
上海交通大学学报(医学版) ›› 2024, Vol. 44 ›› Issue (10): 1307-1315.doi: 10.3969/j.issn.1674-8115.2024.10.013
• 综述 • 上一篇
收稿日期:2024-03-20
接受日期:2024-06-04
出版日期:2024-10-28
发布日期:2024-10-28
通讯作者:
刘敏
E-mail:czixuan2023@126.com;lm4104@shtrhospital.com
作者简介:陈子旋(1999—),男,傣族,硕士生;电子信箱:czixuan2023@126.com。
基金资助:Received:2024-03-20
Accepted:2024-06-04
Online:2024-10-28
Published:2024-10-28
Contact:
LIU Min
E-mail:czixuan2023@126.com;lm4104@shtrhospital.com
Supported by:摘要:
肾细胞癌(renal cell carcinoma,RCC)起源于肾小管上皮细胞,是最常见的肾癌类型,也是死亡率最高的泌尿系统肿瘤。近半个世纪以来,RCC的发病率和死亡率持续上升,给人类健康带来了极大的威胁。尽管手术治疗为大多数 RCC 患者提供了治愈的可能,但肿瘤的复发或转移导致传统治疗方案无法达到理想的效果。因此,受体酪氨酸激酶抑制剂和免疫检查点抑制剂等靶向药物的出现,给RCC的治疗带来了新的希望。靶向治疗成为治疗晚期RCC的主要方式。舒尼替尼是一种受体酪氨酸激酶抑制剂,其通过抑制表皮生长因子受体、血小板衍生生长因子受体、血管内皮生长因子受体等多种受体酪氨酸激酶的活性,抑制肿瘤的血管生成和细胞增殖,最终有效控制肿瘤进展,在RCC的治疗中发挥着关键作用。然而,相当多的RCC患者在使用舒尼替尼治疗后的15个月内对其产生耐药性,给RCC的治疗带来了新的挑战。该文总结了RCC舒尼替尼耐药性的发生机制,归纳了RCC舒尼替尼耐药性的治疗策略,以期为克服RCC对舒尼替尼的耐药,给晚期RCC患者制定更有效的治疗方案提供思路。
