
Journal of Shanghai Jiao Tong University (Medical Science) ›› 2022, Vol. 42 ›› Issue (9): 1336-1346.doi: 10.3969/j.issn.1674-8115.2022.09.022
• Public health • Previous Articles Next Articles
WANG Jie1,2( ), WU Hui3(
), WU Hui3( ), LU Lingpeng4, YANG Kefeng1,2,5, ZHU Jie6, ZHOU Hengyi1,2, YAO Die1,2, GAO Ya1,2, FENG Yuting1,2, LIU Yuhong7(
), LU Lingpeng4, YANG Kefeng1,2,5, ZHU Jie6, ZHOU Hengyi1,2, YAO Die1,2, GAO Ya1,2, FENG Yuting1,2, LIU Yuhong7( ), JIA Jie1,2,5(
), JIA Jie1,2,5( )
)
Received:2022-05-18
Accepted:2022-08-19
Online:2022-09-28
Published:2022-09-28
Contact:
LIU Yuhong,JIA Jie
E-mail:wangjie_1111@alumni.sjtu.edu.cn;liuyuhong0121@126.com;jie.jia@shsmu.edu.cn
Supported by:CLC Number:
WANG Jie, WU Hui, LU Lingpeng, YANG Kefeng, ZHU Jie, ZHOU Hengyi, YAO Die, GAO Ya, FENG Yuting, LIU Yuhong, JIA Jie. Dynamic changes in gut microbiota of women with gestational diabetes mellitus and the correlation with blood glucose, blood lipid and diet[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2022, 42(9): 1336-1346.
Add to citation manager EndNote|Ris|BibTeX
URL: https://xuebao.shsmu.edu.cn/EN/10.3969/j.issn.1674-8115.2022.09.022
| Item | GDM group (n=30) | Control group (n=48) | P value |
|---|---|---|---|
| Age/year | 29.90±4.21 | 28.90±4.15 | 0.304 |
| Pre-pregnancy BMI/(kg·m-2) | 23.01 (20.36, 24.92) | 21.20 (19.31, 23,73) | 0.216 |
| Weight gain/kg | 15.74±4.80 | 12.63±5.77 | 0.012 |
| Gravidity/n (%) | 0.777 | ||
| 1 | 14 (46.67) | 24 (50.00) | |
| 2 | 7 (23.33) | 13 (27.08) | |
| ≥3 | 9 (30.00) | 11 (22.92) | |
| Parity/n (%) | 0.277 | ||
| Nulliparous | 15 (50.00) | 30 (62.50) | |
| Multiparous | 15 (50.00) | 18 (37.50) | |
| Educational background/n (%) | 0.901 | ||
| Middle school or below | 5 (16.67) | 7 (14.58) | |
| High school | 6 (20.00) | 8 (16.67) | |
| College | 17 (56.67) | 31 (64.58) | |
| Graduate or above | 2 (6.67) | 2 (4.17) | |
| FBG/(mmol·L-1) | 5.00±0.57 | 4.35±0.22 | 0.000 |
| Blood glucose level at OGTT/(mmol·L-1) | |||
| 1 h | 10.01±1.62 | 7.29±1.41 | 0.000 |
| 2 h | 7.75±1.80 | 6.07±0.90 | 0.000 |
