
上海交通大学学报(医学版) ›› 2025, Vol. 45 ›› Issue (6): 792-799.doi: 10.3969/j.issn.1674-8115.2025.06.015
黄英荷1, 招冠钰1, 孙阳1, 侯鉴基1, 左勇1,2( )
)
收稿日期:2025-02-24
接受日期:2025-03-26
出版日期:2025-06-23
发布日期:2025-06-23
通讯作者:
左 勇,研究员,博士;电子信箱:zuoyong@shsmu.edu.cn。作者简介:黄英荷(2001—),女,硕士生;电子信箱:1152451431@qq.com。
基金资助:
HUANG Yinghe1, ZHAO Guanyu1, SUN Yang1, HOU Jianji1, ZUO Yong1,2( )
)
Received:2025-02-24
Accepted:2025-03-26
Online:2025-06-23
Published:2025-06-23
Contact:
ZUO Yong, E-mail: zuoyong@shsmu.edu.cn.Supported by:摘要:
全球成人糖尿病患病率逐年递增,其中以2型糖尿病(diabetes mellitus type 2,T2DM)为主。T2DM是由胰岛素抵抗和胰岛素分泌不足引起的伴随糖、蛋白质和脂肪代谢紊乱的一种慢性疾病。创面愈合障碍是T2DM的主要并发症之一。研究表明T2DM患者创面愈合受巨噬细胞调控,并与其表型、活性和数量相关。不同表型的巨噬细胞在T2DM创面愈合的各个阶段扮演不同角色:M1型巨噬细胞参与创伤早期的炎症反应和病原体清除,M2型巨噬细胞在创面愈合后期发挥抗炎症作用并介导创面修复。巨噬细胞表型转换障碍影响创面炎症反应、皮肤细胞功能和细胞外基质(extracellular matrix,ECM)合成等过程,最终导致愈合障碍。目前,巨噬细胞代谢改变与表型转换之间的相互作用机制研究取得了显著进展,且这种动态关联可能通过协同调控参与T2DM创面的愈合进程。该文总结巨噬细胞在正常创面愈合与T2DM患者创面愈合中的功能特点,就病理环境下巨噬细胞糖代谢、脂质代谢和氨基酸代谢变化及这些变化对创面愈合的调控作用展开综述,并讨论靶向巨噬细胞代谢治疗创面愈合的应用前景。
中图分类号:
黄英荷, 招冠钰, 孙阳, 侯鉴基, 左勇. 2型糖尿病创面愈合中巨噬细胞代谢调控的研究进展[J]. 上海交通大学学报(医学版), 2025, 45(6): 792-799.
HUANG Yinghe, ZHAO Guanyu, SUN Yang, HOU Jianji, ZUO Yong. Research progress on macrophage metabolic regulation in wound healing of diabetes mellitus type 2[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2025, 45(6): 792-799.
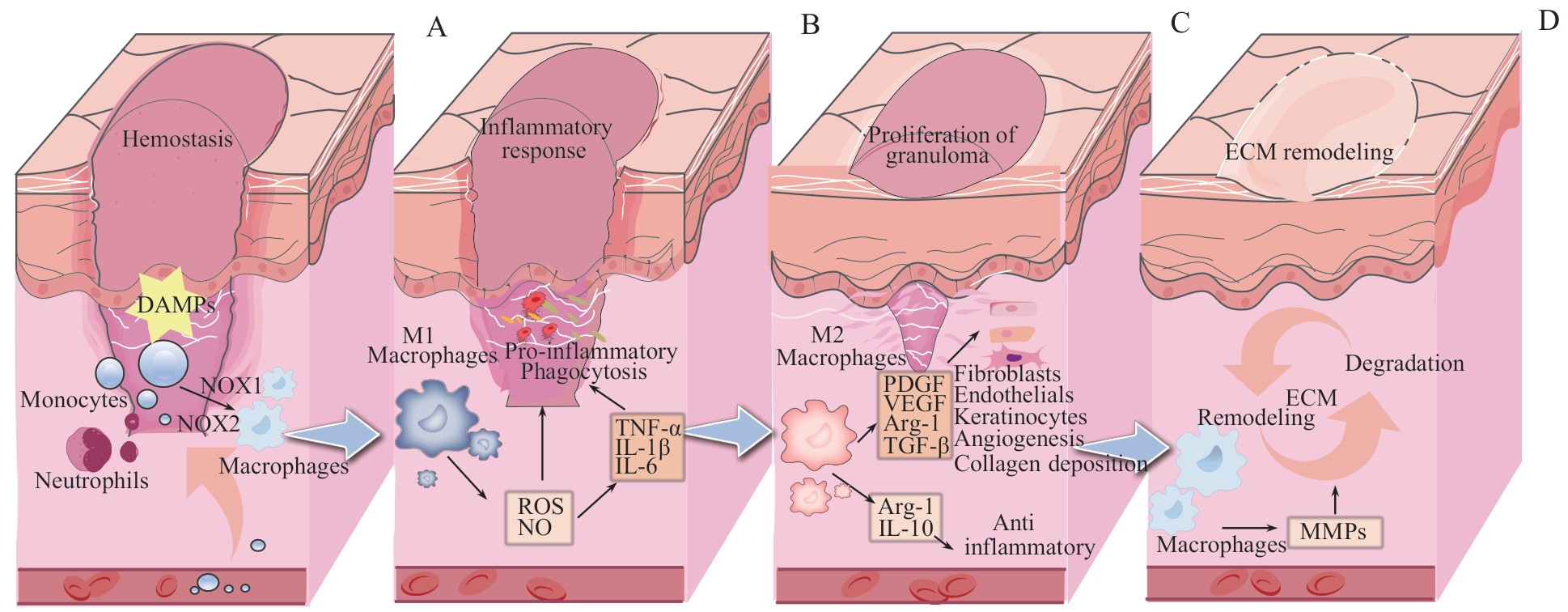
图1 正常创面愈合过程中巨噬细胞的作用机制Note: A. Hemostasis period. B. Inflammatory response period. C. Granulation tissue proliferation period. D. ECM remodeling period. DAMPs—damage-associated molecular patterns; NOX1—NADPH oxidase 1; NOX2—NADPH oxidase 2; VEGF—vascular endothelial growth factor; PDGF—platelet-derived growth factor.
Fig 1 Mechanisms of macrophage function in normal wound healing
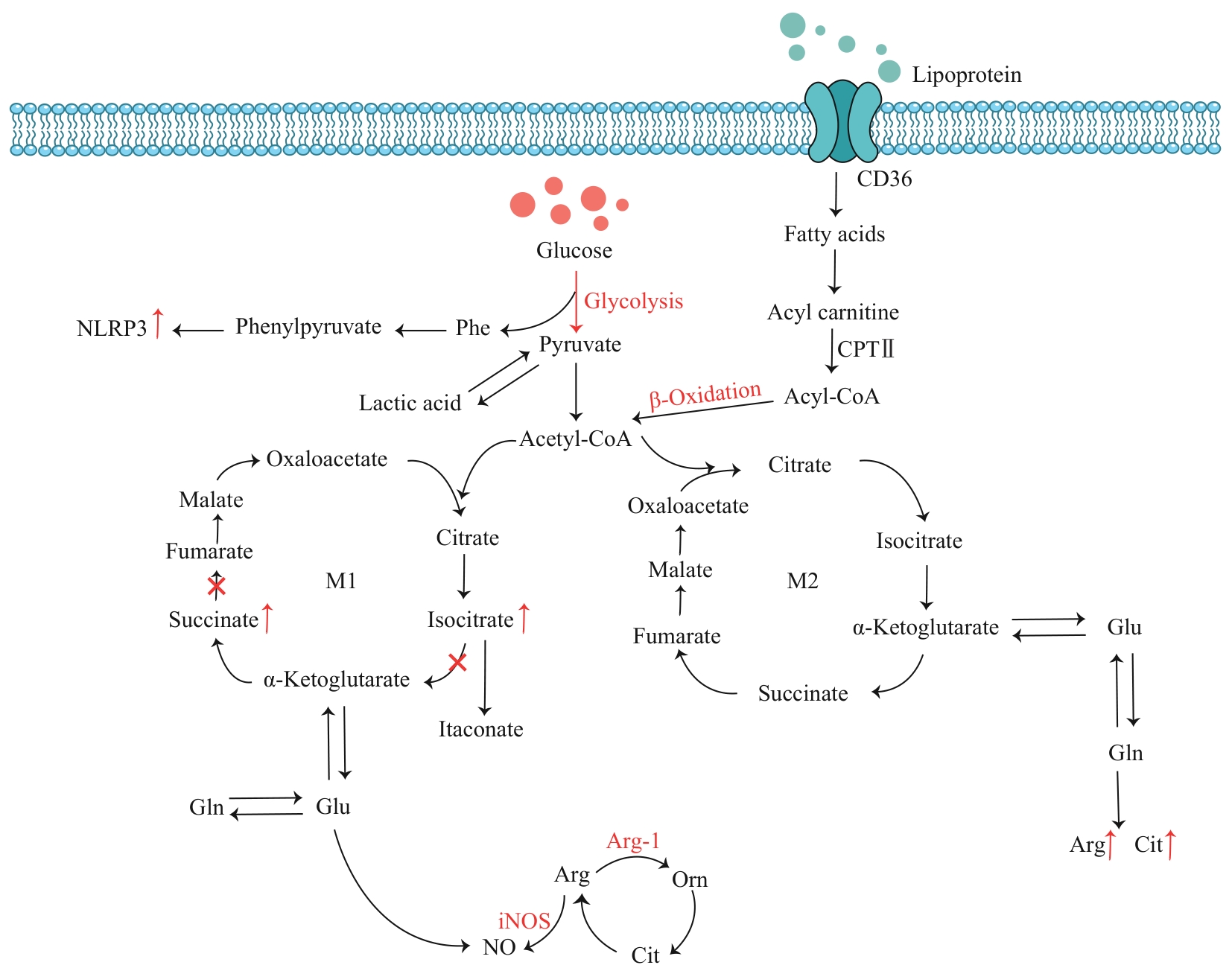
图2 创面中巨噬细胞代谢机制图Note: Phe—phenylalanine; Gln—glutamine; Glu—glutamic acid; Arg—arginine; Orn—ornithine; Cit—citrulline; CPTⅡ—carnitine palmotoyltransferase Ⅱ; Arg-1—arginase-1.
Fig 2 Diagram of macrophage metabolic mechanisms in wounds
| [1] | FREEDMAN B R, HWANG C, TALBOT S, et al. Breakthrough treatments for accelerated wound healing[J]. Sci Adv, 2023, 9(20): eade7007. |
