
上海交通大学学报(医学版) ›› 2022, Vol. 42 ›› Issue (6): 702-708.doi: 10.3969/j.issn.1674-8115.2022.06.002
收稿日期:2022-03-02
接受日期:2022-06-12
出版日期:2022-06-28
发布日期:2022-08-19
通讯作者:
杨 驰,电子信箱:yangchi63@hotmail.com。作者简介:何冬梅(1972—)女,教授,主任医师;电子信箱:lucyhe119@163.com。
基金资助:Received:2022-03-02
Accepted:2022-06-12
Online:2022-06-28
Published:2022-08-19
Contact:
YANG Chi, E-mail: yangchi63@hotmail.com.Supported by:摘要:
颞下颌关节强直以张口受限为特点,生长期发生会导致面部畸形和阻塞性睡眠呼吸暂停等,严重影响患者的外形和下颌功能,是临床难治疾病。随着新技术的出现和经验的不断积累,颞下颌关节强直的诊治取得很大进展。该文在文献回顾的基础上重点介绍上海交通大学医学院附属第九人民医院颞下颌关节中心的手术经验并提出诊疗方案,供临床医师参考。颞下颌关节强直的影像学诊断中,CT冠状重建是分类的主要依据,根据骨球内侧是否存在残余髁突结构及其大小可以分为4种类型,此外对颞下颌关节强直伴发的颌骨畸形、咬合关系紊乱和呼吸道结构紊乱可以进一步分类。颞下颌关节强直的手术治疗包括外侧间隙成形术和关节重建术。当骨球内侧存在髁突结构且其内外径≥正常髁突内外径的1/2时,选择外侧间隙成形术,以保留髁突及关节盘结构;其他类型选择关节重建术,包括自体骨移植、人工关节重建、牵引成骨术等。对合并的颌骨畸形可以同期或二期进行正颌外科手术。自体脂肪移植可以显著减少颞下颌关节强直的复发。
中图分类号:
何冬梅, 杨驰. 颞下颌关节强直的诊治方案:基于上海交通大学医学院附属第九人民医院颞下颌关节中心的经验[J]. 上海交通大学学报(医学版), 2022, 42(6): 702-708.
