
上海交通大学学报(医学版) ›› 2023, Vol. 43 ›› Issue (2): 230-236.doi: 10.3969/j.issn.1674-8115.2023.02.013
收稿日期:2022-08-02
接受日期:2022-11-03
出版日期:2023-02-28
发布日期:2023-02-28
通讯作者:
郑宪友,电子信箱:zhengxianyou@126.com。作者简介:刘铁鑫 (1999—),男,博士生;电子信箱:ltx19821875723@163.com。
基金资助:
LIU Tiexin( ), LIN Junqing, ZHENG Xianyou(
), LIN Junqing, ZHENG Xianyou( )
)
Received:2022-08-02
Accepted:2022-11-03
Online:2023-02-28
Published:2023-02-28
Contact:
ZHENG Xianyou, E-mail: zhengxianyou@126.com.Supported by:摘要:
脊髓损伤是一种能对患者的感觉功能、运动功能以及自主神经功能造成极大影响的疾病,它不仅给患者本人带来严重身心伤害,还对社会造成巨大的经济负担。随着医疗技术的发展,对脊髓损伤内在机制的研究也在不断深入,脊髓损伤的治疗方法层出不穷,但其疗效欠佳,因此亟需进一步探索新的脊髓损伤治疗策略,拓展新的治疗思路。诸多研究表明,各种亚细胞结构与脊髓损伤后损伤部位神经再生及功能恢复密切相关,因此靶向线粒体、溶酶体/自噬体、内质网、胞内体和蛋白酶体等亚细胞结构治疗脊髓损伤可望在促进脊髓损伤后神经再生与修复中起重要作用。多种靶向亚细胞结构的治疗策略在脊髓损伤治疗中效果显著,其中又以靶向线粒体或内质网治疗脊髓损伤的研究为主。靶向线粒体治疗主要着重于维持损伤部位线粒体能量代谢水平,而靶向内质网治疗主要着重于抑制内质网应激。该文就靶向亚细胞结构治疗在脊髓损伤修复中的应用研究进展作一综述,可望为开发脊髓损伤的新型靶向治疗策略、提高脊髓损伤治疗效果提供新思路。
中图分类号:
刘铁鑫, 林俊卿, 郑宪友. 靶向亚细胞结构治疗脊髓损伤的研究进展[J]. 上海交通大学学报(医学版), 2023, 43(2): 230-236.
LIU Tiexin, LIN Junqing, ZHENG Xianyou. Research progress of subcellular structure-targeted therapy in spinal cord injury[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2023, 43(2): 230-236.
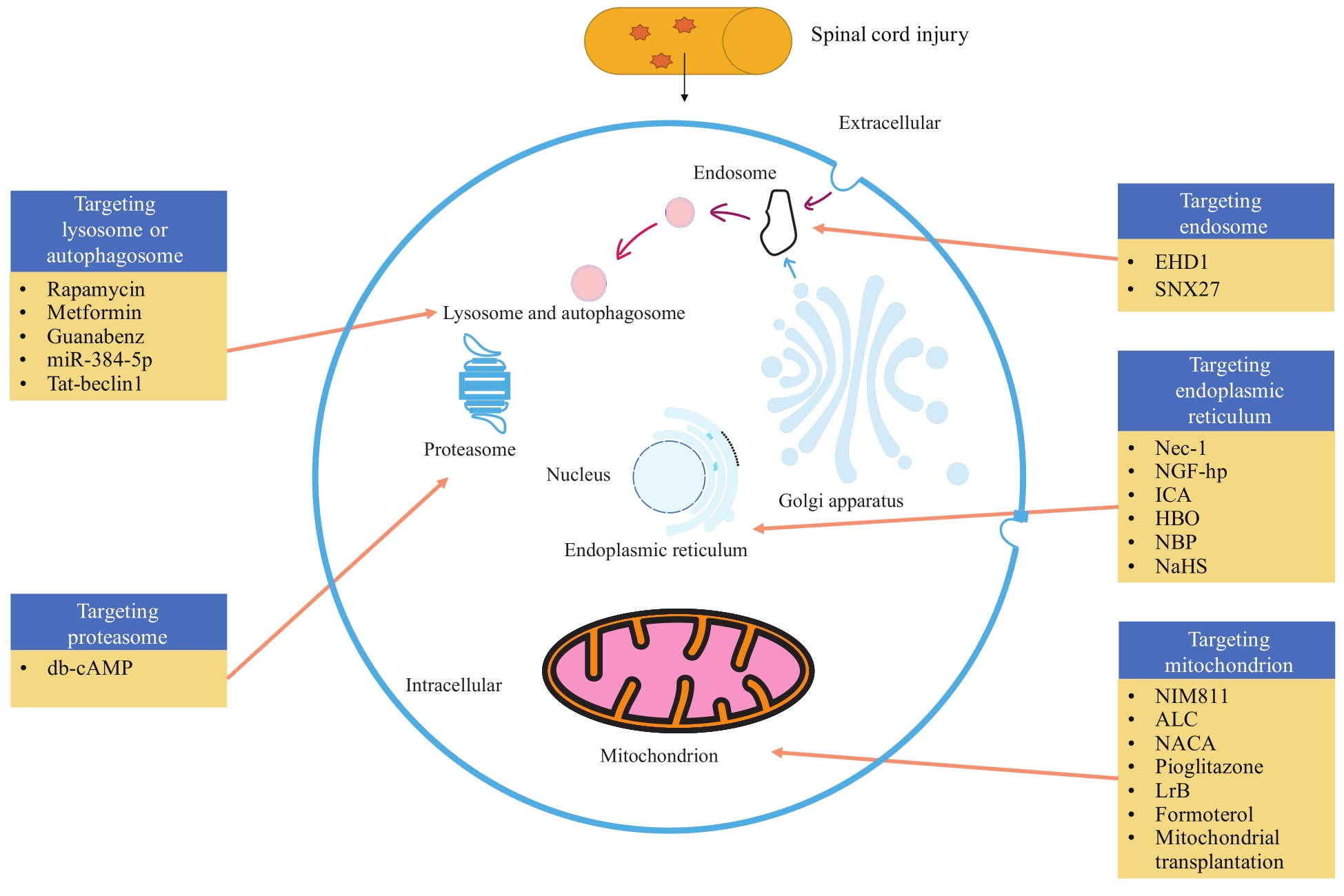
图1 靶向亚细胞结构治疗脊髓损伤示意图Note: EHD1—Eps15 homology domain protein 1; SNX27—sorting nexin family member 27; Nec-1—necrostatin-1; NGF-hp—nerve growth factor heparin-poloxamer; ICA—icariin; HBO—hyperbaric oxygen therapy; NBP—Dl-3-n-butylphthalein; ALC—acetyl-l-carnitine; NACA—n-acetylcysteine amide; LrB—loracerin B; db-cAMP—dibutyl-cAMP.
Fig 1 Schematic diagram of targeted subcellular structures for spinal cord injury
| 1 | COURTINE G, SOFRONIEW M V. Spinal cord repair: advances in biology and technology[J]. Nat Med, 2019, 25(6): 898-908. |
| 2 | FEHLINGS M G, TETREAULT L A, WILSON J R, et al. A clinical practice guideline for the management of acute spinal cord injury: introduction, rationale, and scope[J]. Global Spine J, 2017, 7(3 Suppl): 84S-94S. |
| 3 | 陈星月, 陈栋, 陈春慧, 等. 中国创伤性脊髓损伤流行病学和疾病经济负担的系统评价[J]. 中国循证医学杂志, 2018, 18(2): 143-150. |
| CHEN X Y, CHEN D, CHEN C H, et al. The epidemiology and disease burden of traumatic spinal cord injury in China: a systematic review[J]. Chinese Journal of Evidence-Based Medicine, 2018, 18(2): 143-150. | |