| TC/(mmol·L-1) | 5.27±0.85 | 5.54±1.03 | 0.239 |
| TAG/(mmol·L-1) | 3.00±1.32 | 2.12±0.67 | 0.003 |
| HDL/(mmol·L-1) | 1.83±0.28 | 2.00±0.28 | 0.014 |
| LDL/(mmol·L-1) | 2.67±0.65 | 3.07±0.90 | 0.040 |
Tab 1 Comparison of demographic information and blood biochemical indicators between the GDM group and control group
| Item | GDM group (n=30) | Control group (n=48) | P value |
|---|---|---|---|
| Age/year | 29.90±4.21 | 28.90±4.15 | 0.304 |
| Pre-pregnancy BMI/(kg·m-2) | 23.01 (20.36, 24.92) | 21.20 (19.31, 23,73) | 0.216 |
| Weight gain/kg | 15.74±4.80 | 12.63±5.77 | 0.012 |
| Gravidity/n (%) | 0.777 | ||
| 1 | 14 (46.67) | 24 (50.00) | |
| 2 | 7 (23.33) | 13 (27.08) | |
| ≥3 | 9 (30.00) | 11 (22.92) | |
| Parity/n (%) | 0.277 | ||
| Nulliparous | 15 (50.00) | 30 (62.50) | |
| Multiparous | 15 (50.00) | 18 (37.50) | |
| Educational background/n (%) | 0.901 | ||
| Middle school or below | 5 (16.67) | 7 (14.58) | |
| High school | 6 (20.00) | 8 (16.67) | |
| College | 17 (56.67) | 31 (64.58) | |
| Graduate or above | 2 (6.67) | 2 (4.17) | |
| FBG/(mmol·L-1) | 5.00±0.57 | 4.35±0.22 | 0.000 |
| Blood glucose level at OGTT/(mmol·L-1) | |||
| 1 h | 10.01±1.62 | 7.29±1.41 | 0.000 |
| 2 h | 7.75±1.80 | 6.07±0.90 | 0.000 |
| TC/(mmol·L-1) | 5.27±0.85 | 5.54±1.03 | 0.239 |
| TAG/(mmol·L-1) | 3.00±1.32 | 2.12±0.67 | 0.003 |
| HDL/(mmol·L-1) | 1.83±0.28 | 2.00±0.28 | 0.014 |
| LDL/(mmol·L-1) | 2.67±0.65 | 3.07±0.90 | 0.040 |
| Item | GDM group (n=30) | Control group (n=48) | P value |
|---|---|---|---|
| Nutrient intake | |||
| Energy/(J·d-1) | 6 425 408.09 (5 415 822.49, 8 290 414.36) | 6 510 632.03 (5 251 444.09, 7 870 154.84) | 0.475 |
| Protein/(g·d-1) | 59.20 (51.30, 77.50) | 59.70 (47.15, 71.60) | 0.853 |
| Fat/(g·d-1) | 49.40 (34.50, 55.10) | 34.90 (26.10, 47.10) | 0.046 |
| Carbohydrate/(g·d-1) | 197.40 (178.10, 268.00) | 211.80 (184.20, 249.20) | 0.951 |
| Fiber/(g·d-1) | 16.60 (14.40, 21.70) | 17.00 (13.20, 21.80) | 0.622 |
| BCAA/(mg·d-1) | 6 340.50 (5 417.60, 7 442.50) | 5 952.00 (4 212.35, 7 364.00) | 0.983 |
