
上海交通大学学报(医学版) ›› 2023, Vol. 43 ›› Issue (3): 320-332.doi: 10.3969/j.issn.1674-8115.2023.03.008
收稿日期:2022-08-18
接受日期:2022-12-09
出版日期:2023-03-28
发布日期:2023-03-28
通讯作者:
刘宁宁,电子信箱:liuningning@shsmu.edu.cn。作者简介:王安君(1994—),女,硕士生;电子信箱:wanganjun@sjtu.edu.cn。
基金资助:Received:2022-08-18
Accepted:2022-12-09
Online:2023-03-28
Published:2023-03-28
Contact:
LIU Ningning, E-mail: liuningning@shsmu.edu.cn.Supported by:摘要:
目的·利用美国癌症监测、流行病学和结果(Surveillance,Epidemiology and End Results,SEER)数据库评估新辅助放射治疗(放疗)和辅助放疗对行化学治疗(化疗)和手术的直肠癌患者生存的影响。方法·纳入SEER数据库2005—2015年经病理确诊为直肠癌,并接受化疗和手术治疗的患者;排除尸检或仅死亡证明为直肠癌、无随访时间和临床资料不全的患者。将所有患者分为新辅助放疗联合手术组(RT+S组)、手术治疗组(S组)和手术联合辅助放疗组(S+RT组)。采用倾向性评分匹配(propensity score matching,PSM)以1∶1的比例匹配各组纳入对象,采用受限平均生存时间(restricted mean survival time,RMST)估计直肠癌患者5年和10年内平均生存期,采用Cox比例风险模型确定新辅助放疗和辅助放疗对直肠癌患者总生存期(overall survival,OS)和肿瘤特异性生存期(cancer specific survival,CSS)的影响,通过对患者进行分层分析确定新辅助放疗和辅助放疗的具体获益人群。结果·2005—2015年,共纳入8 975例接受化疗和手术的直肠癌患者;其中S组1 079例,RT+S组5 991例,S+RT组1 905例。经PSM后,各组临床基础特征均衡可比。PSM后,与S组相比,RT+S组患者5年和10年的预后均显著改善(均P=0.000),而S+RT组患者仅5年预后显著改善(均P<0.05),10年预后改善不明显(均P>0.05)。多因素Cox回归分析结果显示,新辅助放疗是患者OS和CSS的独立保护因素(均P=0.000),而辅助放疗并不是(均P>0.05)。亚组分析显示:新辅助放疗对于年龄<50岁、肿瘤分化程度高、肿瘤直径≤30 mm或TNM分期Ⅰ~Ⅲ期患者OS和CSS没有明显的保护作用(均P>0.05);而辅助放疗对于肿瘤低分化/未分化、肿瘤直径>50 mm或TNM分期Ⅳ期的患者OS和CSS有明显的保护作用(均P<0.05)。结论·对于行化疗和手术的直肠癌患者,新辅助放疗有明显的生存获益,但可能不适用于年龄<50岁、肿瘤分化程度高、肿瘤直径≤30 mm或TNM分期Ⅰ~Ⅲ期的患者;而肿瘤低分化/未分化、肿瘤直径>50 mm或TNM分期Ⅳ期的患者可能从辅助放疗中获益。
中图分类号:
王安君, 刘宁宁. 放疗对行化疗和手术的直肠癌患者的效果分析:一项基于SEER数据库的回顾性研究[J]. 上海交通大学学报(医学版), 2023, 43(3): 320-332.
WANG Anjun, LIU Ningning. Efficacy of radiotherapy in patients with rectal cancer undergoing chemotherapy and surgery: a retrospective study based on the SEER database[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2023, 43(3): 320-332.
