
上海交通大学学报(医学版) ›› 2022, Vol. 42 ›› Issue (9): 1275-1287.doi: 10.3969/j.issn.1674-8115.2022.09.014
收稿日期:2022-05-18
接受日期:2022-08-06
出版日期:2022-09-28
发布日期:2022-09-28
通讯作者:
段胜仲,电子信箱:duansz@shsmu.edu.cn。作者简介:李 露(1997—),女,硕士生;电子信箱:lilu123@sjtu.edu.com基金资助:
LI Lu( ), LI Yulin(
), LI Yulin( ), LIU Yan, DUAN Shengzhong(
), LIU Yan, DUAN Shengzhong( )
)
Received:2022-05-18
Accepted:2022-08-06
Online:2022-09-28
Published:2022-09-28
Contact:
DUAN Shengzhong, E-mail: duansz@shsmu.edu.cn.Supported by:摘要:
目的·研究牙周炎(periodontitis,PD)对主动脉弓缩窄(transverse aortic constriction,TAC)诱导的小鼠心肌肥厚的作用和机制。方法·将25只 C57BL/6J小鼠随机分为假手术(Sham)组、TAC组及TAC+PD组。用丝线结扎加涂抹龈下菌斑的方法诱导PD模型,并在PD模型建立后做TAC手术。在假手术或TAC手术后4周,用心脏超声评估心脏功能,然后处死小鼠并取材,其样本用于实时定量聚合酶链式反应(qRT-PCR)、免疫组织化学检测、免疫荧光检测、16S rRNA基因测序。结果·TAC+PD组小鼠的牙槽骨吸收和牙龈组织炎症相关基因的表达均高于Sham组和TAC组,表明在TAC小鼠中成功建立了PD模型。与TAC组相比,TAC+PD组小鼠的左心室射血分数(EF)、左心室缩短分数(FS)值都显著降低,表明PD加重TAC导致的心功能受损。与TAC组相比,TAC+PD组小鼠的心脏质量/体质量比率(HW/BW)和心脏质量/胫骨长度比率(HW/TL)升高、肺质量/体质量比率(LW/BW)升高、心肌细胞横截面积增大、心肌肥厚相关的基因表达水平也显著升高,表明PD加重TAC诱导的心肌肥厚和心力衰竭。与TAC组相比,TAC+PD组小鼠的心肌纤维化程度上升、纤维化相关基因上调、脾脏胫骨长度比率(SW/TL)上升、炎症相关基因上调,表明PD加重了TAC诱导心肌细胞的纤维化和炎症反应。16S rRNA基因测序结果表明,TAC+PD组小鼠的口腔结扎丝线中链球菌属(Streptococcus)和韦荣球菌属(Veillonella)的相对丰度显著高于TAC组;TAC+PD组小鼠的心脏中罗尔斯通菌属(Ralstonia)和嗜糖假单胞菌属(Pelomonas)的相对丰度显著高于TAC组;而且TAC+PD组小鼠的心脏中罗尔斯通菌属和嗜糖假单胞菌属的相对丰度显著高于其口腔结扎丝线。结论·PD能够加重TAC术后小鼠心脏功能损害、心肌肥厚和心肌纤维化,并在一定程度上加重心脏的炎症反应,其作用机制可能与罗尔斯通菌属、嗜糖假单胞菌属等口腔微生物相关。
中图分类号:
李露, 李雨霖, 柳燕, 段胜仲. 牙周炎加重主动脉弓缩窄诱导的小鼠心肌肥厚[J]. 上海交通大学学报(医学版), 2022, 42(9): 1275-1287.
LI Lu, LI Yulin, LIU Yan, DUAN Shengzhong. Periodontitis aggravates transverse aortic constriction-induced cardiac hypertrophy in mice[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2022, 42(9): 1275-1287.
| Gene | Forward primer | Reverse primer |
|---|---|---|
| Il-1β | GAAATGCCACCTTTTGACAGTG | TGGATGCTCTCATCAGGACAG |
| Il-17a | TTTAACTCCCTTGGCGCAAAA | CTTTCCCTCCGCATTGACAC |
| Il-6 | CTGCAAGAGACTTCCATCCAG | AGTGGTATAGACAGGTCTGTTGG |
| Il-18 | GACTCTTGCGTCAACTTCAAGG | CAGGCTGTCTTTTGTCAACGA |
| Ifn-γ | ATGAACGCTACACACTGCATC | CCATCCTTTTGCCAGTTCCTC |
| Ctgf | GGGCCTCTTCTGCGATTTC | ATCCAGGCAAGTGCATTGGTA |
| Col1a1 | CTGGCGGTTCAGGTCCAAT | TTCCAGGCAATCCACGAGC |
| Col3a1 | CTGTAACATGGAAACTGGGGAAA | CCATAGCTGAACTGAAAACCACC |
| Acta1 | CCCAAAGCTAACCGGGAGAAG | CCAGAATCCAACACGATGCC |
| Nppa | GCTTCCAGGCCATATTGGAG | GGGGGCATGACCTCATCTT |
| β-Mhc | CGGACCTTGGAAGACCAGAT | GACAGCTCCCCATTCTCTGT |
| Gapdh | AGGTCGGTGTGAACGGATTTG | TGTAGACCATGTAGTTGAGGTCA |
| β-actin | GGCTGTATTCCCCTCCATCG | CCAGTTGGTAACAATGCCATGT |
表1 qRT-PCR所用的引物序列(5′→3′)
Tab 1 A list of the primers used in the qRT-PCR (5′→3′)
| Gene | Forward primer | Reverse primer |
|---|---|---|
| Il-1β | GAAATGCCACCTTTTGACAGTG | TGGATGCTCTCATCAGGACAG |
| Il-17a | TTTAACTCCCTTGGCGCAAAA | CTTTCCCTCCGCATTGACAC |
| Il-6 | CTGCAAGAGACTTCCATCCAG | AGTGGTATAGACAGGTCTGTTGG |
| Il-18 | GACTCTTGCGTCAACTTCAAGG | CAGGCTGTCTTTTGTCAACGA |
| Ifn-γ | ATGAACGCTACACACTGCATC | CCATCCTTTTGCCAGTTCCTC |
| Ctgf | GGGCCTCTTCTGCGATTTC | ATCCAGGCAAGTGCATTGGTA |
| Col1a1 | CTGGCGGTTCAGGTCCAAT | TTCCAGGCAATCCACGAGC |
| Col3a1 | CTGTAACATGGAAACTGGGGAAA | CCATAGCTGAACTGAAAACCACC |
| Acta1 | CCCAAAGCTAACCGGGAGAAG | CCAGAATCCAACACGATGCC |
| Nppa | GCTTCCAGGCCATATTGGAG | GGGGGCATGACCTCATCTT |
| β-Mhc | CGGACCTTGGAAGACCAGAT | GACAGCTCCCCATTCTCTGT |
| Gapdh | AGGTCGGTGTGAACGGATTTG | TGTAGACCATGTAGTTGAGGTCA |
| β-actin | GGCTGTATTCCCCTCCATCG | CCAGTTGGTAACAATGCCATGT |

图1 TAC结合PD小鼠的牙周炎表型特征Note: A. Graphical illustration of experimental design. w—week. B/C. Representative methylene blue staining of mouse maxillae illustrating CEJ-ABC distance (B) and space between CEJ and ABC (C). D/E. Quantification of CEJ-ABC distance (D) and area between CEJ and ABC (E). F. qRT-PCR analysis of inflammatory genes in mouse gingiva.