| 4 | PETROVA V, NIEUWENHUIS B, FAWCETT J W, et al. Axonal organelles as molecular platforms for axon growth and regeneration after injury[J]. Int J Mol Sci, 2021, 22(4): 1798. |
| 5 | BARTOLÁK-SUKI E, IMSIROVIC J, NISHIBORI Y, et al. Regulation of mitochondrial structure and dynamics by the cytoskeleton and mechanical factors[J]. Int J Mol Sci, 2017, 18(8): 1812. |
| 6 | HAN S M, BAIG H S, HAMMARLUND M. Mitochondria localize to injured axons to support regeneration[J]. Neuron, 2016, 92(6): 1308-1323. |
| 7 | CAVALLUCCI V, BISICCHIA E, CENCIONI M T, et al. Acute focal brain damage alters mitochondrial dynamics and autophagy in axotomized neurons[J]. Cell Death Dis, 2014, 5(11): e1545. |
| 8 | MALLA B, NIESNER R, HAUSER A, et al. Imaging and analysis of neuronal mitochondria in murine acute brain slices[J]. J Neurosci Methods, 2022, 372: 109558. |
| 9 | BALLABIO A, BONIFACINO J S. Lysosomes as dynamic regulators of cell and organismal homeostasis[J]. Nat Rev Mol Cell Biol, 2020, 21(2): 101-118. |
| 10 | STAVOE A K H, HOLZBAUR E L F. Autophagy in neurons[J]. Annu Rev Cell Dev Biol, 2019, 35: 477-500. |
| 11 | SAKAMOTO K, OZAKI T, KO Y C, et al. Glycan sulfation patterns define autophagy flux at axon tip via PTPRσ-cortactin axis[J]. Nat Chem Biol, 2019, 15(7): 699-709. |
| 12 | WEI X Y, LUO L F, CHEN J Z. Roles of mTOR signaling in tissue regeneration[J]. Cells, 2019, 8(9): 1075. |
| 13 | RABANAL-RUIZ Y, KOROLCHUK V I. mTORC1 and nutrient homeostasis: the central role of the lysosome[J]. Int J Mol Sci, 2018, 19(3): 818. |
| 14 | JEHAN C, CARTIER D, BUCHARLES C, et al. Emerging roles of ER-resident selenoproteins in brain physiology and physiopathology[J]. Redox Biol, 2022, 55: 102412. |
| 15 | JACQUEMYN J, CASCALHO A, GOODCHILD R E. The ins and outs of endoplasmic reticulum-controlled lipid biosynthesis[J]. EMBO Rep, 2017, 18(11): 1905-1921. |
| 16 | TOJIMA T, KAMIGUCHI H. Exocytic and endocytic membrane trafficking in axon development[J]. Dev Growth Differ, 2015, 57(4): 291-304. |
| 17 | WOJNACKI J, GALLI T. Membrane traffic during axon development[J]. Dev Neurobiol, 2016, 76(11): 1185-1200. |
| 18 | YAP C C, WINCKLER B. Harnessing the power of the endosome to regulate neural development[J]. Neuron, 2012, 74(3): 440-451. |
| 19 | KORHONEN L, LINDHOLM D. The ubiquitin proteasome system in synaptic and axonal degeneration: a new twist to an old cycle[J]. J Cell Biol, 2004, 165(1): 27-30. |