中图分类号:
陈子旋, 刘敏. 肾细胞癌舒尼替尼耐药性的机制及治疗研究进展[J]. 上海交通大学学报(医学版), 2024, 44(10): 1307-1315.
CHEN Zixuan, LIU Min. Progress in mechanisms and treatment of sunitinib resistance in renal cell carcinoma[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2024, 44(10): 1307-1315.
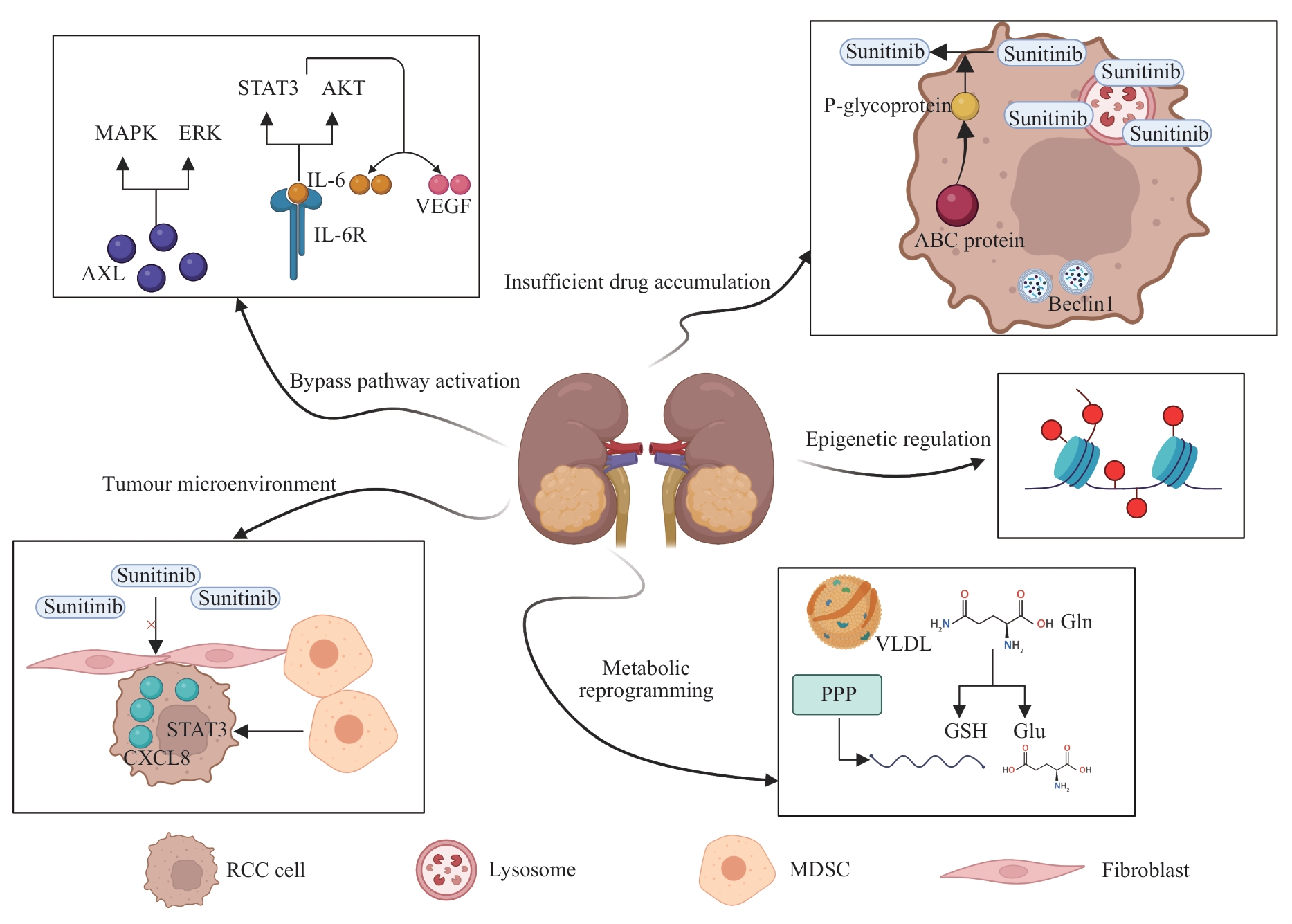
图1 肾细胞癌舒尼替尼耐药性的机制Note: MAPK—mitogen-activated protein kinase; ERK—extracellular regulated protein kinase; IL-6—interleukin-6; STAT3—signal transducer and activator of transcription 3; AKT—protein kinase B; VEGF—vascular endothelial growth factor; AXL—AXR1-like; CXCL8—C-X-C motif chemokine ligand 8; ABC—ATP-binding cassette; VLDL—very-low-density lipoprotein; PPP—pentose phosphate pathway; Gln—glutamine; GSH—glutathione; Glu—glutamate; MDSC—myeloid-derived suppressor cell.