HE Dongmei, YANG Chi. Diagnosis and treatment protocol of temporomandibular joint (TMJ) ankylosis: experience from the TMJ Center of Shanghai Ninth People's Hospital, Shanghai Jiao Tong University School of Medicine[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2022, 42(6): 702-708.
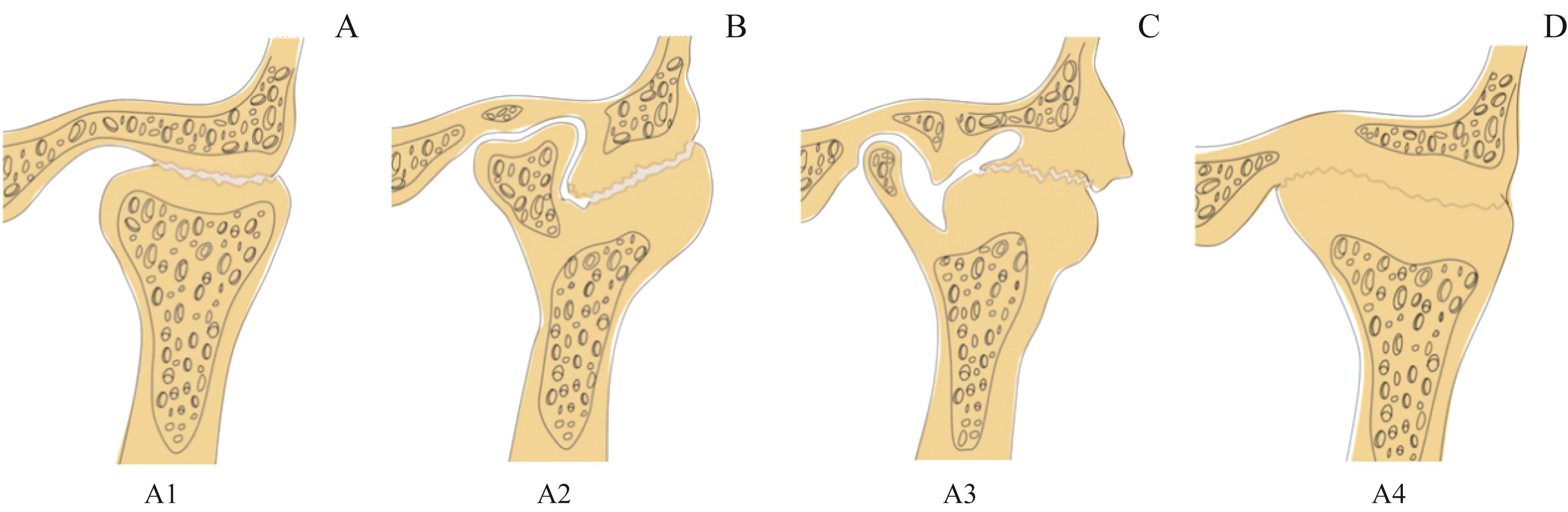
图1 颞下颌关节强直的分类Note:A. Fibrous ankylosis. B. Fibrous or bony fusion on the lateral side of the joint, while the residual condyle fragment is greater than or equal to 1/2 of the condylar head on the medial side. C. The residual condylar fragment is smaller than 1/2 of the condylar head. D. Complete bony fusion of the joint.
Fig 1 Classification of temporomandibular joint ankylosis
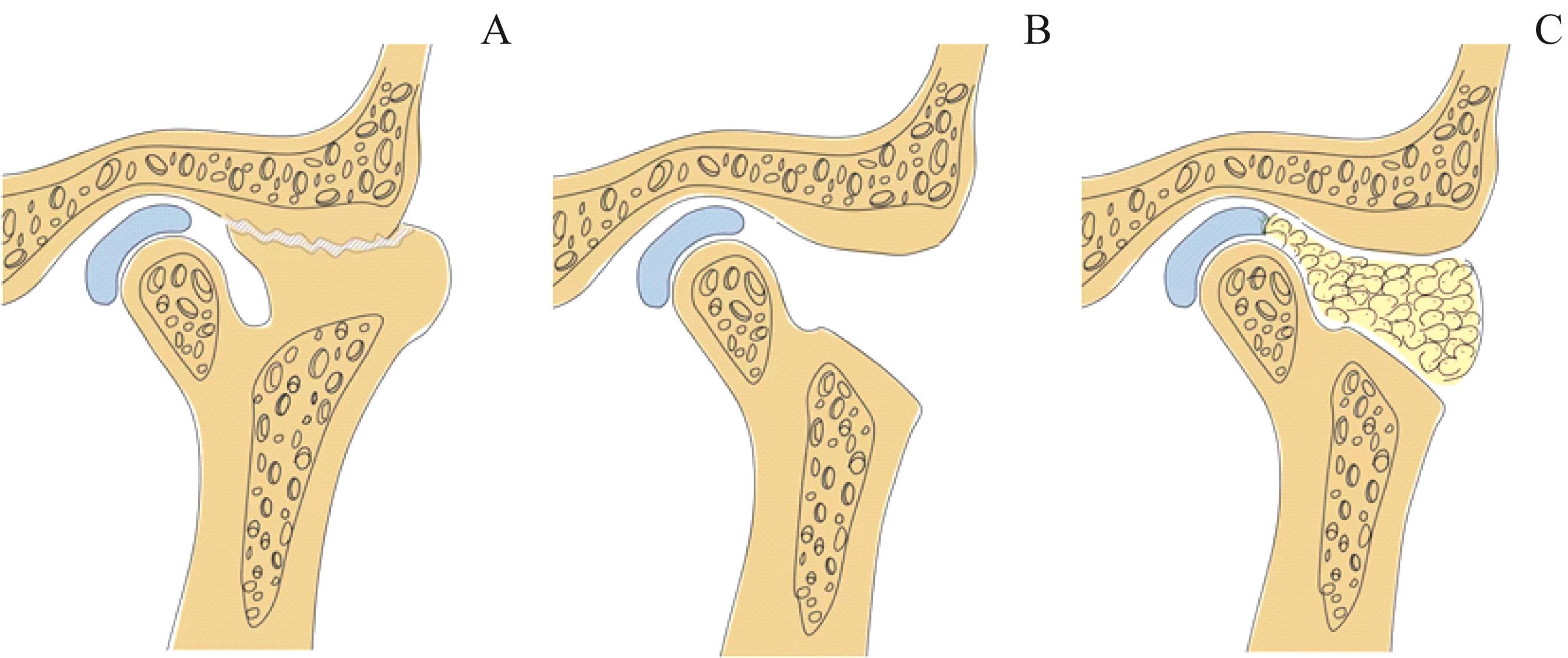
图2 外侧间隙成形术手术过程示意图Note:A. Resection of the lateral bony fusion. B. Restoring the medially displaced condyle and disc. C. Fat packing in the lateral osteotomy space.
