
上海交通大学学报(医学版) ›› 2024, Vol. 44 ›› Issue (12): 1526-1535.doi: 10.3969/j.issn.1674-8115.2024.12.005
• 论著 · 基础研究 • 上一篇
王卫( ), 王红丽, 阿力比亚提·艾尼, 衣力亚尔·肉苏, 阿依努尔, 杨亮(
), 王红丽, 阿力比亚提·艾尼, 衣力亚尔·肉苏, 阿依努尔, 杨亮( )
)
收稿日期:2024-03-10
接受日期:2024-07-10
出版日期:2024-12-28
发布日期:2024-12-28
通讯作者:
杨亮
E-mail:2449965197@qq.com;xjzlyangliang@sina.com
作者简介:王 卫(1996—),男,住院医师,硕士;电子信箱:2449965197@qq.com。
基金资助:
WANG Wei( ), WANG Hongli, ALIBIYATI·i Ain, YILIYAER· Rousu, AYI NUER, YANG Liang(
), WANG Hongli, ALIBIYATI·i Ain, YILIYAER· Rousu, AYI NUER, YANG Liang( )
)
Received:2024-03-10
Accepted:2024-07-10
Online:2024-12-28
Published:2024-12-28
Contact:
YANG Liang
E-mail:2449965197@qq.com;xjzlyangliang@sina.com
Supported by:摘要:
目的·探索血管抑制蛋白2(vasohibin-2,VASH2)在三阴性乳腺癌(triple-negative breast cancer,TNBC)中的表达及VASH2通过调控基因表达和可变剪接在TNBC发生发展中的作用机制。方法·通过基因型-组织表达数据库(Genotype-Tissue Expression,GTEx)联合癌症基因组图谱数据库(The Cancer Genome Atlas,TCGA)比较VASH2在TNBC中与正常乳腺组织中的表达差异,并分析VASH2在TNBC中的甲基化水平。在TNBC细胞系MDA-MB-231中对VASH2过表达,并进行转录组测序,分析受VASH2所调控的差异表达基因及可变剪接基因。结果·VASH2在TNBC组织中与正常组织及其他乳腺癌分型比较表达水平显著提高。VASH2基因的低甲基化可能是VASH2在TNBC 中表达上调的原因之一。VASH2过表达后引起81个基因显著差异表达,其中上调的基因23个,下调的基因58个。VASH2过表达后可变剪接水平发生显著变化的基因主要富集在细胞周期、p53信号通路上。结论·VASH2可能通过调控TNBC中基因可变剪接促进其发生和发展。
中图分类号:
王卫, 王红丽, 阿力比亚提·艾尼, 衣力亚尔·肉苏, 阿依努尔, 杨亮. 血管抑制蛋白2在三阴性乳腺癌中的功能及其调控可变剪接机制[J]. 上海交通大学学报(医学版), 2024, 44(12): 1526-1535.
WANG Wei, WANG Hongli, ALIBIYATI·i Ain, YILIYAER· Rousu, AYI NUER, YANG Liang. Function of vasohibin-2 and the mechanism of alternative splicing in triple-negative breast cancer[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2024, 44(12): 1526-1535.
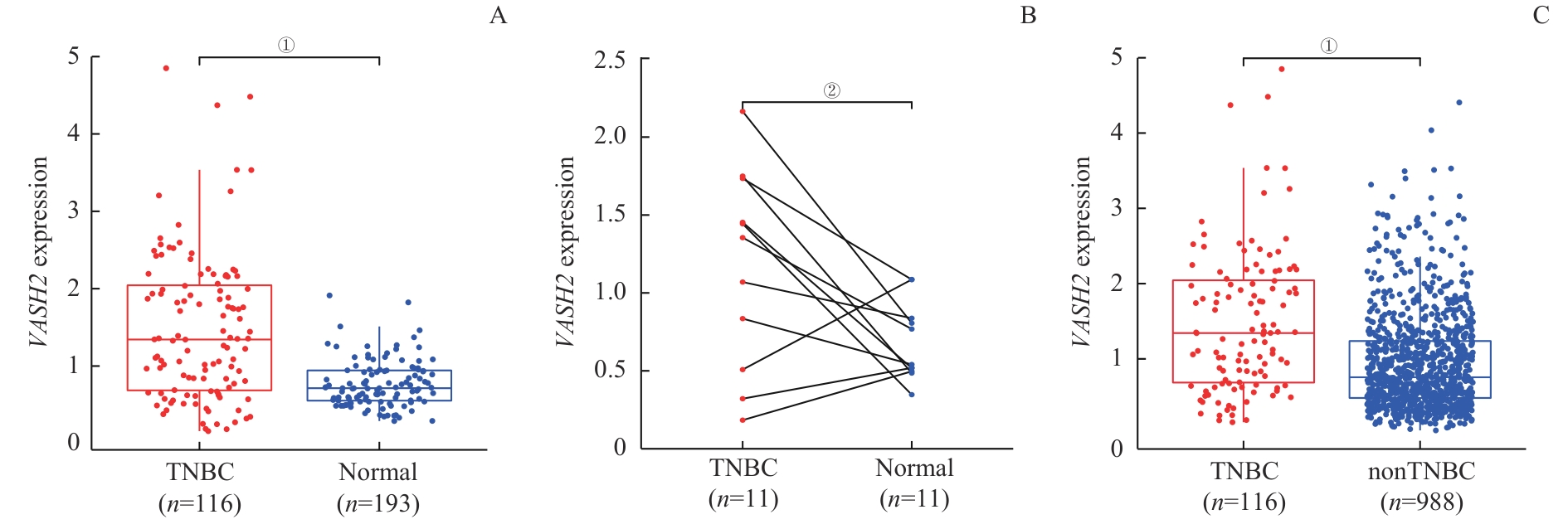
图1 VASH2 的差异表达Note: A. Differential expression between TNBC and normal breast tissues. B. Differential expression between TNBC and paired cancer-adjacent tissues. C. Comparative analysis between TNBC and nonTNBC. ①P<0.001, ②P=0.035.