Fig 1 Mechanisms of sunitinib resistance in renal cell carcinoma
| 1 | RAHIB L, WEHNER M R, MATRISIAN L M, et al. Estimated projection of US cancer incidence and death to 2040[J]. JAMA Netw Open, 2021, 4(4): e214708. |
| 2 | SEMENESCU L E, KAMEL A, CIUBOTARU V, et al. An overview of systemic targeted therapy in renal cell carcinoma, with a focus on metastatic renal cell carcinoma and brain metastases[J]. Curr Issues Mol Biol, 2023, 45(9): 7680-7704. |
| 3 | JIN J, XIE Y H, ZHANG J S, et al. Sunitinib resistance in renal cell carcinoma: from molecular mechanisms to predictive biomarkers[J]. Drug Resist Updat, 2023, 67: 100929. |
| 4 | SHARMA R, KADIFE E, MYERS M, et al. Determinants of resistance to VEGF-TKI and immune checkpoint inhibitors in metastatic renal cell carcinoma[J]. J Exp Clin Cancer Res, 2021, 40(1): 186. |
| 5 | BI K, HE M X, BAKOUNY Z, et al. Tumor and immune reprogramming during immunotherapy in advanced renal cell carcinoma[J]. Cancer Cell, 2021, 39(5): 649-661.e5. |
| 6 | MIKAMI S, MIZUNO R, KOSAKA T, et al. Significance of tumor microenvironment in acquiring resistance to vascular endothelial growth factor-tyrosine kinase inhibitor and recent advance of systemic treatment of clear cell renal cell carcinoma[J]. Pathol Int, 2020, 70(10): 712-723. |
| 7 | 何凯桐, 周阳, 王明珠, 等. 受体酪氨酸激酶AXL在肿瘤生物学中的作用研究进展[J]. 现代肿瘤医学, 2024, 32(1): 167-171. |
| HE K T, ZHOU Y, WANG M Z, et al. Research progress on the role of receptor tyrosine kinase AXL in tumor biology [J]. Journal of Modern Oncology, 2024, 32(1): 167-171. | |
| 8 | CHEN S J, QIAN S B, ZHANG L, et al. Tumor-associated macrophages promote migration and invasion via modulating IL-6/STAT3 signaling in renal cell carcinoma[J]. Int Immunopharmacol, 2022, 111: 109139. |
| 9 | WANG Y, WANG Y Y, QIN Z Y, et al. The role of non-coding RNAs in ABC transporters regulation and their clinical implications of multidrug resistance in cancer[J]. Expert Opin Drug Metab Toxicol, 2021, 17(3): 291-306. |
| 10 | LIU S Z, YAO S J, YANG H, et al. Autophagy: regulator of cell death[J]. Cell Death Dis, 2023, 14(10): 648. |
| 11 | LI X H, HE S K, MA B Y. Autophagy and autophagy-related proteins in cancer[J]. Mol Cancer, 2020, 19(1): 12. |
| 12 | WONG J J W, BERSTAD M B, FREMSTEDAL A S V, et al. Photochemically-induced release of lysosomal sequestered sunitinib: obstacles for therapeutic efficacy[J]. Cancers, 2020, 12(2): 417. |
| 13 | NAGASE K, AKUTAGAWA T, RIKITAKE-YAMAMOTO M, et al. Cellular and physical microenvironments regulate the aggressiveness and sunitinib chemosensitivity of clear cell renal cell carcinoma[J]. J Pathol, 2021, 254(1): 46-56. |
| 14 | AMBROSETTI D, COUTTS M, PAOLI C, et al. Cancer-associated fibroblasts in renal cell carcinoma: implication in prognosis and resistance to anti-angiogenic therapy[J]. BJU Int, 2022, 129(1): 80-92. |
| 15 | XU C F, JOHNSON T, GARCIA-DONAS J, et al. IL8 polymorphisms and overall survival in pazopanib- or sunitinib-treated patients with renal cell carcinoma[J]. Br J Cancer, 2015, 112(7): 1190-1198. |