| [2] | YU F X, LEE P S Y, YANG L L, et al. The impact of sensory neuropathy and inflammation on epithelial wound healing in diabetic corneas[J]. Prog Retin Eye Res, 2022, 89: 101039. |
| [3] | KAUSHIK K, DAS A. TWIST1-reprogrammed endothelial cell transplantation potentiates neovascularization-mediated diabetic wound tissue regeneration[J]. Diabetes, 2020, 69(6): 1232-1247. |
| [4] | GUO W, QIU W, AO X, et al. Low-concentration DMSO accelerates skin wound healing by Akt/mTOR-mediated cell proliferation and migration in diabetic mice[J]. Br J Pharmacol, 2020, 177(14): 3327-3341. |
| [5] | SHARIFIAGHDAM M, SHAABANI E, FARIDI-MAJIDI R, et al. Macrophages as a therapeutic target to promote diabetic wound healing[J]. Mol Ther, 2022, 30(9): 2891-2908. |
| [6] | WOLF S J, MELVIN W J, GALLAGHER K. Macrophage-mediated inflammation in diabetic wound repair[J]. Semin Cell Dev Biol, 2021, 119: 111-118. |
| [7] | ZHOU B S, MAGANA L, HONG Z G, et al. The angiocrine Rspondin3 instructs interstitial macrophage transition via metabolic-epigenetic reprogramming and resolves inflammatory injury[J]. Nat Immunol, 2020, 21(11): 1430-1443. |
| [8] | XIE J, WU X W, ZHENG S, et al. Aligned electrospun poly(L-lactide) nanofibers facilitate wound healing by inhibiting macrophage M1 polarization via the JAK-STAT and NF-κB pathways[J]. J Nanobiotechnology, 2022, 20(1): 342. |
| [9] | SHAN X, HU P H, NI L N, et al. Serine metabolism orchestrates macrophage polarization by regulating the IGF1-p38 axis[J]. Cell Mol Immunol, 2022, 19(11): 1263-1278. |
| [10] | AUDU C O, MELVIN W J, JOSHI A D, et al. Macrophage-specific inhibition of the histone demethylase JMJD3 decreases STING and pathologic inflammation in diabetic wound repair[J]. Cell Mol Immunol, 2022, 19(11): 1251-1262. |
| [11] | PEÑA O A, MARTIN P. Cellular and molecular mechanisms of skin wound healing[J]. Nat Rev Mol Cell Biol, 2024, 25(8): 599-616. |
| [12] | BRAZIL J C, QUIROS M, NUSRAT A, et al. Innate immune cell-epithelial crosstalk during wound repair[J]. J Clin Invest, 2019, 129(8): 2983-2993. |
| [13] | APAYDIN O, ALTAIKYZY A, FILOSA A, et al. Alpha-1 adrenergic signaling drives cardiac regeneration via extracellular matrix remodeling transcriptional program in zebrafish macrophages[J]. Dev Cell, 2023, 58(22): 2460-2476.e7. |