Fig 1 Differential expression of VASH2
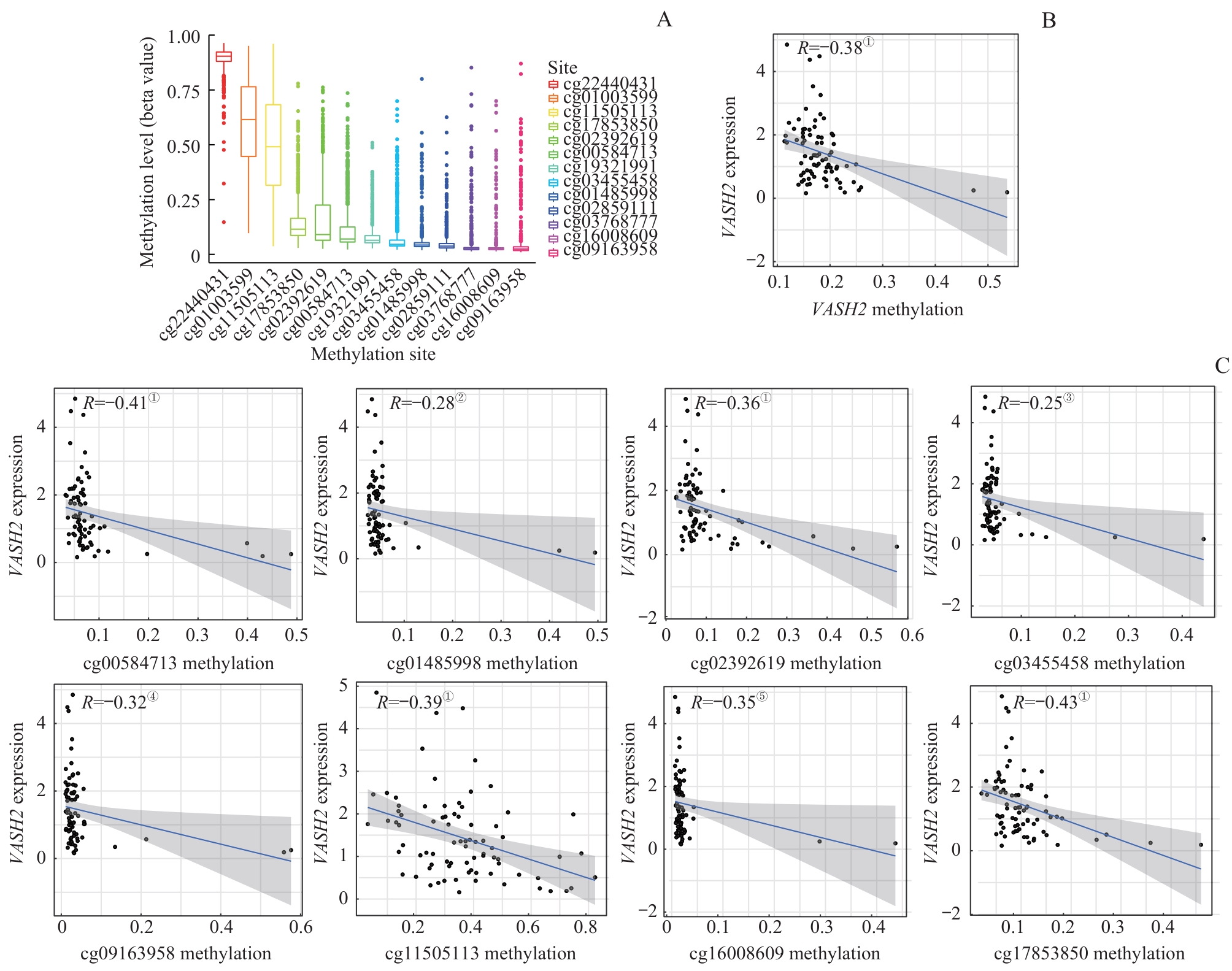
图2 VASH2 在TNBC中的甲基化分析Note: A. Methylation site correlation analysis in the VASH2 promoter. B. Methylation levels corresponded to VASH2 expression. C. Correlation analysis between the degree of methylation sites and the expression of VASH2. ①P<0.001, ②P=0.011, ③P=0.029, ④P=0.004, ⑤P=0.002.