Fig 1 Phenotypical characterization of periodontitis in mice with or without TAC
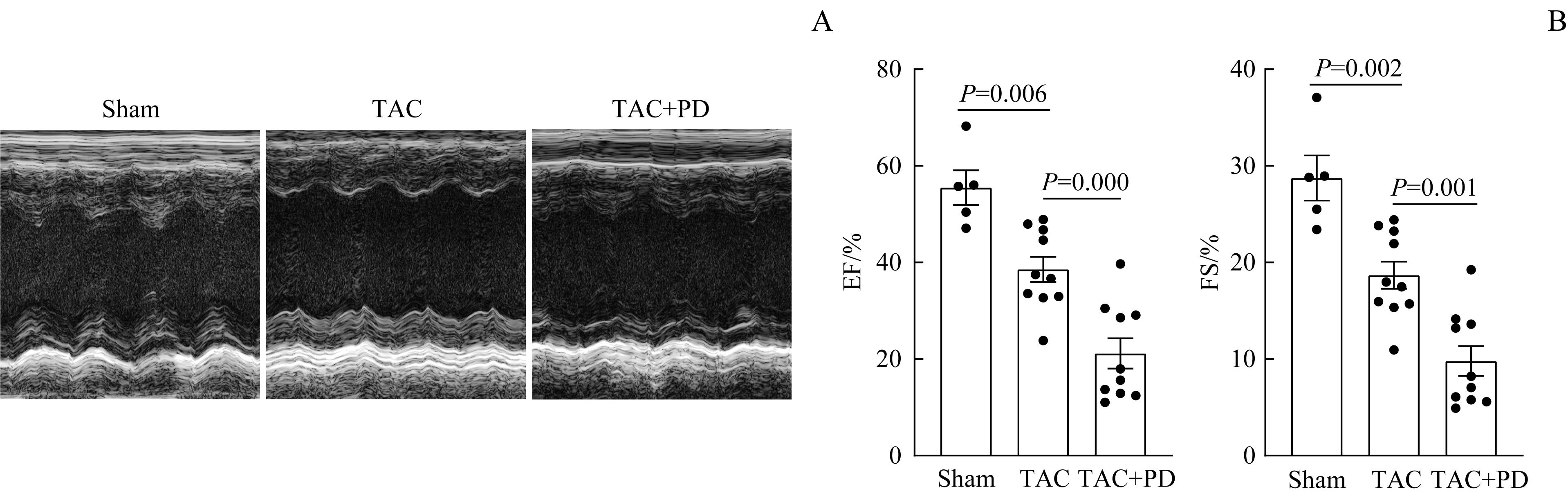
图2 PD加重TAC诱导的小鼠心脏功能障碍Note: A. Representative echocardiographic images of mice 4 weeks after sham or TAC operations. B. Quantification of left ventricle ejection fraction (EF) and left ventricle fractional shortening (FS) based on echocardiography.