| [14] | REYNOLDS G, VEGH P, FLETCHER J, et al. Developmental cell programs are co-opted in inflammatory skin disease[J]. Science, 2021, 371(6527): eaba6500. |
| [15] | ZHAO P X, CAI Z S, ZHANG X J, et al. Hydrogen attenuates inflammation by inducing early M2 macrophage polarization in skin wound healing[J]. Pharmaceuticals (Basel), 2023, 16(6): 885. |
| [16] | RUNGRATANAWANICH W, QU Y, WANG X, et al. Advanced glycation end products (AGEs) and other adducts in aging-related diseases and alcohol-mediated tissue injury[J]. Exp Mol Med, 2021, 53(2): 168-188. |
| [17] | WONG S L, DEMERS M, MARTINOD K, et al. Diabetes primes neutrophils to undergo NETosis, which impairs wound healing[J]. Nat Med, 2015, 21(7): 815-819. |
| [18] | SONG J Y, ZHU K Y, WANG H P, et al. Deciphering the emerging role of programmed cell death in diabetic wound healing[J]. Int J Biol Sci, 2023, 19(15): 4989-5003. |
| [19] | LIU Y, LI Z N, LI W D, et al. Discovery of β-sitosterol's effects on molecular changes in rat diabetic wounds and its impact on angiogenesis and macrophages[J]. Int Immunopharmacol, 2024, 126: 111283. |
| [20] | ZHANG X Y, WU Y, GONG H, et al. A multifunctional herb-derived glycopeptide hydrogel for chronic wound healing[J]. Small, 2024, 20(36): e2400516. |
| [21] | ZHANG F X, SHAN S, FU C L, et al. Advanced mass spectrometry-based biomarker identification for metabolomics of diabetes mellitus and its complications[J]. Molecules, 2024, 29(11): 2530. |
| [22] | VAN DEN BOSSCHE J, BAARDMAN J, OTTO N A, et al. Mitochondrial dysfunction prevents repolarization of inflammatory macrophages[J]. Cell Rep, 2016, 17(3): 684-696. |
| [23] | PILLON N J, LOOS R J F, MARSHALL S M, et al. Metabolic consequences of obesity and type 2 diabetes: balancing genes and environment for personalized care[J]. Cell, 2021, 184(6): 1530-1544. |
| [24] | RUSSO S, KWIATKOWSKI M, GOVORUKHINA N, et al. Meta-inflammation and metabolic reprogramming of macrophages in diabetes and obesity: the importance of metabolites[J]. Front Immunol, 2021, 12: 746151. |
| [25] | EMING S A, MURRAY P J, PEARCE E J. Metabolic orchestration of the wound healing response[J]. Cell Metab, 2021, 33(9): 1726-1743. |