Fig 2 Methylated analysis of VASH2 in TNBC
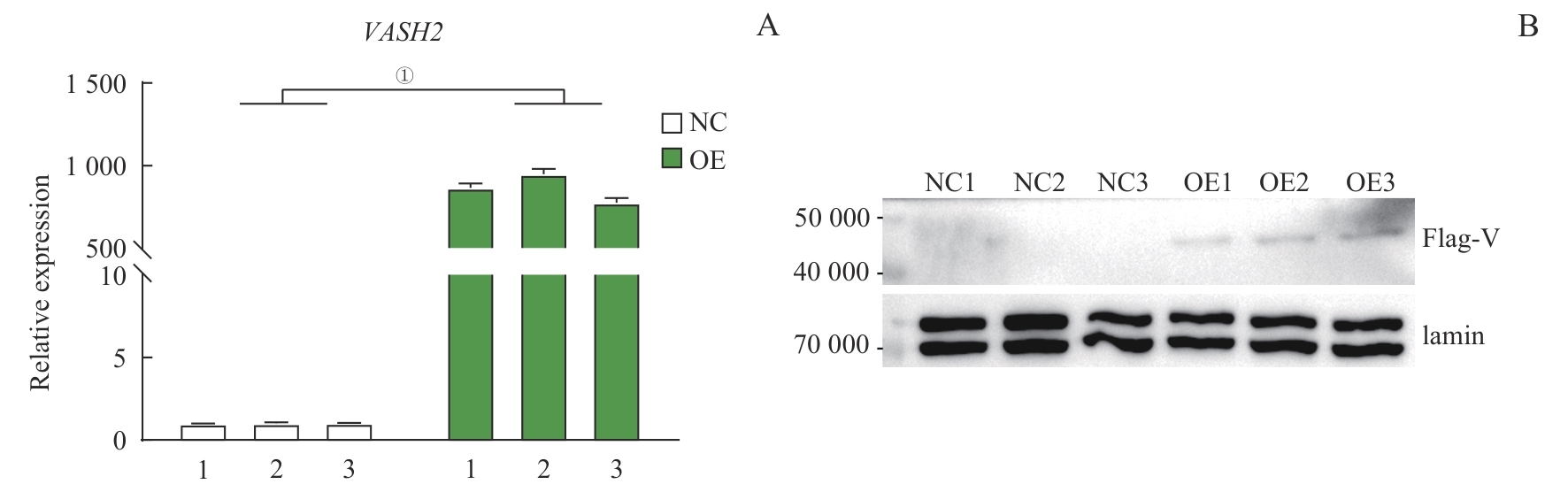
图3 验证VASH2在MDA-MB-231细胞中高表达Note: A. RT-qPCR results of OE-VASH2 and the control groups. B. Western blotting results. ①P<0.001, compared with the control groups.