Fig 2 PD exacerbating TAC-induced cardiac dysfunction in mice
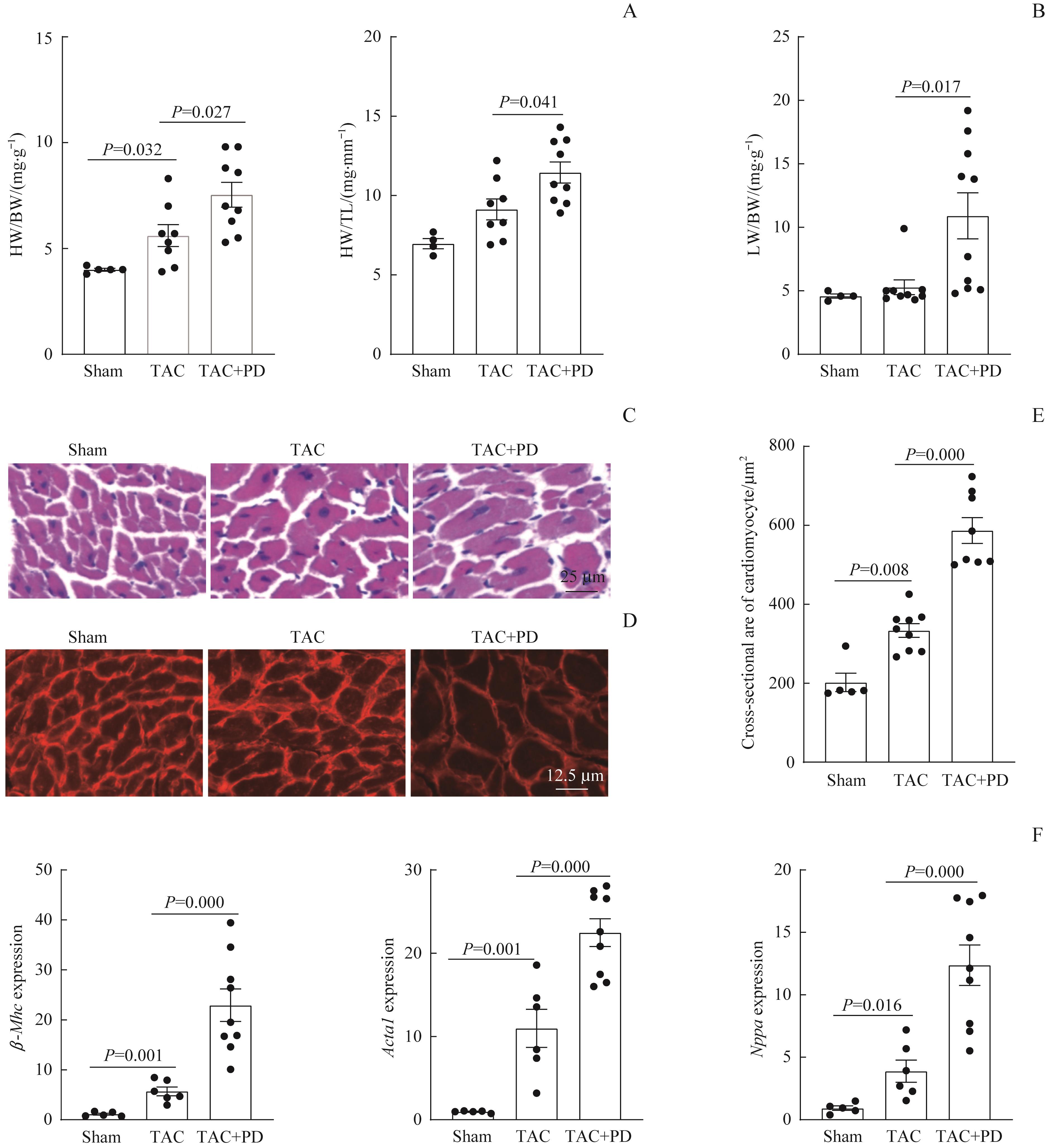
图3 PD加重TAC诱导的小鼠心肌肥厚Note: A. Heart weight to body weight ratio (HW/BW) and heart weight to tibia length ratio (HW/TL). B. Lung weight to body weight ratio (LW/BW). C/D. Representative images of H-E staining (C) and WGA staining (D) of cardiac cross-sections 4 weeks after sham or TAC operations. E. Quantification of cardiomyocyte size based on WGA staining. F. qRT-PCR analysis of hypertrophy-related genes in left ventricles 4 weeks after sham or TAC operations.
Fig 3 PD exacerbating TAC-induced cardiac hypertrophy in mice
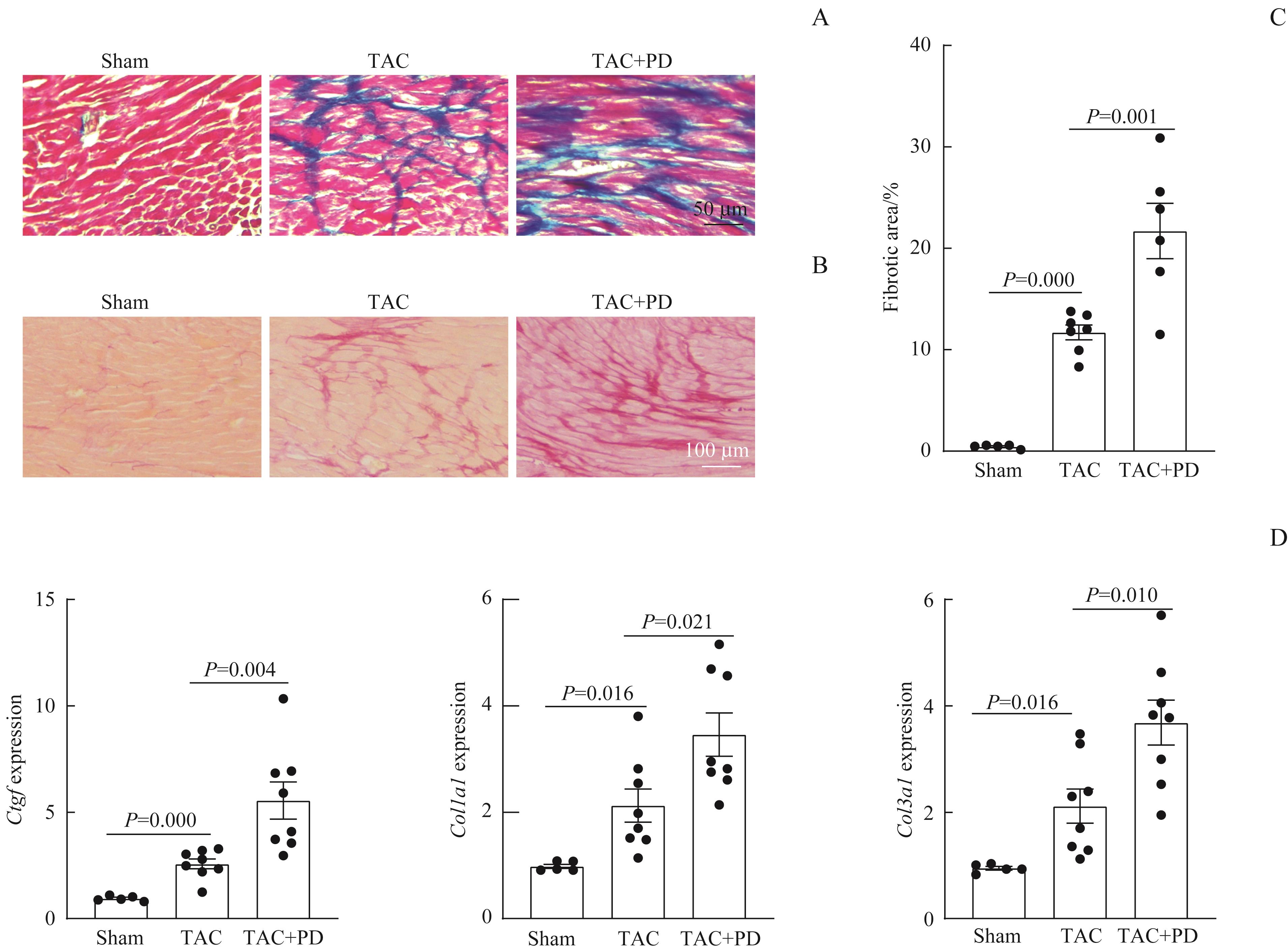
图4 PD加重TAC诱导的小鼠心肌纤维化Note: A/B. Representative images of Masson's trichrome staining (A) and sirius red staining (B) of cardiac cross-sections 4 weeks after sham or TAC operations. C. Quantification of myocardial fibrotic area based on sirius red staining. D. qRT-PCR analysis of fibrosis-related genes in left ventricles 4 weeks after sham or TAC operations.