| [26] | MOUTON A J, LI X, HALL M E, et al. Obesity, hypertension, and cardiac dysfunction: novel roles of immunometabolism in macrophage activation and inflammation[J]. Circ Res, 2020, 126(6): 789-806. |
| [27] | BOUTENS L, HOOIVELD G J, DHINGRA S, et al. Unique metabolic activation of adipose tissue macrophages in obesity promotes inflammatory responses[J]. Diabetologia, 2018, 61(4): 942-953. |
| [28] | HE X T, LI X, ZHANG M, et al. Role of molybdenum in material immunomodulation and periodontal wound healing: targeting immunometabolism and mitochondrial function for macrophage modulation[J]. Biomaterials, 2022, 283: 121439. |
| [29] | WILLENBORG S, SANIN D E, JAIS A, et al. Mitochondrial metabolism coordinates stage-specific repair processes in macrophages during wound healing[J]. Cell Metab, 2021, 33(12): 2398-2414.e9. |
| [30] | ZHANG D, TANG Z Y, HUANG H, et al. Metabolic regulation of gene expression by histone lactylation[J]. Nature, 2019, 574(7779): 575-580. |
| [31] | KOTWAL G J, CHIEN S F. Macrophage differentiation in normal and accelerated wound healing[J]. Results Probl Cell Differ, 2017, 62: 353-364. |
| [32] | HUANG F, LU X Y, YANG Y, et al. Microenvironment-based diabetic foot ulcer nanomedicine[J]. Adv Sci (Weinh), 2023, 10(2): e2203308. |
| [33] | LIN C W, HUNG C M, CHEN W J, et al. New horizons of macrophage immunomodulation in the healing of diabetic foot ulcers[J]. Pharmaceutics, 2022, 14(10): 2065. |
| [34] | YAO Y M, ZHANG H. Better therapy for combat injury[J]. Mil Med Res, 2019, 6(1): 23. |
| [35] | LI Q H, SONG H J, LI S Y, et al. Macrophage metabolism reprogramming EGCG-Cu coordination capsules delivered in polyzwitterionic hydrogel for burn wound healing and regeneration[J]. Bioact Mater, 2023, 29: 251-264. |
| [36] | ZHANG K, LU W C, ZHANG M, et al. Reducing host aldose reductase activity promotes neuronal differentiation of transplanted neural stem cells at spinal cord injury sites and facilitates locomotion recovery[J]. Neural Regen Res, 2022, 17(8): 1814-1820. |
| [37] | HE J B, ZHOU S S, WANG J X, et al. Anti-inflammatory and anti-oxidative electrospun nanofiber membrane promotes diabetic wound healing via macrophage modulation[J]. J Nanobiotechnology, 2024, 22(1): 116. |