Fig 3 Verification of high expression of VASH2 in MDA-MB-231 cells
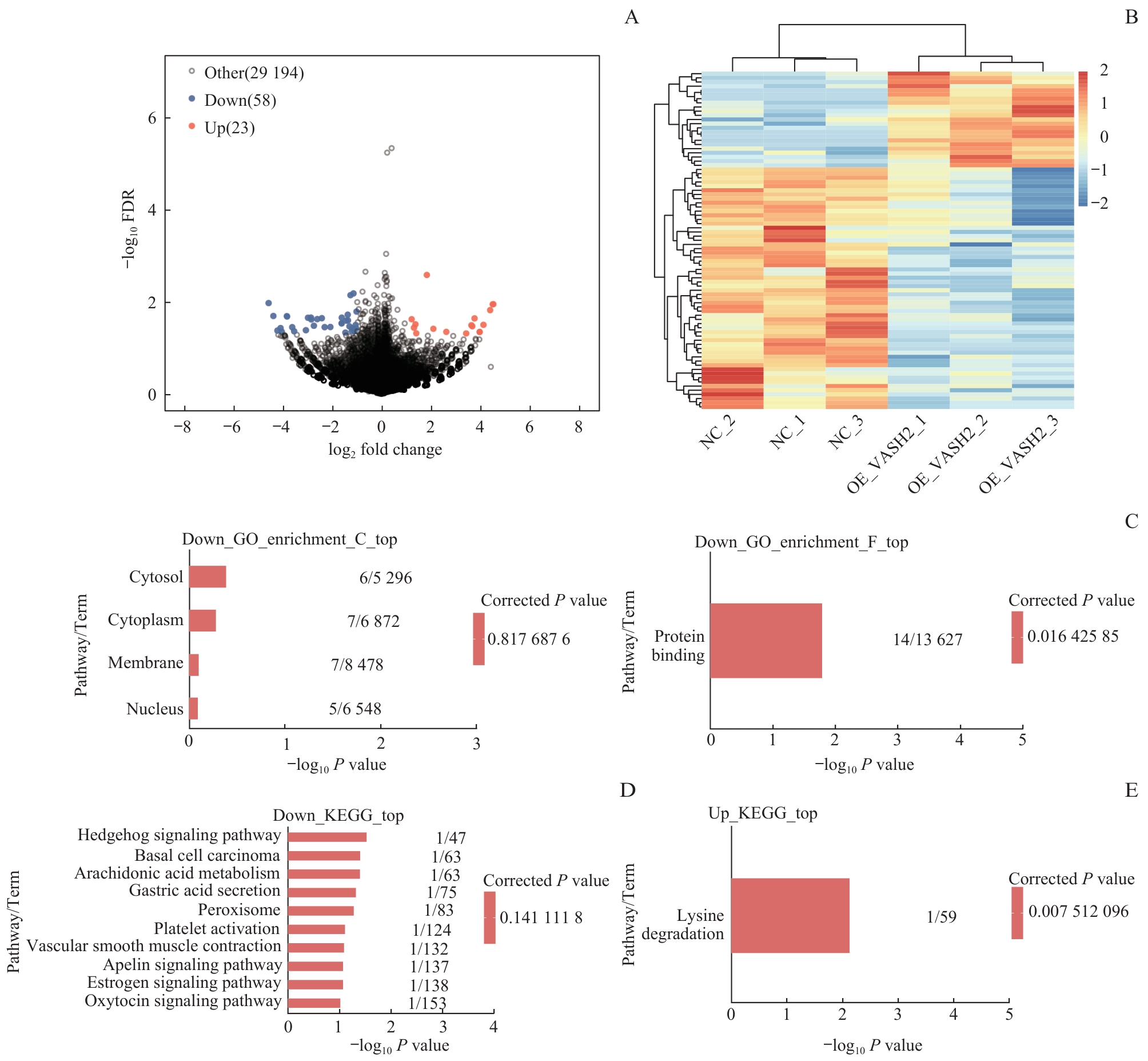
图4 VASH2 调控转录组的RNA-seq分析Note: A. Volcano map based on differentially expressed genes (DEGs). B. Heat map of expression levels of DEGs. C. GO function enrichment bar chart. D/E. Bar charts showing KEGG pathway enrichment of downregulated DEGs (D) and upregulated DEGs (E).
Fig 4 RNA-seq analysis of VASH2-regulated transcriptome
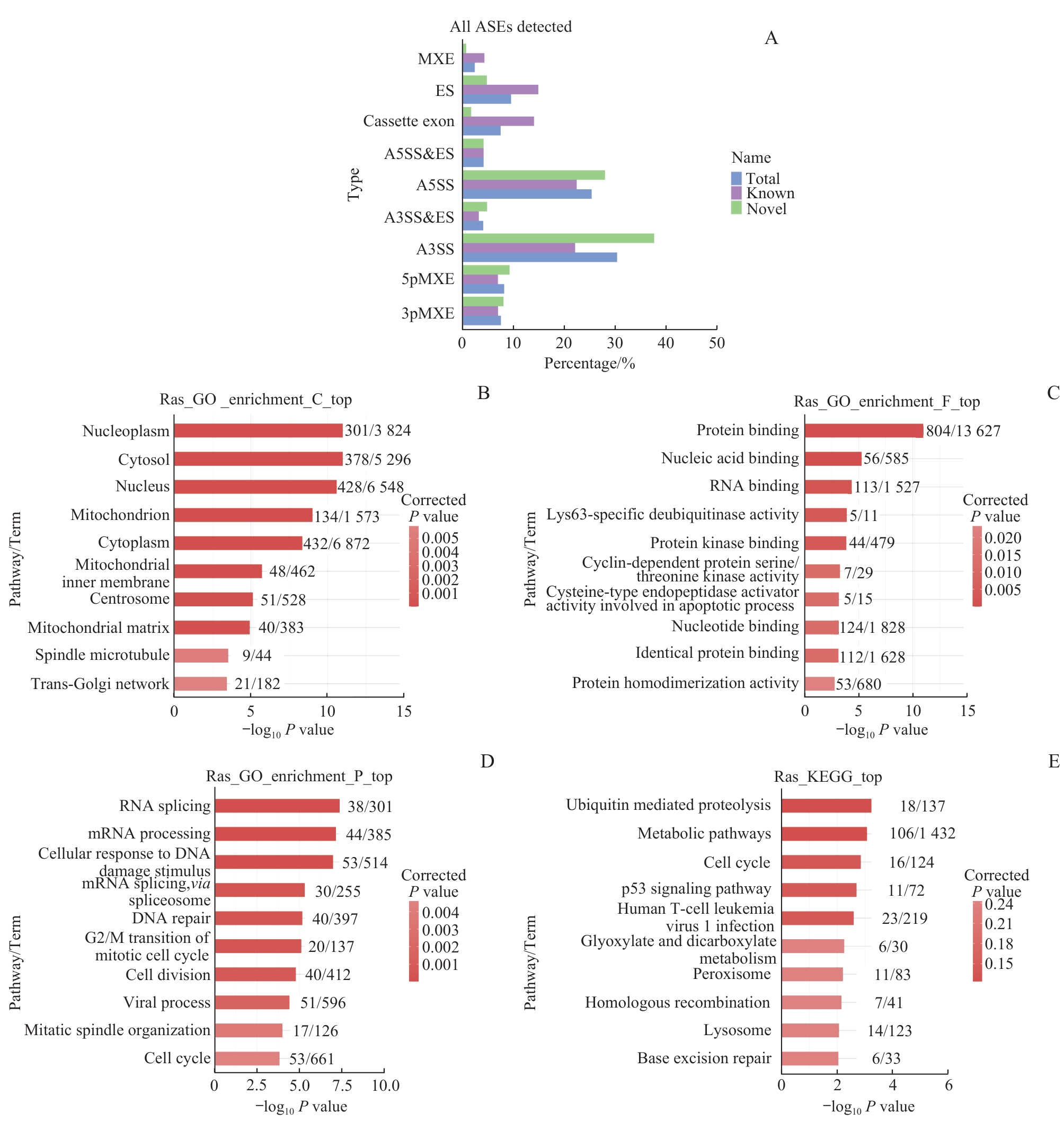
图5 MDA-MB-231细胞中 VASH2 调控的可变剪接事件及功能分析Note: A. Classification of RASEs. B?D. Regulation of top 10 enriched GO biological processes for VASH2. E. Top 10 enriched KEGG pathways for VASH2.
Fig 5 RASEs in MDA-MB-231 cells and function analysis
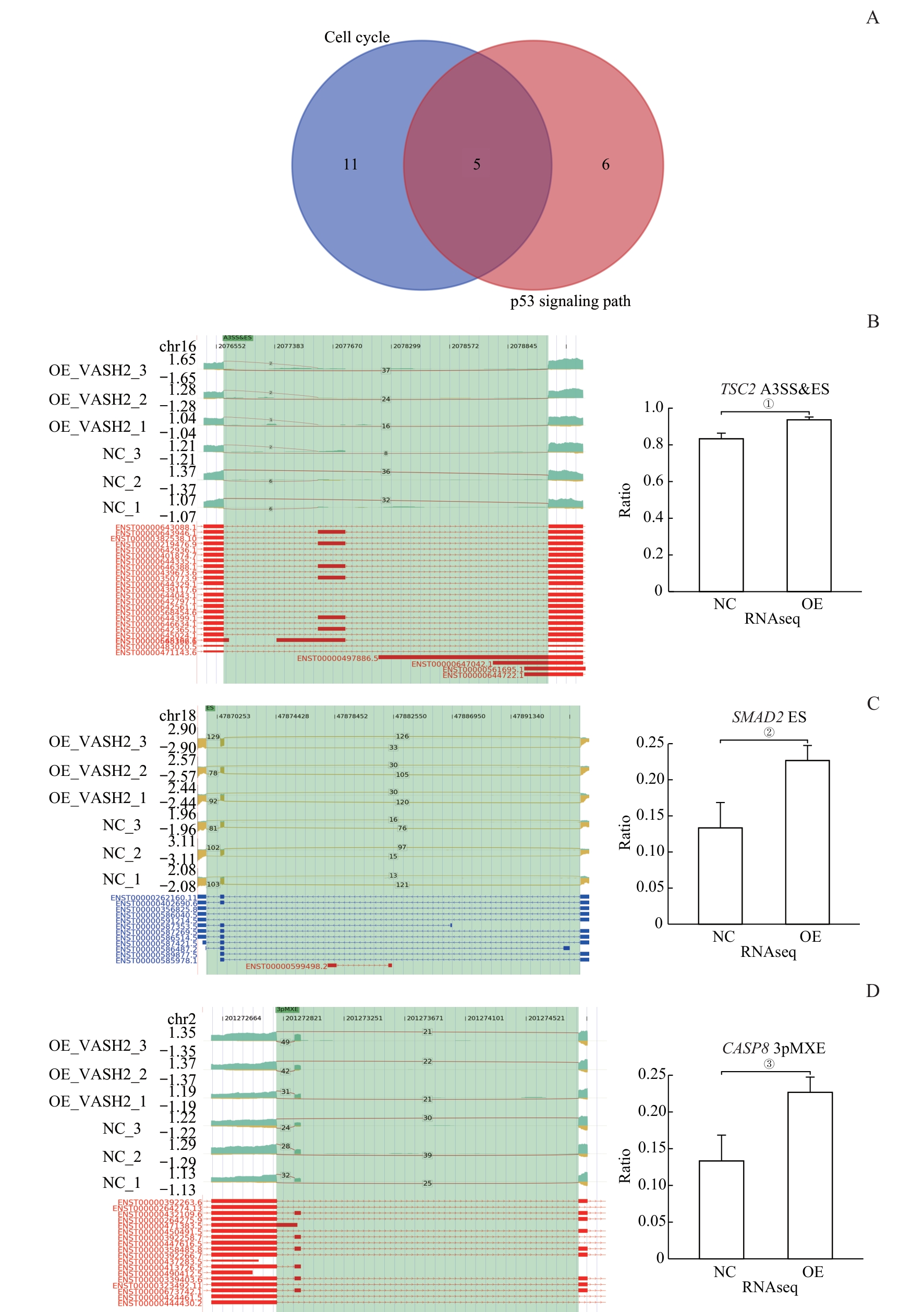
图6 富含细胞凋亡事件的可变剪接基因Note: A. Wayne diagram of the gene set with significantly altered AS expression levels in the cell cycle and p53 signaling pathway. B. ASE of the VASH2-regulated gene TSC2 and IGV-sashimi plot showing A3SS & ES events. C.ASE of the VASH2-regulated gene SMAD2 and IGV-sashimi plot showing ES events. D. ASE of the VASH2-regulated gene CASP8. ①P=0.006, ②P=0.017, ③P=0.027.
Fig 6 Apoptosis-enriched alternative splicing genes
| 1 | DERAKHSHAN F, REIS-FILHO J S. Pathogenesis of triple-negative breast cancer[J]. Annu Rev Pathol, 2022, 17: 181-204. |
| 2 | ZONG Y, PEGRAM M. Research advances and new challenges in overcoming triple-negative breast cancer[J]. Cancer Drug Resist, 2021, 4(3): 517-542. |
| 3 | MERIKHIAN P, EISAVAND M R, FARAHMAND L. Triple-negative breast cancer: understanding Wnt signaling in drug resistance[J]. Cancer Cell Int, 2021, 21(1): 419. |
| 4 | BURSTEIN H J, CURIGLIANO G, THÜRLIMANN B, et al. Customizing local and systemic therapies for women with early breast cancer: the St. Gallen International Consensus Guidelines for treatment of early breast cancer 2021[J]. Ann Oncol. 2021,32(10):1216-1235. |
