malignancy-prediction efficiency between contrast and non-contract CT-based radiomics features in gastrointestinal stromal tumors: a multicenter study[J]. Clin Transl Med, 2020, 10(3): e291. |
| 48 | COLLEWET G, STRZELECKI M, MARIETTE F. Influence of MRI acquisition protocols and image intensity normalization methods on texture classification[J]. Magn Reson Imaging, 2004, 22(1): 81-91. |
| 49 | LUBNER M G, STABO N, LUBNER S J, et al. CT textural analysis of hepatic metastatic colorectal cancer: pre-treatment tumor heterogeneity correlates with pathology and clinical outcomes[J]. Abdom Imaging, 2015, 40(7): 2331-2337. |
| 50 | HUANG Y Q, LIANG C H, HE L, et al. Development and validation of a radiomics nomogram for preoperative prediction of lymph node metastasis in colorectal cancer[J]. J Clin Oncol, 2016, 34(18): 2157-2164. |
| [1] | 胥瀚文, 陈墨馨, 梁小乙, 舒琴, 聂琬钦, 杨雪峰, 沈慜瑄, 黎晓静, 曹禹, 李琳. 基于面部照片的眼病智能诊断研究进展[J]. 上海交通大学学报(医学版), 2025, 45(9): 1249-1255. |
| [2] | 黄昕, 刘家辉, 叶敬文, 钱文莉, 许万星, 王琳. 基于机器学习的小细胞肺癌代谢分子诊断模型的建立和临床应用[J]. 上海交通大学学报(医学版), 2025, 45(8): 1009-1016. |
| [3] | 梁书源, 叶宝英, 程蔚蔚. 超声指标和血液指标预测胎儿生长受限的研究现状[J]. 上海交通大学学报(医学版), 2025, 45(8): 1059-1065. |
| [4] | 宋毅杰, 陈天真, 钟娜, 赵敏. 生成式人工智能在精神医学中的应用与挑战[J]. 上海交通大学学报(医学版), 2025, 45(10): 1271-1278. |
| [5] | 禹志远, 董海平, 高楠, 马柯. 背根神经节吗啡耐受核心基因筛选与机制研究:加权基因共表达网络分析和机器学习的转录组学整合策略[J]. 上海交通大学学报(医学版), 2025, 45(10): 1308-1319. |
| [6] | 吴其蓁, 刘启明, 柴烨子, 陶政宇, 王依楠, 郭欣宁, 姜萌, 卜军. 机器学习预测乳腺癌新辅助治疗后炎症代谢状态改变的模型评价[J]. 上海交通大学学报(医学版), 2024, 44(9): 1169-1181. |
| [7] | 许万星, 王琳, 郭巧梅, 王薛庆, 娄加陶. 多模态肺结节诊断模型的临床验证及应用价值探索[J]. 上海交通大学学报(医学版), 2024, 44(8): 1030-1036. |
| [8] | 李昕欣, 边懿泽, 赵航, 姜萌. 人工智能辅助测量心肌应变的研究进展[J]. 上海交通大学学报(医学版), 2024, 44(6): 773-778. |
| [9] | 周天凡, 邵飞雪, 万盛, 周晨晨, 周思锦, 花晓琳. 基于人工智能模型量化视网膜血管特征参数预测子痫前期的可行性研究[J]. 上海交通大学学报(医学版), 2024, 44(5): 552-559. |
| [10] | 郭勇麟, 陈墨馨, 刘哲源, 李奕霏, 王子琦, 舒琴, 李琳. 基于人工智能技术的斜视诊疗进展[J]. 上海交通大学学报(医学版), 2024, 44(3): 393-398. |
| [11] | 卫雪敏, 高成金. ASPECT评分在急性缺血性脑卒中临床应用中的研究进展[J]. 上海交通大学学报(医学版), 2022, 42(7): 919-924. |
| [12] | 王晓峰, 周璐, 姚乐宇, 何凡, 彭海霞, 杨大明, 黄晓霖. 深度卷积神经网络模型辅助下结直肠息肉检测系统对初级医师结直肠小息肉检出率的影响[J]. 上海交通大学学报(医学版), 2022, 42(2): 205-210. |
| [13] | 李欣, 范青. 机器学习在抑郁症患者面部特征研究中的应用进展[J]. 上海交通大学学报(医学版), 2022, 42(1): 124-129. |
| [14] | 刘想, 谢辉辉, 许玉峰, 陶晓峰, 柳林, 吴迪嘉, 王霄英. 人工智能在胸部创伤肋骨骨折CT诊断中应用的初步研究[J]. 上海交通大学学报(医学版), 2021, 41(7): 920-925. |
| [15] | 李小敏, 曲扬, 张少霆, 赵亮, 刘畅, 谢帅宁, 戴尅戎, 艾松涛. 人工智能技术在骨肌系统影像学方面的应用[J]. 上海交通大学学报(医学版), 2021, 41(2): 262-266. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||