| 16 | 彭恬, 徐雷鸣. 表观遗传修饰与环状RNA在结直肠癌中相互作用的研究进展[J]. 上海交通大学学报(医学版), 2023, 43(2): 237-243. |
| PENG T, XU L M. Crosstalk between epigenetic modification and circRNA in colorectal cancer: recent advances [J]. Journal of Shanghai Jiao Tong University (Medical Science), 2023, 43(2): 237-243. | |
| 17 | ZHAO T L, ZHOU Y L, WANG Q Y, et al. QPCT regulation by CTCF leads to sunitinib resistance in renal cell carcinoma by promoting angiogenesis[J]. Int J Oncol, 2021, 59(1): 48. |
| 18 | CHEN Y L, LU Z Y, QI C, et al. N6-methyladenosine-modified TRAF1 promotes sunitinib resistance by regulating apoptosis and angiogenesis in a METTL14-dependent manner in renal cell carcinoma[J]. Mol Cancer, 2022, 21(1): 111. |
| 19 | WANG J F, WANG C, XU P, et al. PRMT1 is a novel molecular therapeutic target for clear cell renal cell carcinoma[J]. Theranostics, 2021, 11(11): 5387-5403. |
| 20 | LIU Y Q, ZHANG H, FANG Y, et al. Non-coding RNAs in renal cell carcinoma: implications for drug resistance[J]. Biomedecine Pharmacother, 2023, 164: 115001. |
| 21 | ZHU H Y, WANG X, LU S H, et al. Metabolic reprogramming of clear cell renal cell carcinoma[J]. Front Endocrinol, 2023, 14: 1195500. |
| 22 | SATO T, KAWASAKI Y, MAEKAWA M, et al. Metabolomic analysis to elucidate mechanisms of sunitinib resistance in renal cell carcinoma[J]. Metabolites, 2020, 11(1): 1. |
| 23 | LIBERTI M V, LOCASALE J W. The Warburg effect: how does it benefit cancer cells?[J]. Trends Biochem Sci, 2016, 41(3): 211-218. |
| 24 | CHEN W F, HILL H, CHRISTIE A, et al. Targeting renal cell carcinoma with a HIF-2 antagonist[J]. Nature, 2016, 539(7627): 112-117. |
| 25 | NAITO S, MAKHOV P, ASTSATUROV I, et al. LDL cholesterol counteracts the antitumour effect of tyrosine kinase inhibitors against renal cell carcinoma[J]. Br J Cancer, 2017, 116(9): 1203-1207. |
| 26 | GARCIA J, HURWITZ H I, SANDLER A B, et al. Bevacizumab (Avastin®) in cancer treatment: a review of 15years of clinical experience and future outlook[J]. Cancer Treat Rev, 2020, 86: 102017. |
| 27 | ZOU Z L, TAO T, LI H M, et al. mTOR signaling pathway and mTOR inhibitors in cancer: progress and challenges[J]. Cell Biosci, 2020, 10: 31. |
| 28 | MAKHOV P B, GOLOVINE K, KUTIKOV A, et al. Modulation of Akt/mTOR signaling overcomes sunitinib resistance in renal and prostate cancer cells[J]. Mol Cancer Ther, 2012, 11(7): 1510-1517. |
| 29 | SAHARINEN P, EKLUND L, ALITALO K. Therapeutic targeting of the angiopoietin-TIE pathway[J]. Nat Rev Drug Discov, 2017, 16(9): 635-661. |
| 30 | MOOI J, CHIONH F, SAVAS P, et al. Dual antiangiogenesis agents bevacizumab plus trebananib, without chemotherapy, in first-line treatment of metastatic colorectal cancer: results of a phase II study[J]. Clin Cancer Res, 2021, 27(8): 2159-2167. |
| 31 | ATKINS M B, GRAVIS G, DROSIK K, et al. Trebananib (AMG 386) in combination with sunitinib in patients with metastatic renal cell cancer: an open-label, multicenter, phase II study[J]. J Clin Oncol, 2015, 33(30): 3431-3438. |