Fig 4 PD aggravating TAC-induced cardiac fibrosis in mice
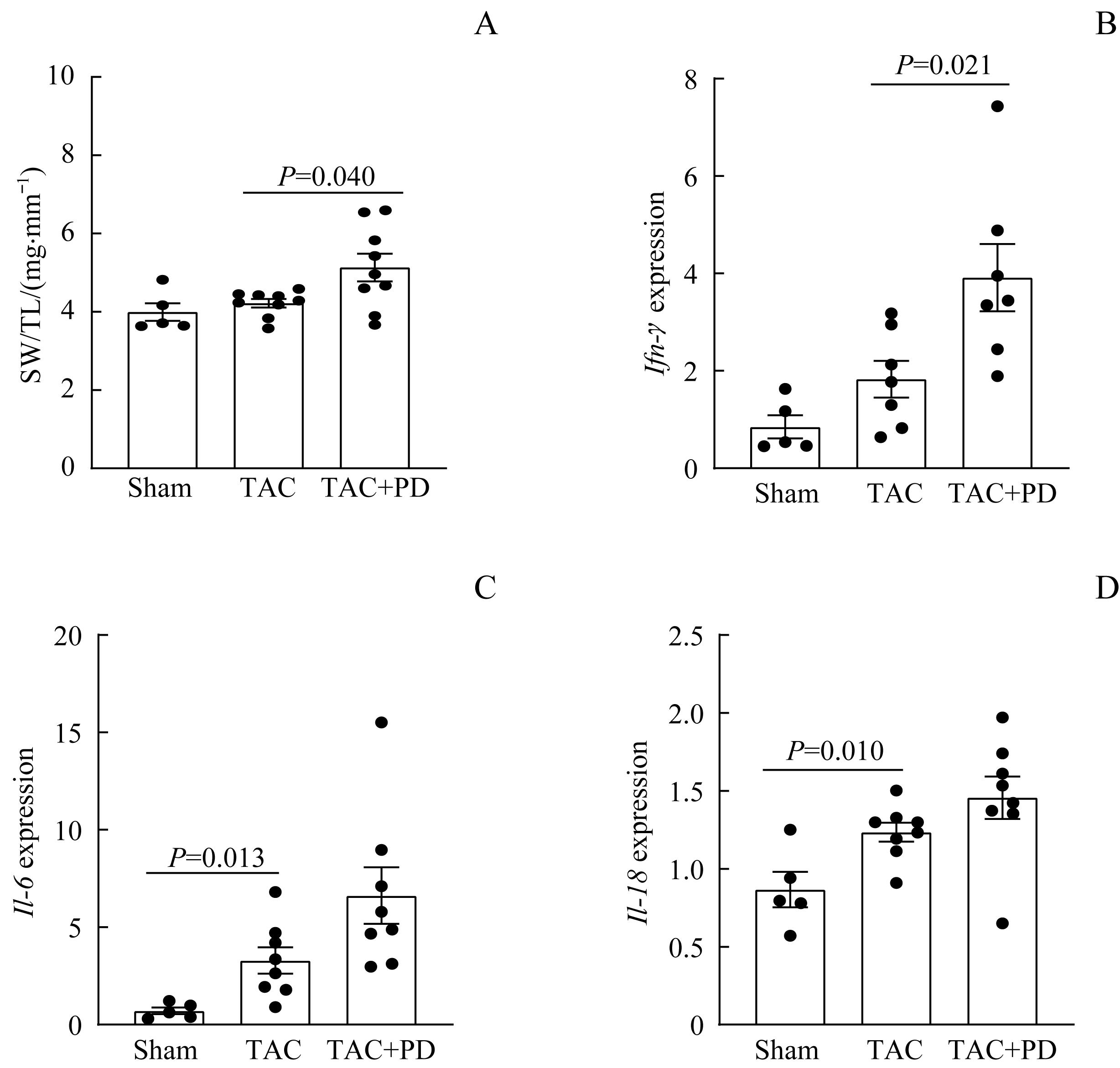
图5 PD加重TAC诱导的小鼠心脏炎症Note: A. Spleen weight to tibia length ratio (SW/TL) of mice 4 weeks after sham or TAC operations. B?D. qRT-PCR analysis of inflammatory genes Ifn-γ (B), Il-6 (C), and Il-18 (D) in left ventricles 4 weeks after sham or TAC operations.