| 20 | LEE M, LIU Y C, CHEN C, et al. Ecm29-mediated proteasomal distribution modulates excitatory GABA responses in the developing brain[J]. J Cell Biol, 2020, 219(2): e201903033. |
| 21 | DI PAOLO A, GARAT J, EASTMAN G, et al. Functional genomics of axons and synapses to understand neurodegenerative diseases[J]. Front Cell Neurosci, 2021, 15: 686722. |
| 22 | NJOMEN E, TEPE J J. Proteasome activation as a new therapeutic approach to target proteotoxic disorders[J]. J Med Chem, 2019, 62(14): 6469-6481. |
| 23 | TAKABATAKE M, GOSHIMA Y, SASAKI Y. Semaphorin-3A promotes degradation of fragile X mental retardation protein in growth cones via the ubiquitin-proteasome pathway[J]. Front Neural Circuits, 2020, 14: 5. |
| 24 | JIN E J, KO H R, HWANG I, et al. Akt regulates neurite growth by phosphorylation-dependent inhibition of radixin proteasomal degradation[J]. Sci Rep, 2018, 8(1): 2557. |
| 25 | HE L H, LEMASTERS J J. Regulated and unregulated mitochondrial permeability transition pores: a new paradigm of pore structure and function?[J]. FEBS Lett, 2002, 512(1/2/3): 1-7. |
| 26 | MCEWEN M L, SULLIVAN P G, SPRINGER J E. Pretreatment with the cyclosporin derivative, NIM811, improves the function of synaptic mitochondria following spinal cord contusion in rats[J]. J Neurotrauma, 2007, 24(4): 613-624. |
| 27 | PATEL S P, SULLIVAN P G, LYTTLE T S, et al. Acetyl-L-carnitine treatment following spinal cord injury improves mitochondrial function correlated with remarkable tissue sparing and functional recovery[J]. Neuroscience, 2012, 210: 296-307. |
| 28 | PATEL S P, SULLIVAN P G, PANDYA J D, et al. N-acetylcysteine amide preserves mitochondrial bioenergetics and improves functional recovery following spinal trauma[J]. Exp Neurol, 2014, 257: 95-105. |
| 29 | PATEL S P, COX D H, GOLLIHUE J L, et al. Pioglitazone treatment following spinal cord injury maintains acute mitochondrial integrity and increases chronic tissue sparing and functional recovery[J]. Exp Neurol, 2017, 293: 74-82. |
| 30 | WANG Q Q, CAI H X, HU Z X, et al. Loureirin B promotes axon regeneration by inhibiting endoplasmic reticulum stress: induced mitochondrial dysfunction and regulating the Akt/GSK-3β pathway after spinal cord injury[J]. J Neurotrauma, 2019, 36(12): 1949-1964. |