| 5 | TU J J, FANG Y L, HAN D F, et al. Activation of nuclear factor-κB in the angiogenesis of glioma: insights into the associated molecular mechanisms and targeted therapies[J]. Cell Prolif, 2021, 54(2): e12929. |
| 6 | TAN X B, LIAO Z F, ZOU S Y, et al. VASH2 promotes cell proliferation and resistance to doxorubicin in non-small cell lung cancer via AKT signaling[J]. Oncol Res, 2020, 28(1): 3-11. |
| 7 | NINOMIYA Y, OZAWA S, OGUMA J, et al. Expression of vasohibin-1 and-2 predicts poor prognosis among patients with squamous cell carcinoma of the esophagus[J]. Oncol Lett, 2018, 16(4): 5265-5274. |
| 8 | SATO Y. The vasohibin family: a novel family for angiogenesis regulation[J]. J Biochem, 2013, 153(1): 5-11. |
| 9 | YAMAMOTO M, OZAWA S, NINOMIYA Y, et al. Plasma vasohibin-1 and vasohibin-2 are useful biomarkers in patients with esophageal squamous cell carcinoma[J]. Esophagus, 2020, 17(3): 289-297. |
| 10 | KITAHARA S, SUZUKI Y, MORISHIMA M, et al. Vasohibin-2 modulates tumor onset in the gastrointestinal tract by normalizing tumor angiogenesis[J]. Mol Cancer, 2014, 13: 99. |
| 11 | NORITA R, SUZUKI Y, FURUTANI Y, et al. Vasohibin-2 is required for epithelial-mesenchymal transition of ovarian cancer cells by modulating transforming growth factor-β signaling[J]. Cancer Sci, 2017, 108(3): 419-426. |
| 12 | TU M, LI Z J, LIU X, et al. Vasohibin 2 promotes epithelial-mesenchymal transition in human breast cancer via activation of transforming growth factor β 1 and hypoxia dependent repression of GATA-binding factor 3[J]. Cancer Lett, 2017, 388: 187-197. |
| 13 | MA H R, CAO L, WANG F, et al. Filamin B extensively regulates transcription and alternative splicing, and is associated with apoptosis in HeLa cells[J]. Oncol Rep, 2020, 43(5): 1536-1546. |