| PUFA/(g·d-1) | 6.90 (2.50, 8.90) | 4.30 (2.70, 6.80) | 0.363 |
| MUFA/(g·d-1) | 5.70 (4.30, 7.90) | 4.90 (3.10, 7.30) | 0.317 |
| SFA/(g·d-1) | 7.60 (5.50, 8.60) | 7.20 (5.65, 8.70) | 0.914 |
| Food intake/(g·d-1) | |||
| Staple | 165.40 (140.70, 196.20) | 179.00 (128.60, 251.25) | 0.593 |
| Vegetable | 437.60 (335.90, 779.00) | 639.30 (445.80, 819.10) | 0.072 |
| Fruit | 506.70 (394.80, 628.60) | 437.10 (294.30, 646.40) | 0.319 |
| Egg | 60.00 (30.00, 64.00) | 60.00 (38.60, 90.00) | 0.374 |
| Meat | 50.10 (34.30, 67.10) | 35.70 (21.50, 56.00) | 0.111 |
| Fish | 41.40 (13.00, 78.60) | 42.90 (28.25, 78.60) | 0.583 |
| Bean | 77.70 (21.40, 131.40) | 50.00 (22.60, 97.60) | 0.655 |
| Dairy | 271.40 (200.00, 320.00) | 250.00 (188.00, 305.95) | 0.701 |
| Dried fruit | 16.00 (6.40, 30.00) | 14.30 (3.80, 20.00) | 0.318 |
Tab 2 Comparison of dietary intake between the GDM group and control group
| Item | GDM group (n=30) | Control group (n=48) | P value |
|---|---|---|---|
| Nutrient intake | |||
| Energy/(J·d-1) | 6 425 408.09 (5 415 822.49, 8 290 414.36) | 6 510 632.03 (5 251 444.09, 7 870 154.84) | 0.475 |
| Protein/(g·d-1) | 59.20 (51.30, 77.50) | 59.70 (47.15, 71.60) | 0.853 |
| Fat/(g·d-1) | 49.40 (34.50, 55.10) | 34.90 (26.10, 47.10) | 0.046 |
| Carbohydrate/(g·d-1) | 197.40 (178.10, 268.00) | 211.80 (184.20, 249.20) | 0.951 |
| Fiber/(g·d-1) | 16.60 (14.40, 21.70) | 17.00 (13.20, 21.80) | 0.622 |
| BCAA/(mg·d-1) | 6 340.50 (5 417.60, 7 442.50) | 5 952.00 (4 212.35, 7 364.00) | 0.983 |
| PUFA/(g·d-1) | 6.90 (2.50, 8.90) | 4.30 (2.70, 6.80) | 0.363 |
| MUFA/(g·d-1) | 5.70 (4.30, 7.90) | 4.90 (3.10, 7.30) | 0.317 |
| SFA/(g·d-1) | 7.60 (5.50, 8.60) | 7.20 (5.65, 8.70) | 0.914 |
| Food intake/(g·d-1) | |||
| Staple | 165.40 (140.70, 196.20) | 179.00 (128.60, 251.25) | 0.593 |
| Vegetable | 437.60 (335.90, 779.00) | 639.30 (445.80, 819.10) | 0.072 |
| Fruit | 506.70 (394.80, 628.60) | 437.10 (294.30, 646.40) | 0.319 |
| Egg | 60.00 (30.00, 64.00) | 60.00 (38.60, 90.00) | 0.374 |
| Meat | 50.10 (34.30, 67.10) | 35.70 (21.50, 56.00) | 0.111 |