| 31 | SCHOLPA N E, WILLIAMS H, WANG W X, et al. Pharmacological stimulation of mitochondrial biogenesis using the food and drug administration-approved β2-adrenoreceptor agonist formoterol for the treatment of spinal cord injury[J]. J Neurotrauma, 2019, 36(6): 962-972. |
| 32 | GOLLIHUE J L, PATEL S P, RABCHEVSKY A G. Mitochondrial transplantation strategies as potential therapeutics for central nervous system trauma[J]. Neural Regen Res, 2018, 13(2): 194-197. |
| 33 | GOLLIHUE J L, PATEL S P, ELDAHAN K C, et al. Effects of mitochondrial transplantation on bioenergetics, cellular incorporation, and functional recovery after spinal cord injury[J]. J Neurotrauma, 2018, 35(15): 1800-1818. |
| 34 | KANNO H, OZAWA H, SEKIGUCHI A, et al. The role of mTOR signaling pathway in spinal cord injury[J]. Cell Cycle, 2012, 11(17): 3175-3179. |
| 35 | ZHANG D, XUAN J, ZHENG B B, et al. Metformin improves functional recovery after spinal cord injury via autophagy flux stimulation[J]. Mol Neurobiol, 2017, 54(5): 3327-3341. |
| 36 | WU Y Q, XIONG J, HE Z L, et al. Metformin promotes microglial cells to facilitate myelin debris clearance and accelerate nerve repairment after spinal cord injury[J]. Acta Pharmacol Sin, 2022, 43(6): 1360-1371. |
| 37 | HETZ C. The unfolded protein response: controlling cell fate decisions under ER stress and beyond[J]. Nat Rev Mol Cell Biol, 2012, 13(2): 89-102. |
| 38 | BISICCHIA E, MASTRANTONIO R, NOBILI A, et al. Restoration of ER proteostasis attenuates remote apoptotic cell death after spinal cord injury by reducing autophagosome overload[J]. Cell Death Dis, 2022, 13(4): 381. |
| 39 | ZHOU Z J, HU B W, LYU Q N, et al. MiR-384-5p promotes spinal cord injury recovery in rats through suppressing of autophagy and endoplasmic reticulum stress[J]. Neurosci Lett, 2020, 727: 134937. |
| 40 | HE M, DING Y T, CHU C, et al. Autophagy induction stabilizes microtubules and promotes axon regeneration after spinal cord injury[J]. Proc Natl Acad Sci USA, 2016, 113(40): 11324-11329. |
| 41 | WANG S, WU J, ZENG Y Z, et al. Necrostatin-1 mitigates endoplasmic reticulum stress after spinal cord injury[J]. Neurochem Res, 2017, 42(12): 3548-3558. |
| 42 | LI Y, ZHANG J, ZHOU K L, et al. Elevating sestrin2 attenuates endoplasmic reticulum stress and improves functional recovery through autophagy activation after spinal cord injury[J]. Cell Biol Toxicol, 2021, 37(3): 401-419. |