| Characteristic | Before PSM | After PSM | ||||||
|---|---|---|---|---|---|---|---|---|
All (n=7 070) | S group (n=1 079) | RT+S group (n=5 991) | P value | All (n=1 906) | S group (n=953) | RT+S group (n=953) | P value | |
| Age/n (%) | 0.024 | 0.999 | ||||||
| <50 years | 1 606 (22.7) | 216 (20.0) | 1 390 (23.2) | 371 (19.5) | 185 (19.4) | 186 (19.5) | ||
| ≥50 years | 5 464 (77.3) | 863 (80.0) | 4 601 (76.8) | 1 535 (80.5) | 768 (80.6) | 767 (80.5) | ||
| Gender/n (%) | 0.049 | 0.999 | ||||||
| Male | 4 412 (62.4) | 644 (59.7) | 3 768 (62.9) | 1 129 (59.2) | 564 (59.2) | 565 (59.3) | ||
| Female | 2 658 (37.6) | 435 (40.3) | 2 223 (37.1) | 777 (40.8) | 389 (40.8) | 388 (40.7) | ||
| Race/n (%) | 0.063 | 0.294 | ||||||
| White | 5 414 (76.6) | 818 (75.8) | 4 596 (76.7) | 1 416 (74.3) | 699 (73.3) | 717 (75.2) | ||
| Black | 524 (7.4) | 98 (9.1) | 426 (7.1) | 165 (8.7) | 79 (8.3) | 86 (9.0) | ||
| Others | 1 132 (16.0) | 163 (15.1) | 969 (16.2) | 325 (17.1) | 175 (18.4) | 150 (15.7) | ||
| Marital status/n (%) | 0.681 | 0.541 | ||||||
| Married | 4 183 (59.2) | 645 (59.8) | 3 538 (59.1) | 1 172 (61.5) | 593 (62.2) | 579 (60.8) | ||
| Others | 2 887 (40.8) | 434 (40.2) | 2 453 (40.9) | 734 (38.5) | 360 (37.8) | 374 (39.2) | ||
| Tumor histology/n (%) | 0.000 | 0.956 | ||||||
| Adenocarcinoma | 5 734 (81.1) | 815 (75.5) | 4 919 (82.1) | 1 472 (77.2) | 737 (77.3) | 735 (77.1) | ||
| Others | 1 336 (18.9) | 264 (24.5) | 1 072 (17.9) | 434 (22.8) | 216 (22.7) | 218 (22.9) | ||
| Tumor size/n (%) | 0.010 | 0.999 | ||||||
| ≤30 mm | 1 586 (22.4) | 228 (21.1) | 1 358 (22.7) | 410 (21.5) | 205 (21.5) | 205 (21.5) | ||
| >30‒50 mm | 3 312 (46.8) | 477 (44.2) | 2 835 (47.3) | 878 (46.1) | 439 (46.1) | 439 (46.1) | ||
| >50 mm | 2 172 (30.7) | 374 (34.7) | 1 798 (30.0) | 618 (32.4) | 309 (32.4) | 309 (32.4) | ||
| Histologic grade/n (%) | 0.000 | 0.970 | ||||||
| Well differentiated | 445 (6.3) | 43 (4.0) | 402 (6.7) | 70 (3.7) | 34 (3.6) | 36 (3.8) | ||
| Moderately differentiated | 5 549 (78.5) | 806 (74.7) | 4 743 (79.2) | 1 463 (76.8) | 732 (76.8) | 731 (76.7) | ||
| Poorly differentiated/undifferentiated | 1 076 (15.2) | 230 (21.3) | 846 (14.1) | 373 (19.6) | 187 (19.6) | 186 (19.5) | ||
| TNM stage/n (%) | 0.000 | 0.999 | ||||||