Fig 2 Schematic diagram of lateral gap arthroplasty operation process
| 1 | SAWHNEY C P. Bony ankylosis of the temporomandibular joint[J]. Plast Reconstr Surg, 1986, 77(1): 29. |
| 2 | NITZAN D W, BAR-ZIV J, SHTEYER A. Surgical management of temporomandibular joint ankylosis type Ⅲ by retaining the displaced condyle and disc[J]. J Oral Maxillofac Surg, 1998, 56(10): 1133-1138;discussion1139. |
| 3 | EL-HAKIM I E, METWALLI S A. Imaging of temporomandibular joint ankylosis. A new radiographic classification[J]. Dentomaxillofac Radiol, 2002, 31(1): 19-23. |
| 4 | HE D M, YANG C, CHEN M J, et al. Traumatic temporomandibular joint ankylosis: our classification and treatment experience[J]. J Oral Maxillofac Surg, 2011, 69(6): 1600-1607. |
| 5 | 杨驰. 颞下颌关节强直// 邱蔚六. 邱蔚六口腔颌面外科学[M]. 上海: 上海科学技术出版社, 2008: 869-871. |
| YANG C. Temporomandibular joint ankylosis// QIU W L. Oral and maxillofacial surgery[M]. Shanghai: Shanghai Scientific & Technical Publishers, 2008: 869-871. | |
| 6 | XIA L, AN J G, HE Y, et al. Association between the clinical features of and types of temporomandibular joint ankylosis based on a modified classification system[J]. Sci Rep, 2019, 9(1): 10493. |
| 7 | BI R, JIANG N, YIN Q, et al. A new clinical classification and treatment strategies for temporomandibular joint ankylosis[J]. Int J Oral Maxillofac Surg, 2020, 49(11): 1449-1458. |
| 8 | BABU L, JAIN M K, RAMESH C, et al. Is aggressive gap arthroplasty essential in the management of temporomandibular joint ankylosis? A prospective clinical study of 15 cases[J]. Br J Oral Maxillofac Surg, 2013, 51(6): 473-478. |
| 9 | MEHROTRA D, PRADHAN R, MOHAMMAD S, et al. Random control trial of dermis-fat graft and interposition of temporalis fascia in the management of temporomandibular ankylosis in children[J]. Br J Oral Maxillofac Surg, 2008, 46(7): 521-526. |
| 10 | THANGAVELU A, SANTHOSH KUMAR K, VAIDHYANATHAN A, et al. Versatility of full thickness skin-subcutaneous fat grafts as interpositional material in the management of temporomandibular joint ankylosis[J]. Int J Oral Maxillofac Surg, 2011, 40(1): 50-56. |
| 11 | LONG X, LI X D, CHENG Y, et al. Preservation of disc for treatment of traumatic temporomandibular joint ankylosis[J]. J Oral Maxillofac Surg, 2005, 63(7): 897-902. |
| 12 | HE D M, YANG C, CHEN M J, et al. Surgical treatment of traumatic temporomandibular joint ankylosis with medially displaced residual condyle: surgical methods and long-term results[J]. J Oral Maxillofac Surg, 2011, 69(9): 2412-2418. |
| 13 | SINGH V, BHAGOL A, DHINGRA R, et al. Management of temporomandibular joint ankylosis type Ⅲ: lateral arthroplasty as a treatment of choice[J]. Int J Oral Maxillofac Surg, 2014, 43(4): 460-464. |