| 14 | YISA S B, FEI W M, YAXUN W M, et al. ATP5A1 participates in transcriptional and posttranscriptional regulation of cancer-associated genes by modulating their expression and alternative splicing profiles in HeLa cells[J]. Technol Cancer Res Treat, 2021, 20: 15330338211039126. |
| 15 | 沈鑫鑫, 金磊, 赵倩, 等. 血管抑制蛋白2在乳腺癌中的表达情况及其对患者预后的影响[J]. 安徽医学, 2021, 42(2): 144-148. |
| SHEN X X, JIN L, ZHAO Q, et al. Expression of vasohibin-2 and its effect on prognosis of breast cancer[J]. Anhui Medical Journal, 2021, 42(2): 144-148. | |
| 16 | GAO Y, ZHANG W Z, LIU C W, et al. MiR-200 affects tamoxifen resistance in breast cancer cells through regulation of MYB[J]. Sci Rep, 2019, 9(1): 18844. |
| 17 | ZENG X, QU X J, ZHAO C Y, et al. FEN1 mediates miR-200a methylation and promotes breast cancer cell growth via MET and EGFR signaling[J]. FASEB J, 2019, 33(10): 10717-10730. |
| 18 | ANSARI J, SHACKELFORD R E, EL-OSTA H. Epigenetics in non-small cell lung cancer: from basics to therapeutics[J]. Transl Lung Cancer Res, 2016, 5(2): 155-171. |
| 19 | LI R, YANG Y E, YIN Y H, et al. Methylation and transcriptome analysis reveal lung adenocarcinoma-specific diagnostic biomarkers[J]. J Transl Med, 2019, 17(1): 324. |
| 20 | CHEN Y C, LIU X R, LI Y K, et al. Lung cancer therapy targeting histone methylation: opportunities and challenges[J]. Comput Struct Biotechnol J, 2018, 16: 211-223. |
| 21 | WANG B, YANG L, ZHAO Q, et al. Vasohibin 2 as a potential predictor of aggressive behavior of triple-negative breast cancer[J]. Am J Transl Res, 2017, 9(6): 2911-2919. |
| 22 | LI F X, HU Y J, QI S T, et al. Structural basis of tubulin detyrosination by vasohibins[J]. Nat Struct Mol Biol, 2019, 26(7): 583-591. |
| 23 | VAN DER LAAN S, LÉVÊQUE M F, MARCELLIN G, et al. Evolutionary divergence of enzymatic mechanisms for tubulin detyrosination[J]. Cell Rep, 2019, 29(12): 4159-4171.e6. |