| Ⅰ | 677 (9.6) | 50 (4.6) | 627 (10.5) | 93 (4.9) | 46 (4.8) | 47 (4.9) | ||
| Ⅱ | 2 027 (28.7) | 144 (13.3) | 1 883 (31.4) | 288 (15.1) | 145 (15.2) | 143 (15.0) | ||
| Ⅲ | 3 509 (49.6) | 480 (44.5) | 3 029 (50.6) | 947 (49.7) | 473 (49.6) | 474 (49.7) | ||
| Ⅳ | 857 (12.1) | 405 (37.5) | 452 (7.5) | 578 (30.3) | 289 (30.3) | 289 (30.3) | ||
| Regional nodes examined/n (%) | 0.000 | 0.999 | ||||||
| <12 | 3 065 (43.4) | 411 (38.1) | 2 654 (44.3) | 734 (38.5) | 367 (38.5) | 367 (38.5) | ||
| ≥12 | 4 005 (56.6) | 668 (61.9) | 3 337 (55.7) | 1 172 (61.5) | 586 (61.5) | 586 (61.5) | ||
表1 PSM前后RT+S组和S组直肠癌患者的临床基本特征
Tab 1 Basic characteristics of rectal cancer patients in the RT+S group and the S group before and after PSM
| Characteristic | Before PSM | After PSM | ||||||
|---|---|---|---|---|---|---|---|---|
All (n=7 070) | S group (n=1 079) | RT+S group (n=5 991) | P value | All (n=1 906) | S group (n=953) | RT+S group (n=953) | P value | |
| Age/n (%) | 0.024 | 0.999 | ||||||
| <50 years | 1 606 (22.7) | 216 (20.0) | 1 390 (23.2) | 371 (19.5) | 185 (19.4) | 186 (19.5) | ||
| ≥50 years | 5 464 (77.3) | 863 (80.0) | 4 601 (76.8) | 1 535 (80.5) | 768 (80.6) | 767 (80.5) | ||
| Gender/n (%) | 0.049 | 0.999 | ||||||
| Male | 4 412 (62.4) | 644 (59.7) | 3 768 (62.9) | 1 129 (59.2) | 564 (59.2) | 565 (59.3) | ||
| Female | 2 658 (37.6) | 435 (40.3) | 2 223 (37.1) | 777 (40.8) | 389 (40.8) | 388 (40.7) | ||
| Race/n (%) | 0.063 | 0.294 | ||||||
| White | 5 414 (76.6) | 818 (75.8) | 4 596 (76.7) | 1 416 (74.3) | 699 (73.3) | 717 (75.2) | ||
| Black | 524 (7.4) | 98 (9.1) | 426 (7.1) | 165 (8.7) | 79 (8.3) | 86 (9.0) | ||
| Others | 1 132 (16.0) | 163 (15.1) | 969 (16.2) | 325 (17.1) | 175 (18.4) | 150 (15.7) | ||
| Marital status/n (%) | 0.681 | 0.541 | ||||||
| Married | 4 183 (59.2) | 645 (59.8) | 3 538 (59.1) | 1 172 (61.5) | 593 (62.2) | 579 (60.8) | ||
| Others | 2 887 (40.8) | 434 (40.2) | 2 453 (40.9) | 734 (38.5) | 360 (37.8) | 374 (39.2) | ||
| Tumor histology/n (%) | 0.000 | 0.956 | ||||||
| Adenocarcinoma | 5 734 (81.1) | 815 (75.5) | 4 919 (82.1) | 1 472 (77.2) | 737 (77.3) | 735 (77.1) | ||
| Others | 1 336 (18.9) | 264 (24.5) | 1 072 (17.9) | 434 (22.8) | 216 (22.7) | 218 (22.9) | ||
| Tumor size/n (%) | 0.010 | 0.999 | ||||||
| ≤30 mm | 1 586 (22.4) | 228 (21.1) | 1 358 (22.7) | 410 (21.5) | 205 (21.5) | 205 (21.5) | ||