| 14 | YANG X J, LU C, DONG M J, et al. Evaluation of the condyle remodeling after lateral arthroplasty in growing children with temporomandibular joint ankylosis[J]. Sci Rep, 2017, 7(1): 9922. |
| 15 | XIA L, HE Y, AN J, et al. Condyle-preserved arthroplasty versus costochondral grafting in paediatric temporomandibular joint ankylosis: a retrospective investigation[J]. Int J Oral Maxillofac Surg, 2019, 48(4): 526-533. |
| 16 | GUI H J, WU J Y, SHEN S G F, et al. Navigation-guided lateral gap arthroplasty as the treatment of temporomandibular joint ankylosis[J]. J Oral Maxillofac Surg, 2014, 72(1): 128-138. |
| 17 | LU C, HE D M, YANG C, et al. Use of computer-assisted templates for placement of osteotomies in lateral gap arthroplasty[J]. J Oral Maxillofac Surg, 2015, 73(1): 30-38. |
| 18 | MOVAHED R, MERCURI L G. Management of temporomandibular joint ankylosis[J]. Oral Maxillofac Surg Clin North Am, 2015, 27(1): 27-35. |
| 19 | GILLIES H D. Plastic surgery of the face[J]. Lancet, 1920, 196(5056): 194. |
| 20 | HUANG I Y, LAI S T, SHEN Y H, et al. Interpositional arthroplasty using autogenous costal cartilage graft for temporomandibular joint ankylosis in adults[J]. Int J Oral Maxillofac Surg, 2007, 36(10): 909-915. |
| 21 | KHADKA A, HU J. Autogenous grafts for condylar reconstruction in treatment of TMJ ankylosis: current concepts and considerations for the future[J]. Int J Oral Maxillofac Surg, 2012, 41(1): 94-102. |
| 22 | LU C, HUANG D, HE D M, et al. Digital occlusal splint for condylar reconstruction in children with temporomandibular joint ankylosis[J]. J Oral Maxillofac Surg, 2014, 72(8): 1585-1593. |
| 23 | ZHAO J Y, HE D M, YANG C, et al. 3-D computed tomography measurement of mandibular growth after costochondral grafting in growing children with temporomandibular joint ankylosis and jaw deformity[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2017, 124(4): 333-338. |
| 24 | 洪民, 李永海, 黄继贤. 喙突移植治疗颞颌关节强直[J]. 解放军医学院学报, 1980, 1(1): 54-58. |
| HONG M, LI Y H, HUANG J X. Coronoid process graft in treatment of temporomandibular ankylosisJ]. Acad J Chin PLA Med School, 1980, 1(1): 54-58. | |
| 25 | ZHU S S, HU J, LI J H, et al. Free grafting of autogenous coronoid process for condylar reconstruction in patients with temporomandibular joint ankylosis[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2008, 106(5): 662-667. |
| 26 | ZHANG W N, GU B, HU J, et al. Retrospective comparison of autogenous cosotochondral graft and coronoid process graft in the management of unilateral ankylosis of the temporomandibular joint in adults[J]. Br J Oral Maxillofac Surg, 2014, 52(10): 928-933. |
| 27 | CHEN S, HE Y, AN J G, et al. Recurrence-related factors of temporomandibular joint ankylosis: a 10-year experience[J]. J Oral Maxillofac Surg, 2019, 77(12): 2512-2521. |