| 24 | NIEUWENHUIS J, ADAMOPOULOS A, BLEIJERVELD O B, et al. Vasohibins encode tubulin detyrosinating activity[J]. Science, 2017, 358(6369): 1453-1456. |
| 25 | JOERGER A C, FERSHT A R. The p53 pathway: origins, inactivation in cancer, and emerging therapeutic approaches[J]. Annu Rev Biochem, 2016, 85: 375-404. |
| 26 | ZHANG H, ZHANG X, LI X, et al. Effect of CCNB1 silencing on cell cycle, senescence, and apoptosis through the p53 signaling pathway in pancreatic cancer[J]. J Cell Physiol, 2018, 234(1): 619-631. |
| 27 | MISSAOUI N, LANDOLSI H, MESTIRI S, et al. Immunohistochemical analysis of c-erbB-2, Bcl-2, p53, p21(WAF1/Cip1), p63 and Ki-67 expression in hydatidiformmoles[J]. Pathol Res Pract,2019,215(3):446-452. |
| 28 | LO W, PARKHURST M, ROBBINS P F, et al. Immunologic recognition of a shared p53 mutated neoantigen in a patient with metastatic colorectal cancer[J]. Cancer Immunol Res,2019,7(4):534-543. |
| 29 | SCHAEFER I M, HORNICK J L, SHOLL L M, et al. Abnormal p53 and p16 staining patterns distinguish uterine leiomyosarcoma from inflammatory myofibroblastic tumour[J]. Histopathology, 2017, 70(7): 1138-1146. |
| 30 | DONNELLAN R, CHETTY R. Cyclin E in human cancers[J]. FASEB J, 1999, 13(8): 773-780. |
| 31 | KEYOMARSI K, O'LEARY N, MOLNAR G, et al. Cyclin E, a potential prognostic marker for breast cancer[J]. Cancer Res, 1994, 54(2): 380-385. |
| 32 | HUANG X, SHAO D, WU H W, et al. Genomic profiling comparison of germline BRCA and non-BRCA carriers reveals CCNE1 amplification as a risk factor for non-BRCA carriers in patients with triple-negative breast cancer[J]. Front Oncol, 2020, 10: 583314. |
| 33 | 杨睿, 陈俊霞. 环状RNA hsa_circ_0058514在三阴性乳腺癌中的表达及作用研究[J]. 中国癌症杂志, 2019, 29(1): 9-18. |
| YANG R, CHEN J X. Effects of circular RNA hsa_circ_0058514 on the development and progression of triple-negative breast cancer[J]. China Oncology, 2019, 29(1): 9-18. | |