| >30‒50 mm | 3 312 (46.8) | 477 (44.2) | 2 835 (47.3) | 878 (46.1) | 439 (46.1) | 439 (46.1) | ||
| >50 mm | 2 172 (30.7) | 374 (34.7) | 1 798 (30.0) | 618 (32.4) | 309 (32.4) | 309 (32.4) | ||
| Histologic grade/n (%) | 0.000 | 0.970 | ||||||
| Well differentiated | 445 (6.3) | 43 (4.0) | 402 (6.7) | 70 (3.7) | 34 (3.6) | 36 (3.8) | ||
| Moderately differentiated | 5 549 (78.5) | 806 (74.7) | 4 743 (79.2) | 1 463 (76.8) | 732 (76.8) | 731 (76.7) | ||
| Poorly differentiated/undifferentiated | 1 076 (15.2) | 230 (21.3) | 846 (14.1) | 373 (19.6) | 187 (19.6) | 186 (19.5) | ||
| TNM stage/n (%) | 0.000 | 0.999 | ||||||
| Ⅰ | 677 (9.6) | 50 (4.6) | 627 (10.5) | 93 (4.9) | 46 (4.8) | 47 (4.9) | ||
| Ⅱ | 2 027 (28.7) | 144 (13.3) | 1 883 (31.4) | 288 (15.1) | 145 (15.2) | 143 (15.0) | ||
| Ⅲ | 3 509 (49.6) | 480 (44.5) | 3 029 (50.6) | 947 (49.7) | 473 (49.6) | 474 (49.7) | ||
| Ⅳ | 857 (12.1) | 405 (37.5) | 452 (7.5) | 578 (30.3) | 289 (30.3) | 289 (30.3) | ||
| Regional nodes examined/n (%) | 0.000 | 0.999 | ||||||
| <12 | 3 065 (43.4) | 411 (38.1) | 2 654 (44.3) | 734 (38.5) | 367 (38.5) | 367 (38.5) | ||
| ≥12 | 4 005 (56.6) | 668 (61.9) | 3 337 (55.7) | 1 172 (61.5) | 586 (61.5) | 586 (61.5) | ||
| Characteristic | Before PSM | After PSM | ||||||
|---|---|---|---|---|---|---|---|---|
All (n=2 984) | S group (n=1 079) | S+RT group (n=1 905) | P value | All (n=1 478) | S group (n=739) | S+RT group (n=739) | P value | |
| Age/n (%) | 0.344 | 0.842 | ||||||
| <50 years | 569 (19.1) | 216 (20.0) | 353 (18.5) | 278 (18.8) | 137 (18.5) | 141 (19.1) | ||
| ≥50 years | 2 415 (80.9) | 863 (80.0) | 1 552 (81.5) | 1 200 (81.2) | 602 (81.5) | 598 (80.9) | ||
| Gender/n (%) | 0.473 | 0.874 | ||||||
| Male | 1 754 (58.8) | 644 (59.7) | 1 110 (58.3) | 862 (58.3) | 429 (58.1) | 433 (58.6) | ||
| Female | 1 230 (41.2) | 435 (40.3) | 795 (41.7) | 616 (41.7) | 310 (41.9) | 306 (41.4) | ||
| Race/n (%) | 0.531 | 0.231 | ||||||
| White | 2 274 (76.2) | 818 (75.8) | 1 456 (76.4) | 1 120 (75.8) | 550 (74.4) | 570 (77.1) | ||
| Black | 249 (8.3) | 98 (9.1) | 151 (7.9) | 122 (8.3) | 59 (8.0) | 63 (8.5) | ||
| Others | 461 (15.4) | 163 (15.1) | 298 (15.6) | 236 (16.0) | 130 (17.6) | 106 (14.3) | ||
| Marital status/n (%) | 0.655 | 0.264 | ||||||