| Fish | 41.40 (13.00, 78.60) | 42.90 (28.25, 78.60) | 0.583 |
| Bean | 77.70 (21.40, 131.40) | 50.00 (22.60, 97.60) | 0.655 |
| Dairy | 271.40 (200.00, 320.00) | 250.00 (188.00, 305.95) | 0.701 |
| Dried fruit | 16.00 (6.40, 30.00) | 14.30 (3.80, 20.00) | 0.318 |
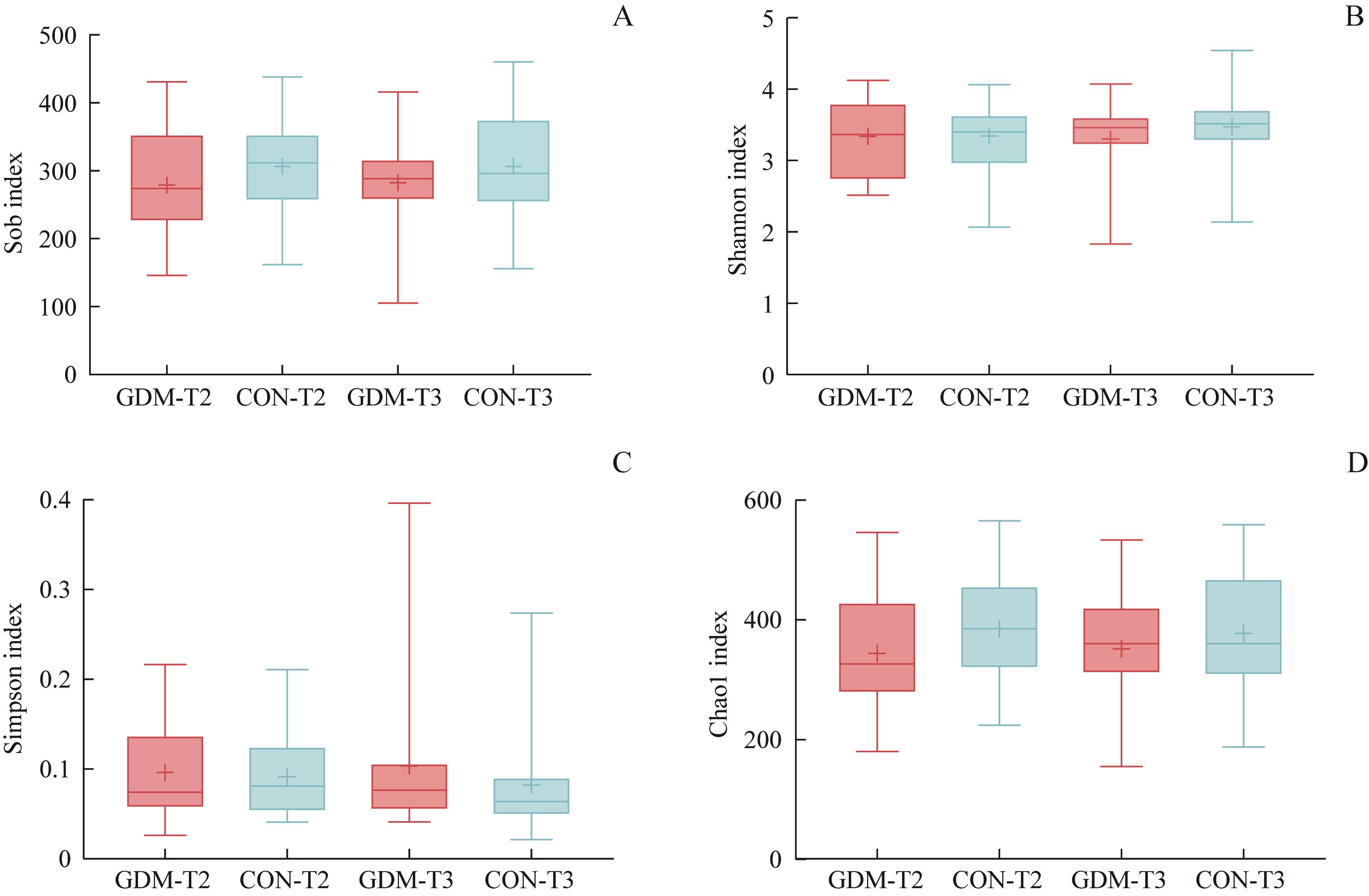
Fig 1 Comparison of gut bacterial α-diversity between the GDM group and control group in the second trimester (T2) and the third trimester (T3) of pregnancy
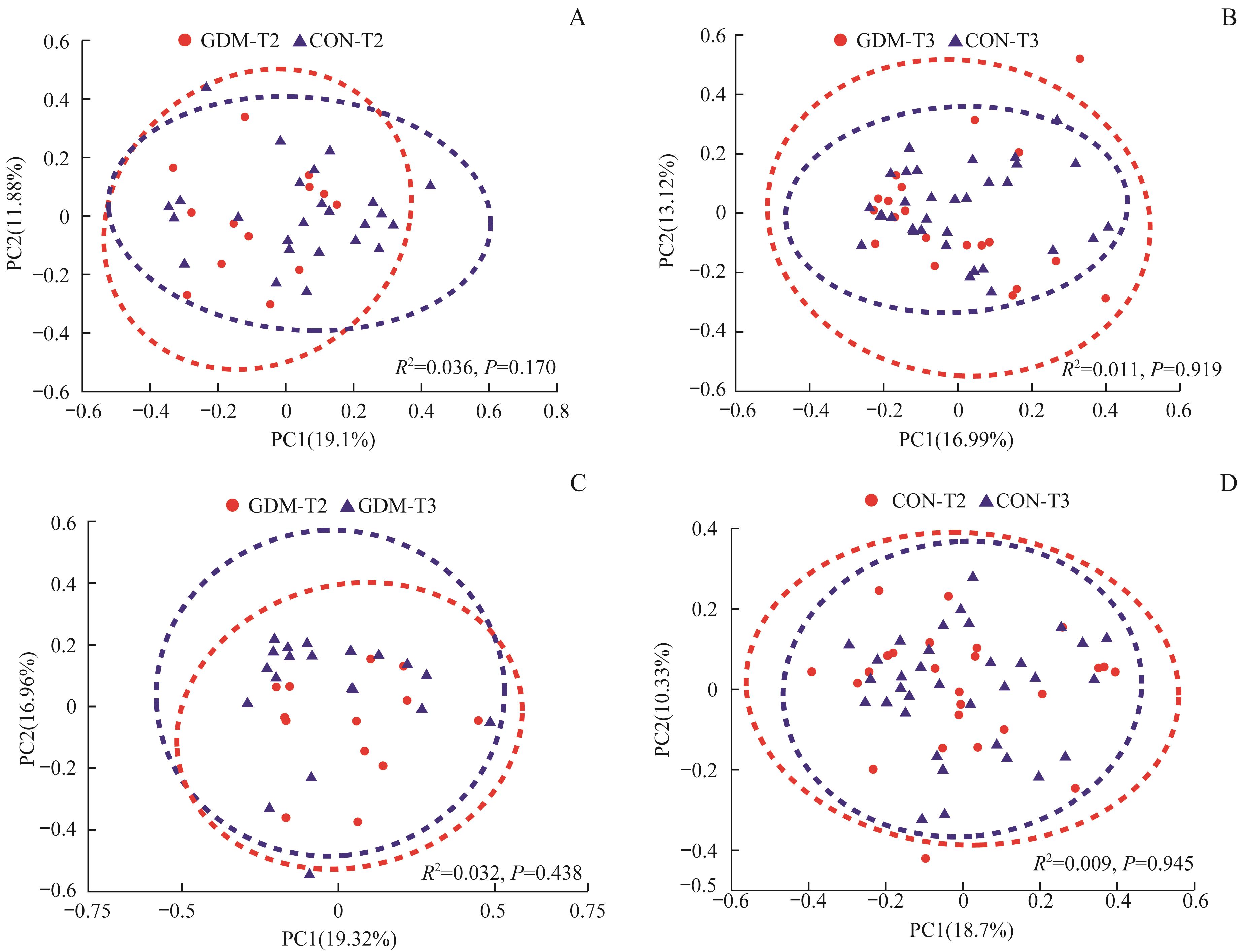
Fig 2 Comparison of gut bacterial β-diversity between the GDM group and control group in the second trimester (T2) and the third trimester (T3) of pregnancy
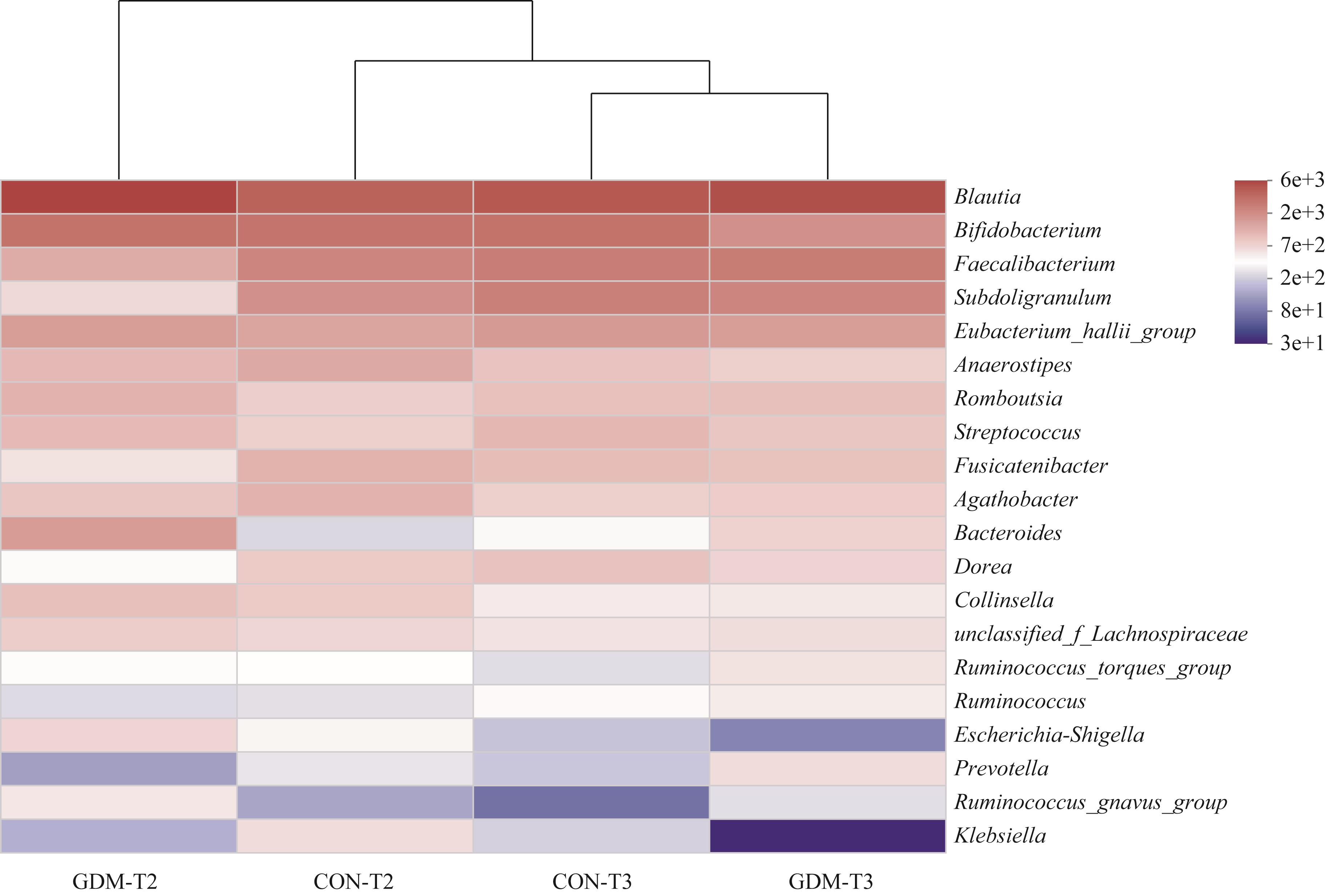
Fig 3 Heatmap clustering analysis of the top 20 gut bacterial genera in the women of the two groups in the second trimester (T2) and the third trimester (T3) of pregnancy

Fig 4 Difference test of the top 20 gut bacterial genera in the women of the two groups in the second trimester (T2) and the third trimester (T3) of pregnancy
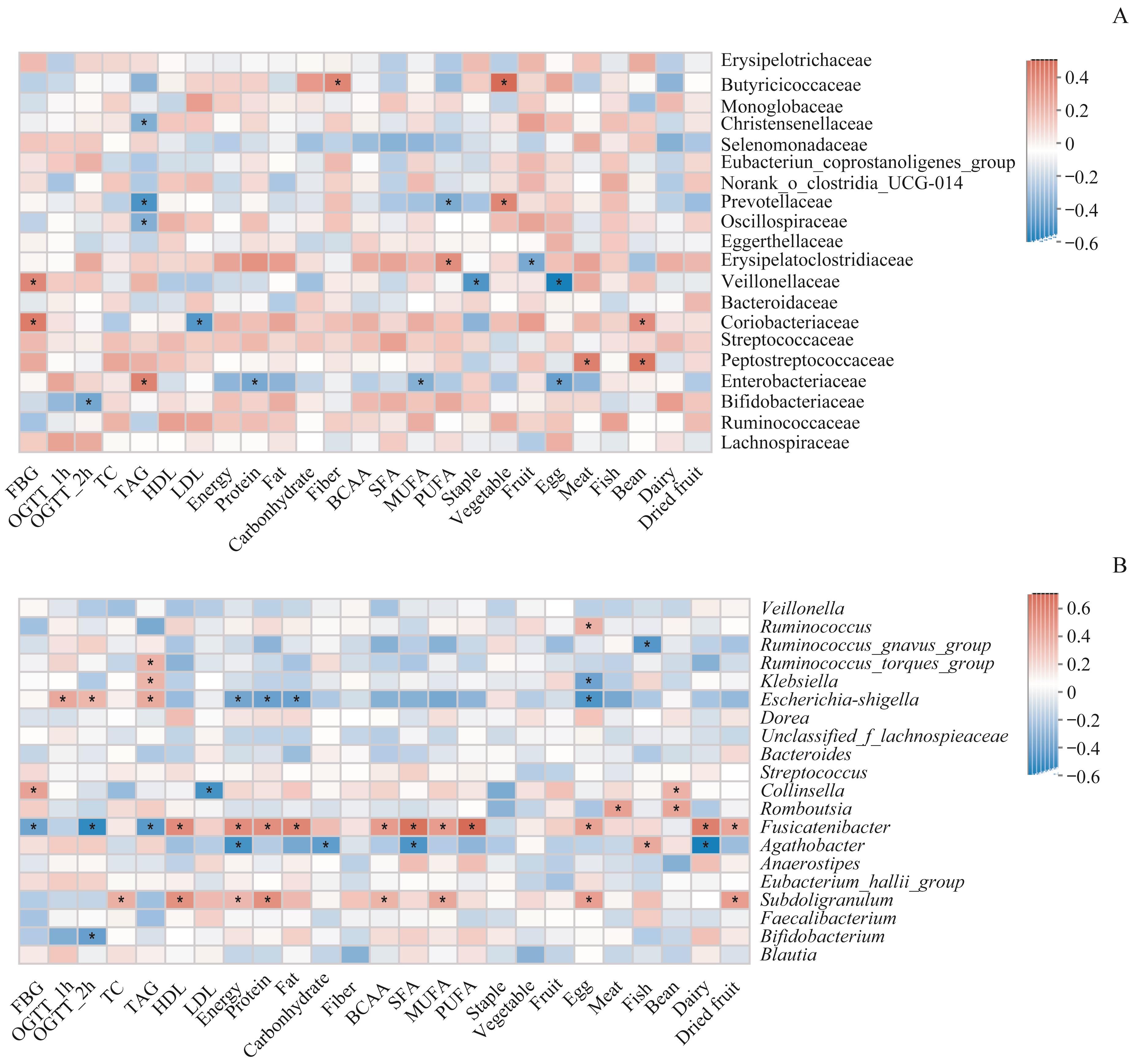
Fig 6 Spearman correlation analysis between the environmental factors and the family level (A) and the genus level (B) of the gut microbiota (top 20) of the pregnant women in the second trimester (T2) of pregnancy
| 1 | American Diabetes Association. Diagnosis and classification of diabetes mellitus[J]. Diabetes Care, 2010, 33(Suppl 1): S62-69. |
| 2 | ZHU Y Y, ZHANG C L. Prevalence of gestational diabetes and risk of progression to type 2 diabetes: a global perspective[J]. Curr Diab Rep, 2016, 16(1): 7. |
| 3 | GAO C H, SUN X, LU L, et al. Prevalence of gestational diabetes mellitus in mainland China: a systematic review and meta-analysis[J]. J Diabetes Investig, 2019, 10(1): 154-162. |
| 4 | DALY B, TOULIS K A, THOMAS N, et al. Increased risk of ischemic heart disease, hypertension, and type 2 diabetes in women with previous gestational diabetes mellitus, a target group in general practice for preventive interventions: a population-based cohort study[J]. PLoS Med, 2018, 15(1): e1002488. |