| [38] | BATISTA-GONZALEZ A, VIDAL R, CRIOLLO A, et al. New insights on the role of lipid metabolism in the metabolic reprogramming of macrophages[J]. Front Immunol, 2020, 10: 2993. |
| [39] | LEE J H, PHELAN P, SHIN M, et al. SREBP-1a-stimulated lipid synthesis is required for macrophage phagocytosis downstream of TLR4-directed mTORC1[J]. Proc Natl Acad Sci USA, 2018, 115(52): E12228-E12234. |
| [40] | VASSILIOU E, FARIAS-PEREIRA R. Impact of lipid metabolism on macrophage polarization: implications for inflammation and tumor immunity[J]. Int J Mol Sci, 2023, 24(15): 12032. |
| [41] | SHOOK B A, WASKO R R, MANO O, et al. Dermal adipocyte lipolysis and myofibroblast conversion are required for efficient skin repair[J]. Cell Stem Cell, 2020, 26(6): 880-895.e6. |
| [42] | COOPER P O, KLEB S S, NOONEPALLE S K, et al. G-protein-coupled receptor 84 regulates acute inflammation in normal and diabetic skin wounds[J]. Cell Rep, 2024, 43(6): 114288. |
| [43] | JETTEN N, ROUMANS N, GIJBELS M J, et al. Wound administration of M2-polarized macrophages does not improve murine cutaneous healing responses[J]. PLoS One, 2014, 9(7): e102994. |
| [44] | PERCIVAL S L, MCCARTY S, HUNT J A, et al. The effects of pH on wound healing, biofilms, and antimicrobial efficacy[J]. Wound Repair Regen, 2014, 22(2): 174-186. |
| [45] | OLONA A, HATELEY C, MURALIDHARAN S, et al. Sphingolipid metabolism during toll-like receptor 4 (TLR4)-mediated macrophage activation[J]. Br J Pharmacol, 2021, 178(23): 4575-4587. |
| [46] | HE L, WEBER K J, SCHILLING J D. Glutamine modulates macrophage lipotoxicity[J]. Nutrients, 2016, 8(4): 215. |
| [47] | PAN Y, HUI X Y, HOO R L C, et al. Adipocyte-secreted exosomal microRNA-34a inhibits M2 macrophage polarization to promote obesity-induced adipose inflammation[J]. J Clin Invest, 2019, 129(2): 834-849. |
| [48] | CHI Z X, CHEN S, YANG D H, et al. Gasdermin D-mediated metabolic crosstalk promotes tissue repair[J]. Nature, 2024, 634(8036): 1168-1177. |
| [49] | DEBATS I G, WOLFS T M, GOTOH T, et al. Role of arginine in superficial wound healing in man[J]. Nitric Oxide, 2009, 21(3/4): 175-183. |
| [50] | ITO D, ITO H, IDETA T, et al. Systemic and topical administration of spermidine accelerates skin wound healing[J]. Cell Commun Signal, 2021, 19(1): 36. |