| Married | 1 801 (60.4) | 645 (59.8) | 1 156 (60.7) | 892 (60.4) | 435 (58.9) | 457 (61.8) | ||
| Others | 1 183 (39.6) | 434 (40.2) | 749 (39.3) | 586 (39.6) | 304 (41.1) | 282 (38.2) | ||
| Tumor histology/n (%) | 0.012 | 0.859 | ||||||
| Adenocarcinoma | 2 171 (72.8) | 815 (75.5) | 1 356 (71.2) | 1 092 (73.9) | 544 (73.6) | 548 (74.2) | ||
| Others | 813 (27.2) | 264 (24.5) | 549 (28.8) | 386 (26.1) | 195 (26.4) | 191 (25.8) | ||
| Tumor size/n (%) | 0.000 | 0.970 | ||||||
| ≤30 mm | 792 (26.5) | 228 (21.1) | 564 (29.6) | 370 (25.0) | 185 (25.0) | 185 (25.0) | ||
| >30‒50 mm | 1 295 (43.4) | 477 (44.2) | 818 (42.9) | 670 (45.3) | 333 (45.1) | 337 (45.6) | ||
| >50 mm | 897 (30.1) | 374 (34.7) | 523 (27.5) | 438 (29.6) | 221 (29.9) | 217 (29.4) | ||
| Histologic grade/n (%) | 0.008 | 0.999 | ||||||
| Well differentiated | 154 (5.2) | 43 (4.0) | 111 (5.8) | 54 (3.7) | 27 (3.7) | 27 (3.7) | ||
| Moderately differentiated | 2 263 (75.8) | 806 (74.7) | 1 457 (76.5) | 1 154 (78.1) | 577 (78.1) | 577 (78.1) | ||
| Poorly differentiated/undifferentiated | 567 (19.0) | 230 (21.3) | 337 (17.7) | 270 (18.3) | 135 (18.3) | 135 (18.3) | ||
| TNM stage/n (%) | 0.000 | 0.999 | ||||||
| Ⅰ | 309 (10.4) | 50 (4.6) | 259 (13.6) | 82 (5.6) | 41 (5.6) | 41 (5.6) | ||
| Ⅱ | 618 (20.7) | 144 (13.3) | 474 (24.9) | 266 (18.0) | 133 (18.0) | 133 (18.0) | ||
| Ⅲ | 1 533 (51.4) | 480 (44.5) | 1 053 (55.3) | 922 (62.4) | 461 (62.4) | 461 (62.4) | ||
| Ⅳ | 524 (17.6) | 405 (37.5) | 119 (6.3) | 208 (14.1) | 104 (14.1) | 104 (14.1) | ||
| Regional nodes examined/n (%) | 0.799 | 0.999 | ||||||
| <12 | 1 147 (38.4) | 411 (38.1) | 736 (38.6) | 522 (35.3) | 261 (35.3) | 261 (35.3) | ||
| ≥12 | 1 837 (61.6) | 668 (61.9) | 1 169 (61.4) | 956 (64.7) | 478 (64.7) | 478 (64.7) | ||
表2 PSM前后S组和S+RT组直肠癌患者的临床基本特征
Tab 2 Basic characteristics of rectal cancer patients in the S group and the S+RT group before and after PSM
| Characteristic | Before PSM | After PSM | ||||||
|---|---|---|---|---|---|---|---|---|
All (n=2 984) | S group (n=1 079) | S+RT group (n=1 905) | P value | All (n=1 478) | S group (n=739) | S+RT group (n=739) | P value | |
| Age/n (%) | 0.344 | 0.842 | ||||||
| <50 years | 569 (19.1) | 216 (20.0) | 353 (18.5) | 278 (18.8) | 137 (18.5) | 141 (19.1) | ||