| 5 | MAHAJAN A, DONOVAN L E, VALLEE R, et al. Evidenced-based nutrition for gestational diabetes mellitus[J]. Curr Diab Rep, 2019, 19(10): 94. |
| 6 | ARRIETA M C, STIEMSMA L T, DIMITRIU P A, et al. Early infancy microbial and metabolic alterations affect risk of childhood asthma[J]. Sci Transl Med, 2015, 7(307): 307ra152. |
| 7 | STANISLAWSKI M A, DABELEA D, WAGNER B D, et al. Gut microbiota in the first 2 years of life and the association with body mass index at age 12 in a Norwegian birth cohort[J]. mBio, 2018, 9(5): e01751-e01718. |
| 8 | CRUSELL M K W, HANSEN T H, NIELSEN T, et al. Gestational diabetes is associated with change in the gut microbiota composition in third trimester of pregnancy and postpartum[J]. Microbiome, 2018, 6(1): 89. |
| 9 | ZHENG W, XU Q, HUANG W Y, et al. Gestational diabetes mellitus is associated with reduced dynamics of gut microbiota during the first half of pregnancy[J]. mSystems, 2020, 5(2): e00109-e00120. |
| 10 | WANG J F, ZHENG J Y, SHI W Y, et al. Dysbiosis of maternal and neonatal microbiota associated with gestational diabetes mellitus[J]. Gut, 2018, 67(9): 1614-1625. |
| 11 | HUANG L L, THONUSIN C, CHATTIPAKORN N, et al. Impacts of gut microbiota on gestational diabetes mellitus: a comprehensive review[J]. Eur J Nutr, 2021, 60(5): 2343-2360. |
| 12 | ROLD L S, BUNDGAARD-NIELSEN C, NIEMANN HOLM-JACOBSEN J, et al. Characteristics of the gut microbiome in women with gestational diabetes mellitus: a systematic review[J]. PLoS One, 2022, 17(1): e0262618. |
| 13 | 中华医学会妇产科学分会产科学组, 中华医学会围产医学分会妊娠合并糖尿病协作组. 妊娠合并糖尿病诊治指南(2014)[J]. 中华妇产科杂志, 2014, 49(8): 561-569. |
| Obstetrics Group of Obsterics and Gynecology Branch of Chinese Medical Association, Gestational Diabetes Mellitus Collaborative Group of Perinatal Medical Branch of Chinese Medical Association. Guidelines for diagnosis and treatment of pregnancy associated with diabetes[J]. Chin J Obstet Gynecol, 2014, 49(8): 561-569. | |
| 14 | 王蓓, 沈丽蔚, 周丽莉, 等. 孕期胆碱摄入及母婴体内胆碱代谢水平的相关性[J]. 中华围产医学杂志, 2017, 20(11): 790-795. |