| [51] | ARRIBAS-LÓPEZ E, ZAND N, OJO O, et al. The effect of amino acids on wound healing: a systematic review and meta-analysis on arginine and glutamine[J]. Nutrients, 2021, 13(8): 2498. |
| [52] | LIU Y, SHI J P, XIONG W, et al. Production of an animal model of semi-Yin and semi-Yang syndrome with diabetic ulcers and study of its pathological and metabolic features[J]. Evid Based Complement Alternat Med, 2021, 2021: 6345147. |
| [53] | MANCHANDA M, TORRES M, INUOSSA F, et al. Metabolic reprogramming and reliance in human skin wound healing[J]. J Invest Dermatol, 2023, 143(10): 2039-2051.e10. |
| [54] | REN W K, XIA Y Y, CHEN S Y, et al. Glutamine metabolism in macrophages: a novel target for obesity/type 2 diabetes[J]. Adv Nutr, 2019, 10(2): 321-330. |
| [55] | LV D M, CAO X L, ZHONG L, et al. Targeting phenylpyruvate restrains excessive NLRP3 inflammasome activation and pathological inflammation in diabetic wound healing[J]. Cell Rep Med, 2023, 4(8): 101129. |
| [56] | ZHAO M N, WANG K Y, LIN R, et al. Influence of glutamine metabolism on diabetes development: a scientometric review[J]. Heliyon, 2024, 10(4): e25258. |
| [57] | GIESBERTZ P, DANIEL H. Branched-chain amino acids as biomarkers in diabetes[J]. Curr Opin Clin Nutr Metab Care, 2016, 19(1): 48-54. |
| [58] | GAN Z D, GUO Y, ZHAO M Y, et al. Excitatory amino acid transporter supports inflammatory macrophage responses[J]. Sci Bull (Beijing), 2024, 69(15): 2405-2419. |
| [59] | YAN J L, TIE G D, WANG S Y, et al. Diabetes impairs wound healing by Dnmt1-dependent dysregulation of hematopoietic stem cells differentiation towards macrophages[J]. Nat Commun, 2018, 9(1): 33. |
| [60] | HOU Y X, WEI D, ZHANG Z Q, et al. Downregulation of nutrition sensor GCN2 in macrophages contributes to poor wound healing in diabetes[J]. Cell Rep, 2024, 43(1): 113658. |
| [61] | ZHANG Q Z, CHEN S Y, GUO Y, et al. Phenylalanine diminishes M1 macrophage inflammation[J]. Sci China Life Sci, 2023, 66(12): 2862-2876. |
| [62] | ZHU H T, XING C, DOU X Q, et al. Chiral hydrogel accelerates re-epithelization in chronic wounds via mechanoregulation[J]. Adv Healthc Mater, 2022, 11(21): e2201032. |