| ≥50 years | 2 415 (80.9) | 863 (80.0) | 1 552 (81.5) | 1 200 (81.2) | 602 (81.5) | 598 (80.9) | ||
| Gender/n (%) | 0.473 | 0.874 | ||||||
| Male | 1 754 (58.8) | 644 (59.7) | 1 110 (58.3) | 862 (58.3) | 429 (58.1) | 433 (58.6) | ||
| Female | 1 230 (41.2) | 435 (40.3) | 795 (41.7) | 616 (41.7) | 310 (41.9) | 306 (41.4) | ||
| Race/n (%) | 0.531 | 0.231 | ||||||
| White | 2 274 (76.2) | 818 (75.8) | 1 456 (76.4) | 1 120 (75.8) | 550 (74.4) | 570 (77.1) | ||
| Black | 249 (8.3) | 98 (9.1) | 151 (7.9) | 122 (8.3) | 59 (8.0) | 63 (8.5) | ||
| Others | 461 (15.4) | 163 (15.1) | 298 (15.6) | 236 (16.0) | 130 (17.6) | 106 (14.3) | ||
| Marital status/n (%) | 0.655 | 0.264 | ||||||
| Married | 1 801 (60.4) | 645 (59.8) | 1 156 (60.7) | 892 (60.4) | 435 (58.9) | 457 (61.8) | ||
| Others | 1 183 (39.6) | 434 (40.2) | 749 (39.3) | 586 (39.6) | 304 (41.1) | 282 (38.2) | ||
| Tumor histology/n (%) | 0.012 | 0.859 | ||||||
| Adenocarcinoma | 2 171 (72.8) | 815 (75.5) | 1 356 (71.2) | 1 092 (73.9) | 544 (73.6) | 548 (74.2) | ||
| Others | 813 (27.2) | 264 (24.5) | 549 (28.8) | 386 (26.1) | 195 (26.4) | 191 (25.8) | ||
| Tumor size/n (%) | 0.000 | 0.970 | ||||||
| ≤30 mm | 792 (26.5) | 228 (21.1) | 564 (29.6) | 370 (25.0) | 185 (25.0) | 185 (25.0) | ||
| >30‒50 mm | 1 295 (43.4) | 477 (44.2) | 818 (42.9) | 670 (45.3) | 333 (45.1) | 337 (45.6) | ||
| >50 mm | 897 (30.1) | 374 (34.7) | 523 (27.5) | 438 (29.6) | 221 (29.9) | 217 (29.4) | ||
| Histologic grade/n (%) | 0.008 | 0.999 | ||||||
| Well differentiated | 154 (5.2) | 43 (4.0) | 111 (5.8) | 54 (3.7) | 27 (3.7) | 27 (3.7) | ||
| Moderately differentiated | 2 263 (75.8) | 806 (74.7) | 1 457 (76.5) | 1 154 (78.1) | 577 (78.1) | 577 (78.1) | ||
| Poorly differentiated/undifferentiated | 567 (19.0) | 230 (21.3) | 337 (17.7) | 270 (18.3) | 135 (18.3) | 135 (18.3) | ||
| TNM stage/n (%) | 0.000 | 0.999 | ||||||
| Ⅰ | 309 (10.4) | 50 (4.6) | 259 (13.6) | 82 (5.6) | 41 (5.6) | 41 (5.6) | ||
| Ⅱ | 618 (20.7) | 144 (13.3) | 474 (24.9) | 266 (18.0) | 133 (18.0) | 133 (18.0) | ||
| Ⅲ | 1 533 (51.4) | 480 (44.5) | 1 053 (55.3) | 922 (62.4) | 461 (62.4) | 461 (62.4) | ||
| Ⅳ | 524 (17.6) | 405 (37.5) | 119 (6.3) | 208 (14.1) | 104 (14.1) | 104 (14.1) | ||
| Regional nodes examined/n (%) | 0.799 | 0.999 | ||||||
| <12 | 1 147 (38.4) | 411 (38.1) | 736 (38.6) | 522 (35.3) | 261 (35.3) | 261 (35.3) | ||