| WANG B, SHEN L W, ZHOU L L, et al. Association between choline intake during pregnancy and choline metabolism in parturients and infants[J]. Chin J Perinat Med, 2017, 20(11): 790-795. | |
| 15 | JIA J, XUN P C, WANG X L, et al. Impact of postnatal antibiotics and parenteral nutrition on the gut microbiota in preterm infants during early life[J]. JPEN J Parenter Enteral Nutr, 2020, 44(4): 639-654. |
| 16 | CORTEZ R V, TADDEI C R, SPARVOLI L G, et al. Microbiome and its relation to gestational diabetes[J]. Endocrine, 2019, 64(2): 254-264. |
| 17 | FERROCINO I, PONZO V, GAMBINO R, et al. Changes in the gut microbiota composition during pregnancy in patients with gestational diabetes mellitus (GDM)[J]. Sci Rep, 2018, 8(1): 12216. |
| 18 | MEDICI DUALIB P, OGASSAVARA J, MATTAR R, et al. Gut microbiota and gestational diabetes mellitus: a systematic review[J]. Diabetes Res Clin Pract, 2021, 180: 109078. |
| 19 | LIU H, PAN L L, LV S T, et al. Alterations of gut microbiota and blood lipidome in gestational diabetes mellitus with hyperlipidemia[J]. Front Physiol, 2019, 10: 1015. |
| 20 | TAN J, MCKENZIE C, POTAMITIS M, et al. The role of short-chain fatty acids in health and disease[J]. Adv Immunol, 2014, 121: 91-119. |
| 21 | VITAL M, KARCH A, PIEPER D H. Colonic butyrate-producing communities in humans: an overview using omics data[J]. mSystems, 2017, 2(6): e00130-e00117. |
| 22 | ZHANG X Y, SHEN D Q, FANG Z W, et al. Human gut microbiota changes reveal the progression of glucose intolerance[J]. PLoS One, 2013, 8(8): e71108. |
| 23 | BORGO F, GARBOSSA S, RIVA A, et al. Body mass index and sex affect diverse microbial niches within the gut[J]. Front Microbiol, 2018, 9: 213. |
| 24 | STRAUB T J, CHOU W C, MANSON A L, et al. Limited effects of long-term daily cranberry consumption on the gut microbiome in a placebo-controlled study of women with recurrent urinary tract infections[J]. BMC Microbiol, 2021, 21(1): 53. |
| 25 | MANCO M, PUTIGNANI L, BOTTAZZO G F. Gut microbiota, lipopolysaccharides, and innate immunity in the pathogenesis of obesity and cardiovascular risk[J]. Endocr Rev, 2010, 31(6): 817-844. |