| 34 | LIU Z, FU Q S, WANG Y, et al. Synergy between vinorelbine and afatinib in the inhibition of non-small cell lung cancer progression by EGFR and p53 signaling pathways[J]. Biomed Pharmacother, 2021, 134: 111144. |
| [1] | 韩依杉, 徐梓淇, 陶梦玉, 范广建, 余波. PRMT6促进乳腺癌细胞的增殖和迁移[J]. 上海交通大学学报(医学版), 2024, 44(8): 999-1010. |
| [2] | 薛煜, 张海龙, 雷鸣. 癌-睾丸抗原SPANXB在肝癌中的表达及其影响肝癌进展的机制研究[J]. 上海交通大学学报(医学版), 2024, 44(7): 801-813. |
| [3] | 施泽纶, 王青, 何雯, 傅唯佳, 王颖雯, 韩晓, 张晓波. 纳米塑料诱导肺泡Ⅱ型上皮细胞DNA损伤加重重症哮喘[J]. 上海交通大学学报(医学版), 2024, 44(11): 1391-1405. |
| [4] | 王晓玲, 葛梦凯, 沈少明. PTEN对FoxM1可变剪接的调控及该过程在肿瘤细胞迁移中的作用[J]. 上海交通大学学报(医学版), 2023, 43(11): 1339-1347. |
| [5] | 王斓茜, 马官荣, 姜咏竹, 常秀林, 方廖琼, 白晋. 大肠埃希菌外膜囊泡对乳腺癌细胞增殖及荷瘤小鼠肿瘤生长的影响[J]. 上海交通大学学报(医学版), 2023, 43(10): 1245-1254. |
| [6] | 宗春燕, 何杰, 张哲, 贾仁兵, 沈键锋. APOBEC3B调控葡萄膜黑色素瘤复制应激的研究[J]. 上海交通大学学报(医学版), 2022, 42(8): 1034-1044. |
| [7] | 徐斐翔, 汪升, 薛明明, 童朝阳, 陈玉梅. 长链非编码RNA-B230352I09表达改变对H9C2心肌细胞增殖及周期的影响[J]. 上海交通大学学报(医学版), 2022, 42(5): 578-582. |
| [8] | 朱楠, 刘炳亚, 俞焙秦. 肌盲样蛋白1在恶性肿瘤中作用的研究进展[J]. 上海交通大学学报(医学版), 2022, 42(10): 1474-1481. |
| [9] | 陈翠, 金叶, 王琳, 李红丽, 万财凤, 姜立新. 30例乳腺化生性癌的多种影像学对比分析[J]. 上海交通大学学报(医学版), 2022, 42(1): 70-76. |
| [10] | 季艳杰, 罗浩, 蔡海燕, 刘欣宇, 金诗佳, 粟深月, 徐含章, 雷虎, 吴英理. CDDO-Me对三阴性乳腺癌细胞泛素特异性蛋白酶2a活性及细胞增殖的抑制作用[J]. 上海交通大学学报(医学版), 2021, 41(8): 1025-1032. |
| [11] | 赫玮, 左勇. 冬凌草甲素上调PLK1对Jurkat细胞细胞周期的影响[J]. 上海交通大学学报(医学版), 2021, 41(5): 603-611. |
| [12] | 顾琦晟, 张米粒, 曹灿, 李继坤. 基于TCGA数据库分析胃癌可变剪接与肿瘤免疫的关系[J]. 上海交通大学学报(医学版), 2021, 41(4): 448-458. |
| [13] | 张凤春1, 2*,张硕渊3*,陈天恩3,徐迎春3. PD-1/PD-L1通路在三阴性乳腺癌预后预测及治疗中的意义[J]. 上海交通大学学报(医学版), 2020, 40(1): 128-. |
| [14] | 王佳琳,季 迪,陈 祥,杨 博,余 林. miR-218-2-3P靶向SIN3A基因影响NK/T细胞淋巴瘤的增殖和凋亡[J]. 上海交通大学学报(医学版), 2019, 39(12): 1394-. |
| [15] | 狄芳芳,刘建胜,李尚,杜艳芝. 转录因子 C/EBPβ在子宫蜕膜化中的作用及机制研究进展[J]. 上海交通大学学报(医学版), 2017, 37(6): 865-. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||