| 43 | FU H T, HU D, CHEN J L, et al. Repair of the injured spinal cord by schwann cell transplantation[J]. Front Neurosci, 2022, 16: 800513. |
| 44 | ZHAO Y Z, JIANG X, XIAO J, et al. Using NGF heparin-poloxamer thermosensitive hydrogels to enhance the nerve regeneration for spinal cord injury[J]. Acta Biomater, 2016, 29: 71-80. |
| 45 | LI H T, ZHANG X R, QI X, et al. Icariin inhibits endoplasmic reticulum stress-induced neuronal apoptosis after spinal cord injury through modulating the PI3K/AKT signaling pathway[J]. Int J Biol Sci, 2019, 15(2): 277-286. |
| 46 | LIU X H, YANG J, LI Z, et al. Hyperbaric oxygen treatment protects against spinal cord injury by inhibiting endoplasmic reticulum stress in rats[J]. Spine, 2015, 40(24): E1276-E1283. |
| 47 | WU Q, ZHANG Y J, GAO J Y, et al. Aquaporin-4 mitigates retrograde degeneration of rubrospinal neurons by facilitating edema clearance and glial scar formation after spinal cord injury in mice[J]. Mol Neurobiol, 2014, 49(3): 1327-1337. |
| 48 | ZHENG B B, ZHOU Y L, ZHANG H Y, et al. Dl-3-n-butylphthalide prevents the disruption of blood-spinal cord barrier via inhibiting endoplasmic reticulum stress following spinal cord injury[J]. Int J Biol Sci, 2017, 13(12): 1520-1531. |
| 49 | WANG H L, WU Y Q, HAN W, et al. Hydrogen sulfide ameliorates blood-spinal cord barrier disruption and improves functional recovery by inhibiting endoplasmic reticulum stress-dependent autophagy[J]. Front Pharmacol, 2018, 9: 858. |
| 50 | KOBAYASHI H, ETOH K, FUKUDA M. Rab35 is translocated from Arf6-positive perinuclear recycling endosomes to neurite tips during neurite outgrowth[J]. Small GTPases, 2014, 5(3): e983874. |
| 51 | WU C S, CUI Z M, LIU Y H, et al. The importance of EHD1 in neurite outgrowth contributing to the functional recovery after spinal cord injury[J]. Int J Dev Neurosci, 2016, 52: 24-32. |
| 52 | GALLON M, CLAIRFEUILLE T, STEINBERG F, et al. A unique PDZ domain and arrestin-like fold interaction reveals mechanistic details of endocytic recycling by SNX27-retromer[J]. Proc Natl Acad Sci USA, 2014, 111(35): E3604-E3613. |
| 53 | ZENG Y Z, WANG N W, GUO T T, et al. Snx27 deletion promotes recovery from spinal cord injury by neuroprotection and reduces macrophage/microglia proliferation[J]. Front Neurol, 2018, 9: 1059. |
| 54 | SPITZBARTH I, MOORE S A, STEIN V M, et al. Current insights into the pathology of canine intervertebral disc extrusion-induced spinal cord injury[J]. Front Vet Sci, 2020, 7: 595796. |