| 26 | CANI P D, NEYRINCK A M, FAVA F, et al. Selective increases of bifidobacteria in gut microflora improve high-fat-diet-induced diabetes in mice through a mechanism associated with endotoxaemia[J]. Diabetologia, 2007, 50(11): 2374-2383. |
| [1] | SONG Jing, JIANG Shuo, WAN Fangyu, LI Juan, MUHETA Adina, MIN Xinying, ZHOU Jingqi. Research progress in effects and mechanisms of dietary pattern interventions in metabolic associated fatty liver disease [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2025, 45(7): 926-933. |
| [2] | CHEN Shentse, CHEN Yiming, WANG Fan, ZHANG Mengke, YANG Weichieh, LÜ Dongbin, HONG Wu. Advances in dietary interventions for the treatment of depression-related symptoms [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2024, 44(8): 1050-1055. |
| [3] | LU Xingyu, XU Yidan, LIU Yiqin, ZHANG Qianren, DONG Yan. Effect of high-fat diet on adipose tissues structure and inflammatory characteristics during pregnancy in mice [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2024, 44(8): 981-990. |
| [4] | DU Yage, LU Yanhui, AN Yu, SONG Ying, ZHENG Jie. Research progress in mechanisms of gut microbiota in diabetic cognitive impairment and its targeted intervention [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2024, 44(4): 494-500. |
| [5] | YANG Ruijun, LÜ Shuhong, LIU Zhiye, ZHANG Xin, LIU Zhihao. Relationship of screen time and dietary behaviors with depressive symptoms in junior high school students in five provinces in China [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2024, 44(3): 358-364. |
| [6] | MA Jinqian, FAN Pianpian, ZHENG Tao, ZHANG Lin, CHEN Yuanzhi, SHEN Jian, OUYANG Fengxiu. Relationship among maternal gut, vaginal microbiota and microbiota in meconium and vernix caseosa in newborns [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2024, 44(1): 50-63. |
| [7] | GAO Yu, YIN Shan, PANG Yue, LIANG Wenyi, LIU Yumin. Effect of rhubarb on gut microbiota-host co-metabolism in rats [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2023, 43(8): 997-1007. |