| 32 | SAMMARCO E, MANFREDI F, NUZZO A, et al. Immune checkpoint inhibitor rechallenge in renal cell carcinoma: current evidence and future directions[J]. Cancers, 2023, 15(12): 3172. |
| 33 | MOTZER R J, POWLES T, BUROTTO M, et al. Nivolumab plus cabozantinib versus sunitinib in first-line treatment for advanced renal cell carcinoma (CheckMate 9ER): long-term follow-up results from an open-label, randomised, phase 3 trial[J]. Lancet Oncol, 2022, 23(7): 888-898. |
| 34 | BAJALIA E M, AZZOUZ F B, CHISM D A, et al. Phytochemicals for the prevention and treatment of renal cell carcinoma: preclinical and clinical evidence and molecular mechanisms[J]. Cancers, 2022, 14(13): 3278. |
| 35 | ASHAQ A, MAQBOOL M F, MARYAM A, et al. Hispidulin: a novel natural compound with therapeutic potential against human cancers[J]. Phytother Res, 2021, 35(2): 771-789. |
| 36 | PORTA C, PROCOPIO G, CARTENÌ G, et al. Sequential use of sorafenib and sunitinib in advanced renal-cell carcinoma (RCC): an Italian multicentre retrospective analysis of 189 patient cases[J]. BJU Int, 2011, 108(8 Pt 2): E250-E257. |
| 37 | 张楠. 口服抗癌疫苗正在走向现实[N]. 中国科学报, 2022-05-16(3). |
| ZHANG N. Oral cancer vaccines are becoming a reality[N]. China Science Daily, 2022-05-16(3). | |
| 38 | DEBENEDETTE M, GAMBLE A, NORRIS M, et al. A review of the clinical experience with CMN-001, a tumor RNA loaded dendritic cell immunotherapy for the treatment of metastatic renal cell carcinoma[J]. Hum Vaccin Immunother, 2023, 19(2): 2220629. |
| 39 | CHEN R H, XIAO Z W, YAN X Q, et al. Tumor cell-secreted ISG15 promotes tumor cell migration and immune suppression by inducing the macrophage M2-like phenotype[J]. Front Immunol, 2020, 11: 594775. |
| 40 | NGUYEN H M, OLADEJO M, PAULISHAK W, et al. A Listeria-based vaccine targeting ISG15 exerts anti-tumor efficacy in renal cell carcinoma[J]. Cancer Immunol Immunother, 2023, 72(9): 2889-2903. |
| 41 | PUROHIT K, REDDY N, SUNNA A. Exploring the potential of bioactive peptides: from natural sources to therapeutics[J]. Int J Mol Sci, 2024, 25(3): 1391. |
| 42 | KUMAR V, BARWAL A, SHARMA N, et al. Therapeutic proteins: developments, progress, challenges, and future perspectives[J]. 3 Biotech, 2024, 14(4): 112. |
| 43 | ZHANG L, JIN G Z, LI D. Tat-hspb1 suppresses clear cell renal cell carcinoma (ccRCC) growth via lysosomal membrane permeabilization[J]. Cancers (Basel), 2022, 14(22): 5710. |
| 44 | LI X, LIU M H, LIU H Y, et al. Tumor metabolic reprogramming in lung cancer progression[J]. Oncol Lett, 2022, 24(2): 287. |
| 45 | WANG R L, YAN Q, LIU X, et al. Unraveling lipid metabolism reprogramming for overcoming drug resistance in melanoma[J]. Biochem Pharmacol, 2024, 223: 116122. |
| 46 | JONASCH E, WALKER C L, RATHMELL W K. Clear cell renal cell carcinoma ontogeny and mechanisms of lethality[J]. Nat Rev Nephrol, 2021, 17(4): 245-261. |