| [63] | MIAO M Y, NIU Y W, XIE T, et al. Diabetes-impaired wound healing and altered macrophage activation: a possible pathophysiologic correlation[J]. Wound Repair Regen, 2012, 20(2): 203-213. |
| [64] | CHEN M, CHANG C, LEVIAN B, et al. Why are there so few FDA-approved therapeutics for wound healing?[J]. Int J Mol Sci, 2023, 24(20): 15109. |
| [65] | DA PORTO A, MIRANDA C, BROSOLO G, et al. Nutritional supplementation on wound healing in diabetic foot: what is known and what is new?[J]. World J Diabetes, 2022, 13(11): 940-948. |
| [1] | 朱子俊, 钱逸斐, 李倩玉, 李松玲, 覃雯莉, 刘艳丰. 后期促进复合体亚基10调控PI3K-AKT-mTOR通路促进肝细胞癌进展的研究[J]. 上海交通大学学报(医学版), 2025, 45(9): 1171-1182. |
| [2] | 杨全军, 柏丁源, 周雨萱, 白露, 郭澄. 异柠檬酸脱氢酶1突变介导D-2-羟基戊二酸代谢重编程在肿瘤免疫调控中的作用及相关药物研发进展[J]. 上海交通大学学报(医学版), 2025, 45(9): 1239-1248. |
| [3] | 黄昕, 刘家辉, 叶敬文, 钱文莉, 许万星, 王琳. 基于机器学习的小细胞肺癌代谢分子诊断模型的建立和临床应用[J]. 上海交通大学学报(医学版), 2025, 45(8): 1009-1016. |
| [4] | 姜芊羽, 姚程程, 季萍, 王颖. HAMA水凝胶促进皮肤创面愈合的组织局部微环境特征[J]. 上海交通大学学报(医学版), 2025, 45(8): 969-980. |
| [5] | 王琳, 徐萍, 张乔婷, 田军, 娄晓丽, 王静. 胱天蛋白酶募集域蛋白9在重症急性胰腺炎巨噬细胞M1极化中的作用[J]. 上海交通大学学报(医学版), 2025, 45(8): 981-989. |
| [6] | 赛提尔古丽·克然木, 钱蕾, 丁思怡, 哈娜提·马合力木汗, 杨雪儿, 贾浩. 精氨酸代谢调控间充质干细胞功能的研究进展[J]. 上海交通大学学报(医学版), 2025, 45(7): 910-915. |
| [7] | 宋静, 姜烁, 万方煜, 李娟, 艾迪娜·木合塔, 闵新颖, 周婧琪. 膳食模式干预对代谢相关脂肪性肝病的影响与机制研究进展[J]. 上海交通大学学报(医学版), 2025, 45(7): 926-933. |
| [8] | 韩龙传, 李悦, 邹智慧, 罗静, 李若伊, 张颖婷, 唐欣欣, 田丽红, 陆宇恒, 黄莺, 贺明, 付寅坤. 磷脂酰乙醇胺引起内质网应激促进巨噬细胞衰老及肝损伤[J]. 上海交通大学学报(医学版), 2025, 45(6): 693-704. |
| [9] | 汤开然, 冯成领, 韩邦旻. 基于单细胞测序与转录组测序构建M2巨噬细胞基因相关的前列腺癌预后模型[J]. 上海交通大学学报(医学版), 2025, 45(5): 549-561. |
| [10] | 倪书奕, 姜钊, 汪中涛, 何树梅. 红景天苷对卡介苗感染的巨噬细胞免疫功能的影响[J]. 上海交通大学学报(医学版), 2025, 45(4): 426-433. |
| [11] | 连明珠, 张常晓, 盛凯, 郭梦, 方姝予. 老年营养风险指数对住院老年2型糖尿病患者发生肺部感染的预测价值[J]. 上海交通大学学报(医学版), 2025, 45(4): 452-458. |
| [12] | 邹沛辰, 刘鸿宇, 阿衣娜扎尔·艾合买提, 朱亮, 唐亚斌, 雷绘敏. 索托拉西布获得性耐药肺癌细胞的代谢轮廓分析[J]. 上海交通大学学报(医学版), 2025, 45(2): 138-149. |
| [13] | 马秀珍, 周妮, 郭思琪, 王源媛, 麦平. 大麻素受体1通过Gαi/o/RhoA信号通路促进急性肺损伤小鼠巨噬细胞M1极化[J]. 上海交通大学学报(医学版), 2025, 45(2): 161-168. |
| [14] | 林祎嘉, 程丽珍, 胡廷军, 苗雅. 基于孟德尔随机化法的2型糖尿病与认知障碍因果关系研究[J]. 上海交通大学学报(医学版), 2025, 45(2): 204-210. |
| [15] | 陆佳萍, 刘醒, 张林杉, 赵琳, 张敏, 李小英, 刘玥隽. 腹部脂肪面积与2型糖尿病患者胰岛β细胞第一时相分泌功能的关系[J]. 上海交通大学学报(医学版), 2025, 45(1): 42-50. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||