| [8] | WEN Yajin, HE Wen, HAN Xiao, ZHANG Xiaobo. Exploratory analysis of gut microbiota differences in childhood asthma with different severity [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2023, 43(6): 655-664. |
| [9] | JIANG Xinting, HUANG Gaozhong. Research progress in the effect of nutritional intervention on cognitive impairment related to Alzheimer's disease [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2023, 43(6): 788-794. |
| [10] | LIU Qianruo, FANG Zichen, WU Yuhan, ZHONG Xianxin, GUO Muhe, JIA Jie. Research progress in the relationship between gut microbia and its metabolites and gestational diabetes mellitus [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2023, 43(5): 641-647. |
| [11] | XU Yidan, ZHANG Qianren, LU Xingyu, DONG Yan. Effect of maternal high-fat diet on placental phenotype in mice [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2023, 43(4): 397-405. |
| [12] | ZHANG Yue, QU Lei, GU Qin, ZHU Yiqing, MA Liying, SUN Wenguang. Effect of continuous positive urine ketone body on clinical outcomes of pregnant women with gestational diabetes mellitus and newborn [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2023, 43(3): 314-319. |
| [13] | LU Yu, WANG Hao, BA Qian. Role of gut microbiota in hepatocellular carcinoma: cancer occurrence, progresses and treatments [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2022, 42(7): 939-944. |
| [14] | WU Ya, YIN Jun. Research progress of ketogenic diet regulating intestinal microbiome in the treatment of diseases [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2022, 42(4): 545-550. |
| [15] | Qin GU, Yingqian XIA, Yiqing ZHU, Liying MA, Lei QU, Wenguang SUN. Analysis of the effects of individualized one-day outpatient diet guidance on glycemic control, body weight gain rate and pregnancy outcome in pregnant women with gestational diabetes mellitus [J]. JOURNAL OF SHANGHAI JIAOTONG UNIVERSITY (MEDICAL SCIENCE), 2022, 42(2): 185-191. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||