| 47 | CHOUEIRI T K, BAUER T M, PAPADOPOULOS K P, et al. Inhibition of hypoxia-inducible factor-2α in renal cell carcinoma with belzutifan: a phase 1 trial and biomarker analysis[J]. Nat Med, 2021, 27(5): 802-805. |
| 48 | TAN S K, HOUGEN H Y, MERCHAN J R, et al. Fatty acid metabolism reprogramming in ccRCC: mechanisms and potential targets[J]. Nat Rev Urol, 2023, 20(1): 48-60. |
| 49 | ZHOU L J, LUO Y B, LIU Y N, et al. Fatty acid oxidation mediated by malonyl-CoA decarboxylase represses renal cell carcinoma progression[J]. Cancer Res, 2023, 83(23): 3920-3939. |
| 50 | BENSAAD K, FAVARO E, LEWIS C A, et al. Fatty acid uptake and lipid storage induced by HIF-1α contribute to cell growth and survival after hypoxia-reoxygenation[J]. Cell Rep, 2014, 9(1): 349-365. |
| 51 | MURANAKA H, AKINSOLA R, BILLET S, et al. Glutamine supplementation as an anticancer strategy: a potential therapeutic alternative to the convention[J]. Cancers, 2024, 16(5): 1057. |
| 52 | MOROZUMI K, KAWASAKI Y, SATO T, et al. Elucidation and regulation of tyrosine kinase inhibitor resistance in renal cell carcinoma cells from the perspective of glutamine metabolism[J]. Metabolites, 2024, 14(3): 170. |
| 53 | SCHULTE M L, FU A, ZHAO P, et al. Pharmacological blockade of ASCT2-dependent glutamine transport leads to antitumor efficacy in preclinical models[J]. Nat Med, 2018, 24(2): 194-202. |
| 54 | LOI S, SETTLEMAN J, JOYCE J A, et al. The next big questions in cancer research[J]. Cell, 2023, 186(8): 1523-1527. |
| [1] | 张烨晟, 杨易静, 黄依雯, 施珑玙, 王曼媛, 陈思思. 肿瘤微环境免疫细胞调节肿瘤细胞耐药性的研究进展[J]. 上海交通大学学报(医学版), 2024, 44(7): 830-838. |
| [2] | 周婉桢, 滕银成. 非经典Wnt通路在卵巢癌中的作用与潜在治疗意义研究进展[J]. 上海交通大学学报(医学版), 2023, 43(8): 1056-1063. |
| [3] | 崔芷嫣, 陈尧, 陶悦, 沈树红, 李慧. PRPS1 I72位点突变对急性淋巴细胞白血病耐药性的影响及其机制研究[J]. 上海交通大学学报(医学版), 2023, 43(8): 977-987. |
| [4] | 赵富茂, 彭玫, 彭晓露, 舒韦韦, 彭丽. 鲍曼不动杆菌在环境美罗培南浓度变化时耐药性的改变及其机制[J]. 上海交通大学学报(医学版), 2023, 43(11): 1396-1407. |
| [5] | 张漪蓉, 魏玮庆, 马皎, 张雪. 靶向SOX9调控弥漫性大B细胞淋巴瘤代谢重编程的研究[J]. 上海交通大学学报(医学版), 2023, 43(10): 1236-1244. |
| [6] | 汤开然, 吴琼, 黄思佳, 邱旭东, 李文彦, 邓华云, 黄雷. 与MUC1共同调控肿瘤化疗耐药的MUCIN家族成员的筛选[J]. 上海交通大学学报(医学版), 2022, 42(9): 1288-1295. |
| [7] | 廖雅慧, 刘丽云, 朱泓睿, 林厚文, 严继舟, 孙凡. 海绵来源的smenospongine通过抑制非小细胞肺癌细胞中的EGFR-Akt-ABCG2信号通路抑制顺铂耐药[J]. 上海交通大学学报(医学版), 2022, 42(8): 997-1007. |
| [8] | 李聪聪, 姚玉峰, 张传珍. 铜绿假单胞菌对环丙沙星异质性耐药的研究[J]. 上海交通大学学报(医学版), 2022, 42(7): 839-845. |
| [9] | 向晗, 向武, 张伟国. 获得性囊性肾病相关肾细胞癌的研究进展[J]. 上海交通大学学报(医学版), 2022, 42(5): 680-684. |
| [10] | 陆文清, 孟周文理, 虞永峰, 陆舜. 非小细胞肺癌第三代表皮生长因子受体-酪氨酸激酶抑制剂的耐药机制及治疗策略[J]. 上海交通大学学报(医学版), 2022, 42(4): 535-544. |
| [11] | 林艳艳, 许岩, 李慧. 儿童急性淋巴细胞白血病化学治疗常规药物耐药机制的研究进展[J]. 上海交通大学学报(医学版), 2022, 42(2): 211-217. |
| [12] | 赵雪, 董春燕. WD40重复蛋白43在肺腺癌中的表达及其对细胞紫杉醇耐药的影响[J]. 上海交通大学学报(医学版), 2022, 42(12): 1656-1665. |
| [13] | 姜春宇, 郭晓奎, 秦金红. 肺炎克雷伯菌CRISPR-Cas系统及anti-CRISPR蛋白家族研究进展[J]. 上海交通大学学报(医学版), 2022, 42(12): 1757-1765. |
| [14] | 李莉莎, 李建辉, 何斌, 吴楠楠, 朱同玉, 郭晓奎, 陈峥宏. 噬菌体治疗泛耐药肺炎克雷伯菌肺部感染的临床应用及效果初探[J]. 上海交通大学学报(医学版), 2021, 41(9): 1272-1276. |
| [15] | 徐建华, 江萍, 邓炯. ATP结合盒蛋白G超家族成员2在肺癌中的表达及意义[J]. 上海交通大学学报(医学版), 2021, 41(6): 830-833. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||