| 55 | MYEKU N, WANG H, FIGUEIREDO-PEREIRA M E. cAMP stimulates the ubiquitin/proteasome pathway in rat spinal cord neurons[J]. Neurosci Lett, 2012, 527(2): 126-131. |
| 56 | MORIWAKI K, CHAN F K M. RIP3: a molecular switch for necrosis and inflammation[J]. Genes Dev, 2013, 27(15): 1640-1649. |
| 57 | WU C S, CHEN J J, LIU Y H, et al. Upregulation of PSMB4 is associated with the necroptosis after spinal cord injury[J]. Neurochem Res, 2016, 41(11): 3103-3112. |
| 58 | TICA J R, BRADBURY E J, DIDANGELOS A. Combined transcriptomics, proteomics and bioinformatics identify drug targets in spinal cord injury[J]. Int J Mol Sci, 2018, 19(5): 1461. |
| [1] | 韩龙传, 李悦, 邹智慧, 罗静, 李若伊, 张颖婷, 唐欣欣, 田丽红, 陆宇恒, 黄莺, 贺明, 付寅坤. 磷脂酰乙醇胺引起内质网应激促进巨噬细胞衰老及肝损伤[J]. 上海交通大学学报(医学版), 2025, 45(6): 693-704. |
| [2] | 杨乐, 周怡, 王钶韵, 赖娅莉. 大黄素改善阿尔茨海默病认知障碍、内质网应激和神经炎症的研究[J]. 上海交通大学学报(医学版), 2025, 45(6): 727-734. |
| [3] | 禹恺, 帅哲玮, 黄洪军, 罗艳. 小胶质细胞在中枢神经系统炎症性疾病中的作用和机制研究进展[J]. 上海交通大学学报(医学版), 2025, 45(5): 630-638. |
| [4] | 罗文, 吕明君, 张珍, 张雪, 姚志荣. 自噬在皮肤黑色素瘤中的双重效应及耐药中的作用研究进展[J]. 上海交通大学学报(医学版), 2025, 45(2): 233-240. |
| [5] | 唐珺倩, 李本尚. 儿童高危细胞遗传学B系急性淋巴细胞白血病治疗新进展[J]. 上海交通大学学报(医学版), 2025, 45(10): 1390-1399. |
| [6] | 张勇, 李伟宏, 程志鹏, 王斌, 王思珩, 王毓斌. 受体相互作用蛋白激酶1调节癌症进展和免疫反应的研究现状[J]. 上海交通大学学报(医学版), 2024, 44(6): 788-794. |
| [7] | 徐文晖, 杨畅, 李瑞卿, 卞京, 李夏伊, 郑磊贞. 干扰素调节因子3促结直肠癌细胞增殖与侵袭相关探索[J]. 上海交通大学学报(医学版), 2024, 44(3): 301-311. |
| [8] | 丁艳玲, 李杰, 袁军, 李燕. 慢性淋巴细胞白血病靶向治疗的研究进展[J]. 上海交通大学学报(医学版), 2024, 44(2): 264-270. |
| [9] | 唐思洁, 糜坚青. 抗体药物偶联物在血液肿瘤中的临床应用研究进展[J]. 上海交通大学学报(医学版), 2024, 44(12): 1607-1614. |
| [10] | 方馨悦, 石岚, 夏思易, 王佳璇, 吴英理, 何珂骏. Menin-MLL蛋白相互作用及相关抑制剂在MLL基因重排白血病中应用的研究进展[J]. 上海交通大学学报(医学版), 2024, 44(10): 1287-1298. |
| [11] | 贾君杰, 邢海帆, 张群子, 刘奇烨, 汪年松, 范瑛. 缺氧诱导因子-1α抑 制剂YC-1改善糖尿病肾病小鼠肾脏损伤的机制研究[J]. 上海交通大学学报(医学版), 2023, 43(9): 1089-1098. |
| [12] | 周婉桢, 滕银成. 非经典Wnt通路在卵巢癌中的作用与潜在治疗意义研究进展[J]. 上海交通大学学报(医学版), 2023, 43(8): 1056-1063. |
| [13] | 董海平, 谢海怡, 马晓晓, 王震虹. 脑卒中后脑血管内皮细胞内质网应激抑制Wnt7/β-catenin通路导致血脑屏障损伤的机制研究[J]. 上海交通大学学报(医学版), 2023, 43(7): 829-838. |
| [14] | 梅艳青, 韩雨洁, 翁文筠, 张蕾, 唐玉杰. 靶向抑制CDK12/13在高级别胶质瘤中的体外治疗效果和作用分子机制探究[J]. 上海交通大学学报(医学版), 2023, 43(5): 545-559. |
| [15] | 徐瀛濂, 田静, 张翔, 赵顺英. 气道上皮细胞在哮喘发病机制中的作用研究进展[J]. 上海交通大学学报(医学版), 2023, 43(5): 619-623. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||