Fig 5 PD aggravating TAC-induced cardiac inflammation
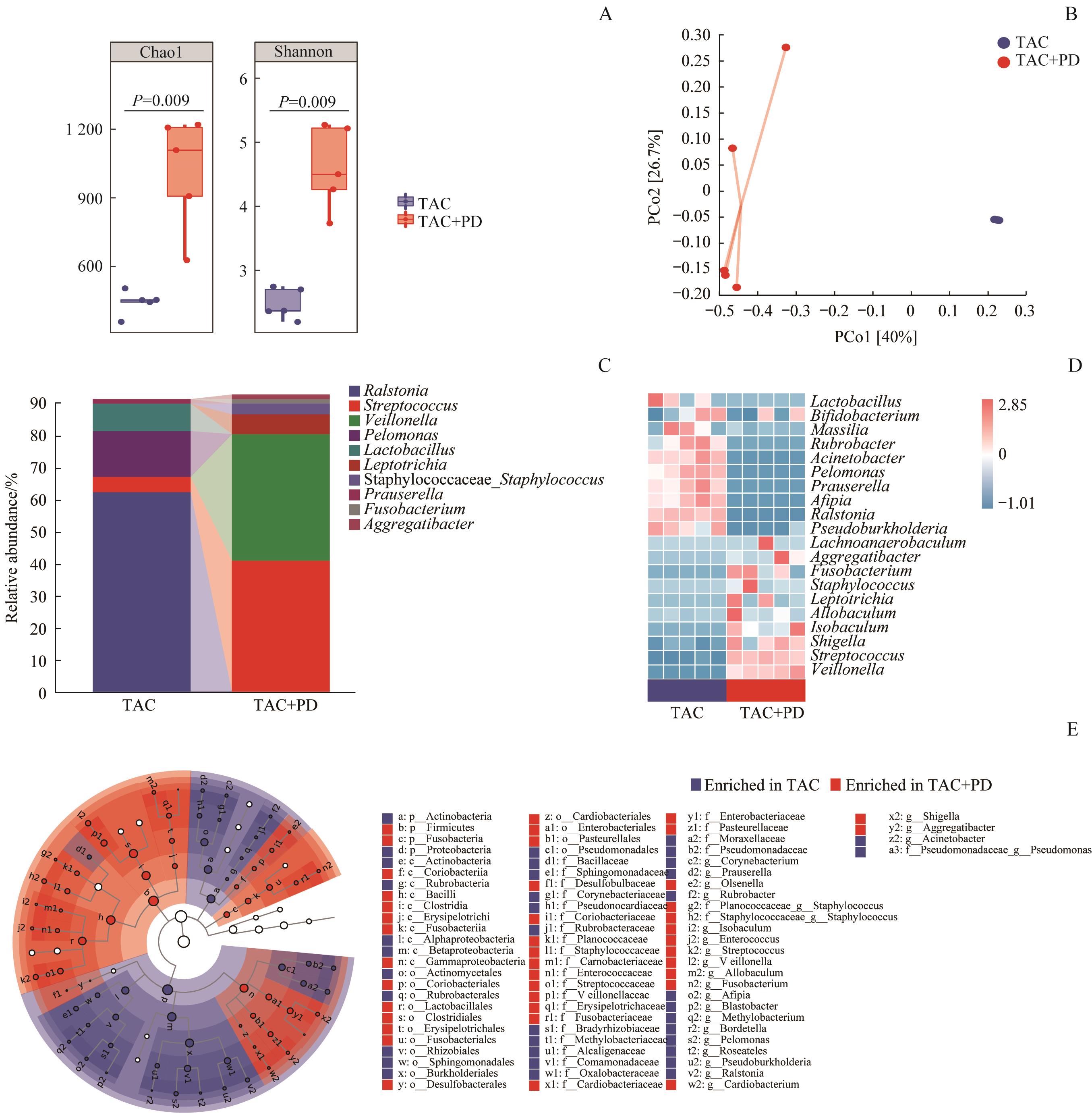
图6 PD改变TAC小鼠的口腔微生态Note: A. α-diversity of microbiota in oral ligatures assessed by Chao1 and Shannon indices. B. β-diversity of microbiota in oral ligatures analyzed by PCoA based on Bray-Curtis distance. C. Composition of microbiota in oral ligatures showing relative abundances of the 10 most abundant genera. D. Heatmap of relative abundances of the 20 most abundant genera in oral ligatures. E. Taxonomic cladogram of microbiota in oral ligatures using LEfSe (LDA=2). Oral microbiota was analyzed by using 16S rRNA gene sequencing.