| 28 | HUANG D, LU C, YAO Z D, et al. A comparison of the effect between coronoid process graft and costochondral graft in the reconstruction of temporomandibular joint[J]. J Craniofac Surg, 2016, 27(2): e197-e200. |
| 29 | LIU Y M, LI J H, HU J, et al. Autogenous coronoid process pedicled on temporal muscle grafts for reconstruction of the mandible condylar in patients with temporomandibular joint ankylosis[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2010, 109(2): 203-210. |
| 30 | SNYDER C C, LEVINE G A, DINGMAN D L. Trial of a sternoclavicular whole joint graft as a substitute for the temporomandibular joint[J]. Plast Reconstr Surg, 1971, 48(5): 447-452. |
| 31 | SINGH V, DHINGRA R, BHAGOL A. Prospective analysis of temporomandibular joint reconstruction in ankylosis with sternoclavicular graft and buccal fat pad lining[J]. J Oral Maxillofac Surg, 2012, 70(4): 997-1006. |
| 32 | RAO J K D, DAR N, SHARMA A, et al. Evaluation of the sternoclavicular graft for the reconstruction of temporomandibular joint after gap arthroplasty[J]. Ann Maxillofac Surg, 2017, 7(2): 194-201. |
| 33 | THIRUNAVUKKARASU R, BALASUBRAMANIAM S, BALASUBRAMANIAN S, et al. Sternoclavicular joint graft in temporomandibular joint reconstruction for ankylosis[J]. Ann Maxillofac Surg, 2018, 8(2): 292-298. |
| 34 | SETH S, GUPTA H, KUMAR D, et al. Sternoclavicular graft versus costochondral graft in reconstruction of ankylosed temporomandibular joint[J]. J Maxillofac Oral Surg, 2019, 18(4): 559-566. |
| 35 | LIU Y, KHADKA A, LI J, et al. Sliding reconstruction of the condyle using posterior border of mandibular ramus in patients with temporomandibular joint ankylosis[J]. Int J Oral Maxillofac Surg, 2011, 40(11): 1238-1245. |
| 36 | MERCURI L G, WOLFORD L M, SANDERS B, et al. Long-term follow-up of the CAD/CAM patient fitted total temporomandibular joint reconstruction system[J]. J Oral Maxillofac Surg, 2002, 60(12): 1440-1448. |
| 37 | MERCURI L G, ALI F A, WOOLSON R. Outcomes of total alloplastic replacement with periarticular autogenous fat grafting for management of reankylosis of the temporomandibular joint[J]. J Oral Maxillofac Surg, 2008, 66(9): 1794-1803. |
| 38 | WOLFORD L, MOVAHED R, TESCHKE M, et al. Temporomandibular joint ankylosis can be successfully treated with TMJ concepts patient-fitted total joint prosthesis and autogenous fat grafts[J]. J Oral Maxillofac Surg, 2016, 74(6): 1215-1227. |
| 39 | ZOU L X, ZHANG L Z, HE D M, et al. Clinical and radiologic follow-up of zimmer biomet stock total temporomandibular joint replacement after surgical modifications[J]. J Oral Maxillofac Surg, 2018, 76(12): 2518-2524. |
| 40 | HU Y H, ZHANG L Z, HE D M, et al. Simultaneous treatment of temporomandibular joint ankylosis with severe mandibular deficiency by standard TMJ prosthesis[J]. Sci Rep, 2017, 7: 45271. |
| 41 | BAI G, HE D M, YANG C, et al. Application of digital templates to guide total alloplastic joint replacement surgery with biomet standard replacement system[J]. J Oral Maxillofac Surg, 2014, 72(12): 2440-2452. |
| 42 | LI H, HE D M, XIE Q Y, et al. Do simultaneous mandibular advancement and temporomandibular joint prosthesis impact the upper airway in TMJ ankylosis patients? [J]. Ann Transl Med, 2021, 9(22): 1638. |
| 43 | STUCKI-MCCORMICK S U, FOX R M, MIZRAHI R D. Reconstruction of a neocondyle using transport distraction osteogenesis[J]. Semin Orthod, 1999, 5(1): 59-63. |
| 44 | XIAO E, ZHANG Y, AN J, et al. Long-term evaluation of the stability of reconstructed condyles by transport distraction osteogenesis[J]. Int J Oral Maxillofac Surg, 2012, 41(12): 1490-1494. |
| 45 | HASSAN S A E H, MOHAMED F I. Distraction osteogenesis in the management of mandibular hypoplasia secondary to temporomandibular joint ankylosis. Long term follow up[J]. J Craniomaxillofac Surg, 2019, 47(10): 1510-1520. |
| 46 | YU H B, SHEN G F, ZHANG S L, et al. Gap arthroplasty combined with distraction osteogenesis in the treatment of unilateral ankylosis of the temporomandibular joint and micrognathia[J]. Br J Oral Maxillofac Surg, 2009, 47(3): 200-204. |
| 47 | ZHANG C, LI Y F, YE B, et al. Application of bidirectional distraction osteogenesis for the treatment of mandibular micriognathia caused by temporomandibular joint ankylosis[J]. J Craniofac Surg, 2017, 28(6): 1502-1507. |
| 48 | SRIVASTAVA D, LUTHRA P, MISHRA S, et al. Technique of dual distraction for correction of unilateral temporomandibular joint ankylosis with facial asymmetry: a case series[J]. J Oral Maxillofac Surg, 2019, 77(12): 2555.e1-2555.e12. |
| 49 | ZHANG X H, CHEN M J, WU Y, et al. Management of temporomandibular joint ankylosis associated with mandibular asymmetry in infancy[J]. J Craniofac Surg, 2011, 22(4): 1316-1319. |
| 50 | KAUR K, ROYCHOUDHURY A, BHUTIA O, et al. Evaluation of success of transport disc distraction osteogenesis and costochondral graft for ramus condyle unit reconstruction in pediatric temporomandibular joint ankylosis[J]. J Oral Maxillofac Surg, 2020, 78(6): 1018.e1-1018.e16. |
| 51 | MITTAL N, GOYAL M, SARDANA D, et al. Outcomes of surgical management of TMJ ankylosis: a systematic review and meta-analysis[J]. J Craniomaxillofac Surg, 2019, 47(7): 1120-1133. |
| 52 | AL-MORAISSI E A, EL-SHARKAWY T M, MOUNAIR R M, et al. A systematic review and meta-analysis of the clinical outcomes for various surgical modalities in the management of temporomandibular joint ankylosis[J]. Int J Oral Maxillofac Surg, 2015, 44(4): 470-482. |
| 53 | ZHU S S, WANG D Z, YIN Q D, et al. Treatment guidelines for temporomandibular joint ankylosis with secondary dentofacial deformities in adults[J]. J Craniomaxillofac Surg, 2013, 41(7): e117-e127. |