Fig 6 PD altering oral microbiota in mice undergoing TAC
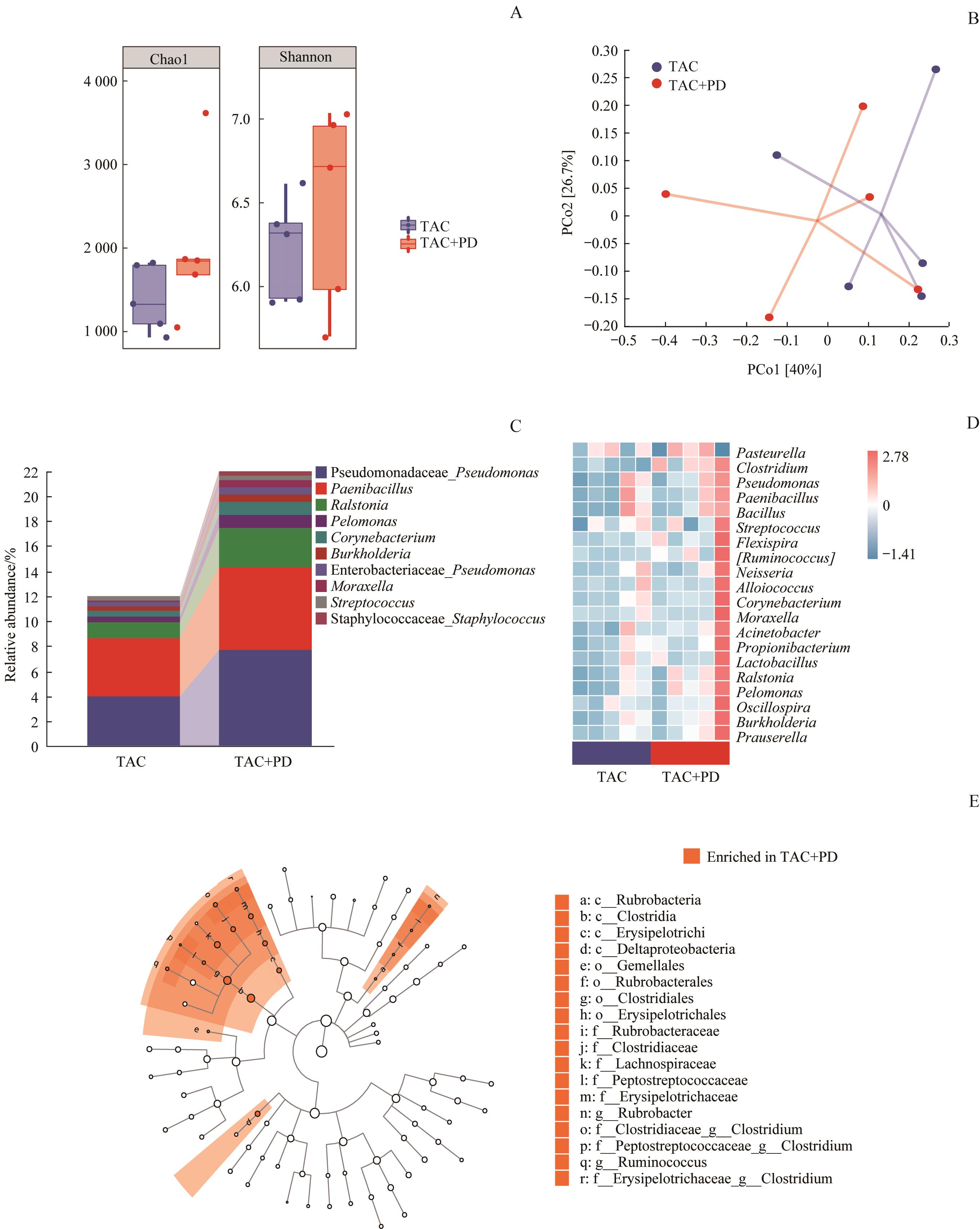
图7 PD改变TAC小鼠的心脏微生态Note: A. α-diversity of microbiota in hearts assessed by Chao1 and Shannon indices. B. β-diversity of microbiota in hearts analyzed by PCoA based on Bray-Curtis distance. C. Composition of microbiota in hearts showing relative abundances of the 10 most abundant genera. D. Heatmap of relative abundances of the 20 most abundant genera in hearts. E. Taxonomic cladogram of microbiota in hearts using LEfSe (LDA=2). Heart microbiota was analyzed by using 16S rRNA gene sequencing.
Fig 7 PD altering heart microbiota in mice undergoing TAC

图8 比较TAC结合PD小鼠的口腔微生态与心脏微生态Note: A. Venn diagram showing the overlapped and different genera between oral and heart microbiota. B. Comparison of microbial β-diversity between oral and heart microbiota using PCoA based on Bray-Curtis distance. C. Compositional difference between oral and heart microbiota at phylum level. D. Compositional difference between oral and heart microbiota at genus level. O—oral; H—heart. The numbers (1?5) denote individual mice. E. Taxonomic cladogram presentation of oral and heart microbiota based on LEfSe (LDA=2.72). Microbiota in oral ligatures and hearts was analyzed by using 16S rRNA gene sequencing.
Fig 8 Comparison of oral and heart microbiota in mice with PD undergoing TAC
| 1 | BROWN L J, OLIVER R C, LÖE H. Periodontal diseases in the US in 1981: prevalence, severity, extent, and role in tooth mortality[J]. J Periodontol, 1989, 60(7): 363-370. |
| 2 | KASSEBAUM N J, BERNABÉ E, DAHIYA M, et al. Global burden of severe periodontitis in 1990‒2010: a systematic review and meta-regression[J]. J Dent Res, 2014, 93(11): 1045-1053. |
| 3 | SANZ M, MARCO DEL CASTILLO A, JEPSEN S, et al. Periodontitis and cardiovascular diseases: consensus report[J]. J Clin Periodontol, 2020, 47(3): 268-288. |
| 4 | HAJISHENGALLIS G, CHAVAKIS T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities[J]. Nat Rev Immunol, 2021, 21(7): 426-440. |
| 5 | BOURGEOIS D, INQUIMBERT C, OTTOLENGHI L, et al. Periodontal pathogens as risk factors of cardiovascular diseases, diabetes, rheumatoid arthritis, cancer, and chronic obstructive pulmonary disease: is there cause for consideration? [J]. Microorganisms, 2019, 7(10): 424. |
| 6 | HILL J A, OLSON E N. Cardiac plasticity[J]. N Engl J Med, 2008, 358(13): 1370-1380. |
| 7 | SHIMIZU I, MINAMINO T. Physiological and pathological cardiac hypertrophy[J]. J Mol Cell Cardiol, 2016, 97: 245-262. |
| 8 | NAKAMURA M, SADOSHIMA J. Mechanisms of physiological and pathological cardiac hypertrophy[J]. Nat Rev Cardiol, 2018, 15(7): 387-407. |
| 9 | BAI L, CHEN B Y, LIU Y, et al. A mouse periodontitis model with humanized oral bacterial community[J]. Front Cell Infect Microbiol, 2022, 12: 842845. |
| 10 | WEI X, WU B, ZHAO J, et al. Myocardial hypertrophic preconditioning attenuates cardiomyocyte hypertrophy and slows progression to heart failure through upregulation of S100A8/A9[J]. Circulation, 2015, 131(17): 1506-1517;discussion1517. |
| 11 | ZAURA E, KEIJSER B J F, HUSE S M, et al. Defining the healthy “core microbiome” of oral microbial communities[J]. BMC Microbiol, 2009, 9: 259. |
| 12 | SEGATA N, IZARD J, WALDRON L, et al. Metagenomic biomarker discovery and explanation[J]. Genome Biol, 2011, 12(6): R60. |
| 13 | KOREN O, SPOR A, FELIN J, et al. Human oral, gut, and plaque microbiota in patients with atherosclerosis[J]. Proc Natl Acad Sci U S A, 2011, 108(Suppl 1): 4592-4598. |