| 54 | JIANG Y M, HUANG Y J, YE B, et al. Management of temporomandibular joint ankylosis with dentofacial deformities in children[J]. J Craniofac Surg, 2018, 29(2): e150-e155. |
| 55 | GERBINO G, ZAVATTERO E, BERRONE S, et al. One stage treatment of temporomandibular joint complete bony ankylosis using total joint replacement[J]. J Craniomaxillofac Surg, 2016, 44(4): 487-492. |
| 56 | KABAN L B, PERROTT D H, FISHER K. A protocol for management of temporomandibular joint ankylosis[J]. J Oral Maxillofac Surg, 1990, 48(11): 1145-1151;discussion1152. |
| 57 | KABAN L B, BOUCHARD C, TROULIS M J. A protocol for management of temporomandibular joint ankylosis in children[J]. J Oral Maxillofac Surg, 2009, 67(9): 1966-1978. |
| 58 | DURR E D, TURLINGTON E G, FOOTE R L. Radiation treatment of heterotopic bone formation in the temporomandibular joint articulation[J]. Int J Radiat Oncol Biol Phys, 1993, 27(4): 863-869. |
| 59 | JENSEN A W, VIOZZI C F, FOOTE R L. Long-term results of radiation prophylaxis for heterotopic ossification in the temporomandibular joint[J]. J Oral Maxillofac Surg, 2010, 68(5): 1100-1105. |
| [1] | 李倩玉, 钱逸斐, 李松玲, 朱子俊, 覃雯莉, 刘艳丰, 邱必军. Zeste 12抑制基因在肝细胞癌中的功能及机制[J]. 上海交通大学学报(医学版), 2025, 45(9): 1138-1148. |
| [2] | 王静怡, 邓佳丽, 朱仪, 丁心怡, 郭嘉婧, 王中领. 新型pH响应性锰基纳米探针用于乳腺癌铁死亡及磁共振成像实验研究[J]. 上海交通大学学报(医学版), 2025, 45(9): 1183-1193. |
| [3] | 胥瀚文, 陈墨馨, 梁小乙, 舒琴, 聂琬钦, 杨雪峰, 沈慜瑄, 黎晓静, 曹禹, 李琳. 基于面部照片的眼病智能诊断研究进展[J]. 上海交通大学学报(医学版), 2025, 45(9): 1249-1255. |
| [4] | 江怡, 黄晨浩, 李祉良, 吴珺玮, 赵任, 张弢. 1例KRAS突变的结直肠癌患者术前接受化疗联合免疫治疗的效果报道[J]. 上海交通大学学报(医学版), 2025, 45(9): 1256-1260. |
| [5] | 黄昕, 刘家辉, 叶敬文, 钱文莉, 许万星, 王琳. 基于机器学习的小细胞肺癌代谢分子诊断模型的建立和临床应用[J]. 上海交通大学学报(医学版), 2025, 45(8): 1009-1016. |
| [6] | 何苏荟, 赵银龙, 张家毓. 端粒酶基因治疗对压力超负荷心力衰竭小鼠的影响[J]. 上海交通大学学报(医学版), 2025, 45(8): 949-956. |
| [7] | 张兴利, 田洁, 罗菁, 刘倩, 欧阳皖雁, 邱宏春, 王焰, 糜坚青. 剂量减低的来那度胺/美法仑/醋酸泼尼松方案治疗老年虚弱新诊断多发性骨髓瘤的效果分析[J]. 上海交通大学学报(医学版), 2025, 45(7): 815-822. |
| [8] | 林桐, 陶怡, 金诗炜, 孙淼, 糜坚青. 血浆置换联合经典化学治疗对多发性骨髓瘤患者肾功能的影响[J]. 上海交通大学学报(医学版), 2025, 45(7): 823-828. |
| [9] | 孟靖, 谢玉婷, 左佳鑫, 熊屏. 纳米工程化T细胞体系的构建及其对口腔鳞状细胞癌的体外治疗研究[J]. 上海交通大学学报(医学版), 2025, 45(7): 866-873. |
| [10] | 陈子旋, 刘敏. 肾细胞癌免疫细胞治疗的研究进展[J]. 上海交通大学学报(医学版), 2025, 45(7): 916-925. |
| [11] | 孙磊, 戴世锋, 陈裕华, 许新怡, 姜克乐, 李筱文, 李承靖, 吴婷婷. 颞下颌关节紊乱病患者关节盘与髁突距离的定量分析研究[J]. 上海交通大学学报(医学版), 2025, 45(6): 684-692. |
| [12] | 高欣洁, 刘艳, 王大威. 地中海贫血基因治疗研究进展及思考[J]. 上海交通大学学报(医学版), 2025, 45(5): 540-548. |
| [13] | 张钲佳, 李小敏, 周鑫, 马海荣, 艾松涛. 高阶磁共振功能成像评估骨与软组织肿瘤价值初探[J]. 上海交通大学学报(医学版), 2025, 45(5): 585-596. |
| [14] | 李文妙, 邢莉, 潘英瑜, 黄滢, 杨国访, 刘德达. 下颌第一磨牙根管直径和锥度的锥形束CT测量分析[J]. 上海交通大学学报(医学版), 2025, 45(5): 597-604. |
| [15] | 禹恺, 帅哲玮, 黄洪军, 罗艳. 小胶质细胞在中枢神经系统炎症性疾病中的作用和机制研究进展[J]. 上海交通大学学报(医学版), 2025, 45(5): 630-638. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||