| 14 | KINANE D F, STATHOPOULOU P G, PAPAPANOU P N. Periodontal diseases[J]. Nat Rev Dis Primers, 2017, 3: 17038. |
| 15 | ARMINGOHAR Z, JØRGENSEN J J, KRISTOFFERSEN A K, et al. Bacteria and bacterial DNA in atherosclerotic plaque and aneurysmal wall biopsies from patients with and without periodontitis[J]. J Oral Microbiol, 2014, 6. DOI: 10.3402/jom.v6.23408.eCollection 2014. |
| 16 | MAHENDRA J, MAHENDRA L, FELIX J, et al. Prevelance of periodontopathogenic bacteria in subgingival biofilm and atherosclerotic plaques of patients undergoing coronary revascularization surgery[J]. J Indian Soc Periodontol, 2013, 17(6): 719-724. |
| 17 | SHI B C, LUX R, KLOKKEVOLD P, et al. The subgingival microbiome associated with periodontitis in type 2 diabetes mellitus[J]. ISME J, 2020, 14(2): 519-530. |
| 18 | LIU X H, TIAN K, MA X R, et al. Analysis of subgingival microbiome of periodontal disease and rheumatoid arthritis in Chinese: a case-control study[J]. Saudi J Biol Sci, 2020, 27(7): 1835-1842. |
| 19 | KNÖLL R, IACCARINO G, TARONE G, et al. Towards a re-definition of 'cardiac hypertrophy' through a rational characterization of left ventricular phenotypes: a position paper of the Working Group 'Myocardial Function' of the ESC[J]. Eur J Heart Fail, 2011, 13(8): 811-819. |
| 20 | MCLELLAN A J A, ELLIMS A H, PRABHU S, et al. Diffuse ventricular fibrosis on cardiac magnetic resonance imaging associates with ventricular tachycardia in patients with hypertrophic cardiomyopathy[J]. J Cardiovasc Electrophysiol, 2016, 27(5): 571-580. |
| 21 | ALMAAS V M, HAUGAA K H, STRØM E H, et al. Increased amount of interstitial fibrosis predicts ventricular arrhythmias, and is associated with reduced myocardial septal function in patients with obstructive hypertrophic cardiomyopathy[J]. Europace, 2013, 15(9): 1319-1327. |
| 22 | MANN D L. Innate immunity and the failing heart: the cytokine hypothesis revisited[J]. Circ Res, 2015, 116(7): 1254-1268. |
| 23 | TRACHTENBERG B H, HARE J M. Inflammatory cardiomyopathic syndromes[J]. Circ Res, 2017, 121(7): 803-818. |
| 24 | HEUSCH G, LIBBY P, GERSH B, et al. Cardiovascular remodelling in coronary artery disease and heart failure[J]. Lancet, 2014, 383(9932): 1933-1943. |
| 25 | WEI Y P, SHI M, ZHEN M, et al. Comparison of subgingival and buccal mucosa microbiome in chronic and aggressive periodontitis: a pilot study[J]. Front Cell Infect Microbiol, 2019, 9: 53. |
| 26 | JI S, KIM Y, MIN B M, et al. Innate immune responses of gingival epithelial cells to nonperiodontopathic and periodontopathic bacteria[J]. J Periodontal Res, 2007, 42(6): 503-510. |
| 27 | PINHO-GOMES A C, NASIR A, MOSCA R, et al. Intraoperative diagnosis of mitral valve endocarditis secondary to Paenibacillus provencensis[J]. Ann R Coll Surg Engl, 2017, 99(2): e54-e55. |
| 28 | ZIGANSHINA E E, SHARIFULLINA D M, LOZHKIN A P, et al. Bacterial communities associated with atherosclerotic plaques from Russian individuals with atherosclerosis[J]. PLoS One, 2016, 11(10): e0164836. |
| 29 | SCHÄFFLER H, HERLEMANN D P R, ALBERTS C, et al. Mucosa-attached bacterial community in Crohn′s disease coheres with the clinical disease activity index[J]. Environ Microbiol Rep, 2016, 8(5): 614-621. |
| 30 | WANG Z N, HAZEN J, JIA X, et al. The nutritional supplement L-alpha glycerylphosphorylcholine promotes atherosclerosis[J]. Int J Mol Sci, 2021, 22(24): 13477. |
| 31 | TOYA T, CORBAN M T, MARRIETTA E, et al. Coronary artery disease is associated with an altered gut microbiome composition[J]. PLoS One, 2020, 15(1): e0227147. |
| 32 | LI Z H, WU Z Y, YAN J Y, et al. Gut microbe-derived metabolite trimethylamine N-oxide induces cardiac hypertrophy and fibrosis[J]. Lab Invest, 2019, 99(3): 346-357. |
| 33 | ZHAO M M, WEI H R, LI C Z, et al. Gut microbiota production of trimethyl-5-aminovaleric acid reduces fatty acid oxidation and accelerates cardiac hypertrophy[J]. Nat Commun, 2022, 13(1): 1757. |
| 34 | HEINEKE J, MOLKENTIN J D. Regulation of cardiac hypertrophy by intracellular signalling pathways[J]. Nat Rev Mol Cell Biol, 2006, 7(8): 589-600. |
| 35 | BILLET S, BARDIN S, VERP S, et al. Gain-of-function mutant of angiotensin Ⅱ receptor, type 1A, causes hypertension and cardiovascular fibrosis in mice[J]. J Clin Invest, 2007, 117(7): 1914-1925. |
| 36 | BOUTHIER J D, DE LUCA N, SAFAR M E, et al. Cardiac hypertrophy and arterial distensibility in essential hypertension[J]. Am Heart J, 1985, 109(6): 1345-1352. |
| 37 | SRIVASTAVA P M, CALAFIORE P, MACISAAC R J, et al. Prevalence and predictors of cardiac hypertrophy and dysfunction in patients with type 2 diabetes[J]. Clin Sci (Lond), 2008, 114(4): 313-320. |
| 38 | HU Q X, ZHANG H L, GUTIÉRREZ CORTÉS N, et al. Increased Drp1 acetylation by lipid overload induces cardiomyocyte death and heart dysfunction[J]. Circ Res, 2020, 126(4): 456-470. |
| 39 | RUBIN S A, FISHBEIN M C, SWAN H J. Compensatory hypertrophy in the heart after myocardial infarction in the rat[J]. J Am Coll Cardiol, 1983, 1(6): 1435-1441. |
| 40 | PFEFFER M A, BRAUNWALD E. Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications[J]. Circulation, 1990, 81(4): 1161-1172. |
| 41 | EVERETT R J, TASTET L, CLAVEL M A, et al. Progression of hypertrophy and myocardial fibrosis in aortic stenosis: a multicenter cardiac magnetic resonance study[J]. Circ Cardiovasc Imaging, 2018, 11(6): e007451. |
| [1] | 周亦凝, 叶之韵, 陈慧文, 谢欣宜, 周薇, 宋忠臣. Th17细胞特异性敲除Stat3对牙周炎小鼠焦虑抑郁样行为的影响[J]. 上海交通大学学报(医学版), 2025, 45(7): 838-845. |
| [2] | 王佳璇, 张骞骞, 隋佰延, 刘昕. 重度牙周炎小鼠模型构建方法的优化与评价[J]. 上海交通大学学报(医学版), 2025, 45(1): 79-86. |
| [3] | 李虎虓, 李笑甜, 赵旭日, 张桓瑜, 周薇, 宋忠臣. 牙龈素提取物对口腔鳞癌细胞HN6生物学特性的影响[J]. 上海交通大学学报(医学版), 2024, 44(2): 161-168. |
| [4] | 谢欣宜, 周薇, 邱澈, 沈慧, 宋忠臣. 伴阿尔茨海默病牙周炎患者血清Th17/Treg相关细胞因子水平变化研究[J]. 上海交通大学学报(医学版), 2023, 43(5): 600-605. |
| [5] | 丁远森, 王枫, 孙家悦, 邵正威, 邹德荣, 陆家瑜. 不同年龄2型糖尿病患者牙周健康流行病学调查[J]. 上海交通大学学报(医学版), 2021, 41(2): 217-222. |
| [6] | 邓 海1,佟 琰1,Kristine SUN2,夏欣怡2,李 璞1,张春丽1,胡 春1,宋忠臣2,刘英莉1. 慢性牙周炎在腹膜透析患者中的发病状况及其与患者透析充分性的相关性研究[J]. 上海交通大学学报(医学版), 2020, 40(7): 943-949. |
| [7] | 夏欣怡,陈慧文,胡 苡,宋忠臣. 硫酸吲哚酚对人牙周膜细胞增殖及炎症因子表达的影响[J]. 上海交通大学学报(医学版), 2020, 40(4): 437-. |
| [8] | 胡 苡1, 2,周 薇2,宋忠臣1, 2. 实验性牙周炎大鼠脑内外的炎性改变[J]. 上海交通大学学报(医学版), 2020, 40(12): 1579-1584. |
| [9] | 袁 芸,张洪铭,黄 慧. 牙周炎对大鼠外周血中辅助性T细胞分群的影响[J]. 上海交通大学学报(医学版), 2020, 40(10): 1360-1364. |
| [10] | 王雅萍,林智恺,束蓉. Er,Cr:YSGG激光辅助龈下刮治对重度牙周炎患者的短期 临床疗效[J]. 上海交通大学学报(医学版), 2019, 39(4): 378-. |
| [11] | 钱洁蕾,束蓉,王依玮,谢玉峰. 慢性牙周炎易感患者种植体周围角化黏膜对种植体周软组织 健康的影响[J]. 上海交通大学学报(医学版), 2018, 38(8): 929-. |
| [12] | 姜春兰,程惠娟,焦婷. 亚甲基蓝介导的光动力疗法诱导牙周炎中巨噬细胞凋亡的体内外研究[J]. 上海交通大学学报(医学版), 2018, 38(12): 1429-. |
| [13] | 胡淑澄,束蓉,宋忠臣,孙梦君,王依玮. 光化合技术辅助治疗慢性牙周炎的临床效果[J]. 上海交通大学学报(医学版), 2017, 37(5): 621-. |
| [14] | 李超伦,刘大力,谢玉峰,宋忠臣,葛琳华,束蓉. 医学院学生牙周健康状态的流行病学研究[J]. 上海交通大学学报(医学版), 2017, 37(4): 545-. |
| [15] | 钱洁蕾,束蓉,宋忠臣,谢玉峰,王依玮. 慢性牙周炎患者种植体3年存活情况分析[J]. 上海交通大学学报(医学版), 2017, 37(3): 368-. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||