| ≥12 | 1 837 (61.6) | 668 (61.9) | 1 169 (61.4) | 956 (64.7) | 478 (64.7) | 478 (64.7) | ||
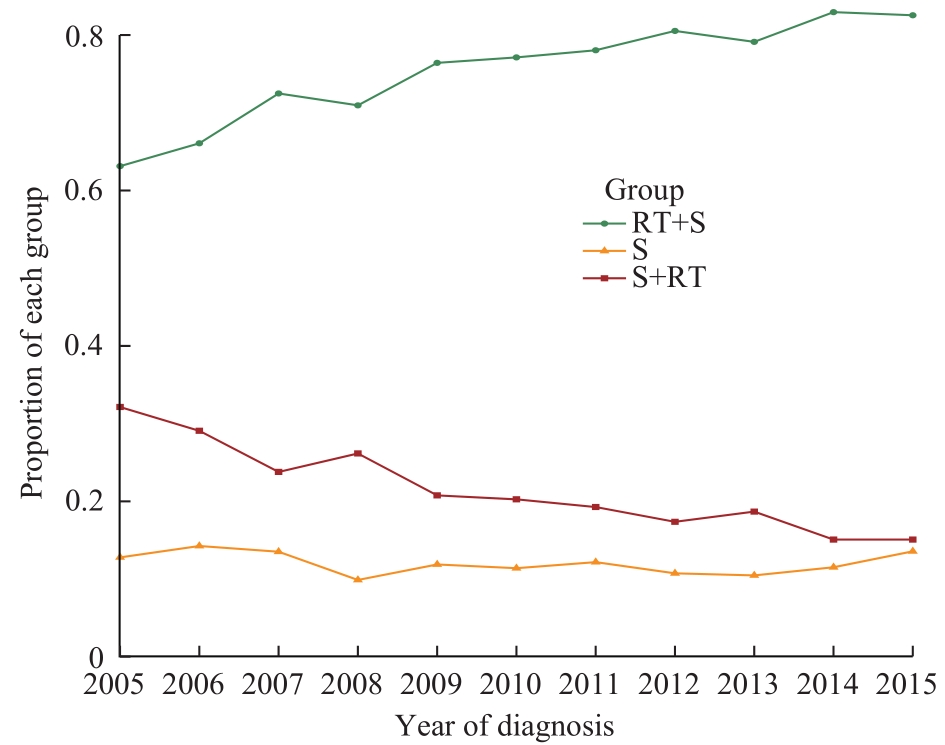
图2 2005—2015年接受化疗和手术的3组直肠癌患者的比例变化趋势
Fig 2 Trends in the proportions of rectal cancer patients in three groups receiving chemotherapy from 2005 to 2015
| Test model | Before PSM | After PSM | ||||
|---|---|---|---|---|---|---|
RT+S group (95%CI) | S group (95%CI) | P value | RT+S group (95%CI) | S group (95%CI) | P value | |
| Log-rank | ||||||
| Median OS/month | 149 (142‒155) | 62 (55‒72) | ‒ | 104 (93‒123) | 71 (61‒86) | ‒ |
| Median CSS/month | NA | 79 (66‒107) | ‒ | NA | 107 (81‒142) | ‒ |
| RMST | ||||||
| 60 months (5 years) survival time | 52.9 (52.5‒53.3) | 44.2 (43.0‒45.3) | 0.000 | 49.8 (48.8‒50.8) | 45.4 (44.2‒46.6) | 0.000 |
| 60 months (5 years) cancer specific survival time | 54.1 (53.8‒54.5) | 45.9 (44.8‒47.0) | 0.000 | 50.8 (49.8‒51.8) | 47.3 (46.1‒48.5) | 0.000 |
| 120 months (10 years) survival time | 91.7 (90.6‒92.7) | 70.1 (67.3‒72.8) | 0.000 | 82.1 (79.4‒84.9) | 73.2 (70.2‒76.1) | 0.000 |
| 120 months (10 years) cancer specific survival time | 97.4 (96.4‒98.4) | 75.2 (72.4‒78.1) | 0.000 | 87.1 (84.4‒89.9) | 78.7 (75.7‒81.8) | 0.000 |
表3 RT+S组和S组直肠癌患者OS和CSS比较
Tab 3 Comparison of OS and CSS in the patients with rectal cancer between the RT+S group and the S group
| Test model | Before PSM | After PSM | ||||
|---|---|---|---|---|---|---|
RT+S group (95%CI) | S group (95%CI) | P value | RT+S group (95%CI) | S group (95%CI) | P value | |
| Log-rank | ||||||
| Median OS/month | 149 (142‒155) | 62 (55‒72) | ‒ | 104 (93‒123) | 71 (61‒86) | ‒ |
| Median CSS/month | NA | 79 (66‒107) | ‒ | NA | 107 (81‒142) | ‒ |
| RMST | ||||||
| 60 months (5 years) survival time | 52.9 (52.5‒53.3) | 44.2 (43.0‒45.3) | 0.000 | 49.8 (48.8‒50.8) | 45.4 (44.2‒46.6) | 0.000 |
| 60 months (5 years) cancer specific survival time | 54.1 (53.8‒54.5) | 45.9 (44.8‒47.0) | 0.000 | 50.8 (49.8‒51.8) | 47.3 (46.1‒48.5) | 0.000 |
| 120 months (10 years) survival time | 91.7 (90.6‒92.7) | 70.1 (67.3‒72.8) | 0.000 | 82.1 (79.4‒84.9) | 73.2 (70.2‒76.1) | 0.000 |
| 120 months (10 years) cancer specific survival time | 97.4 (96.4‒98.4) | 75.2 (72.4‒78.1) | 0.000 | 87.1 (84.4‒89.9) | 78.7 (75.7‒81.8) | 0.000 |
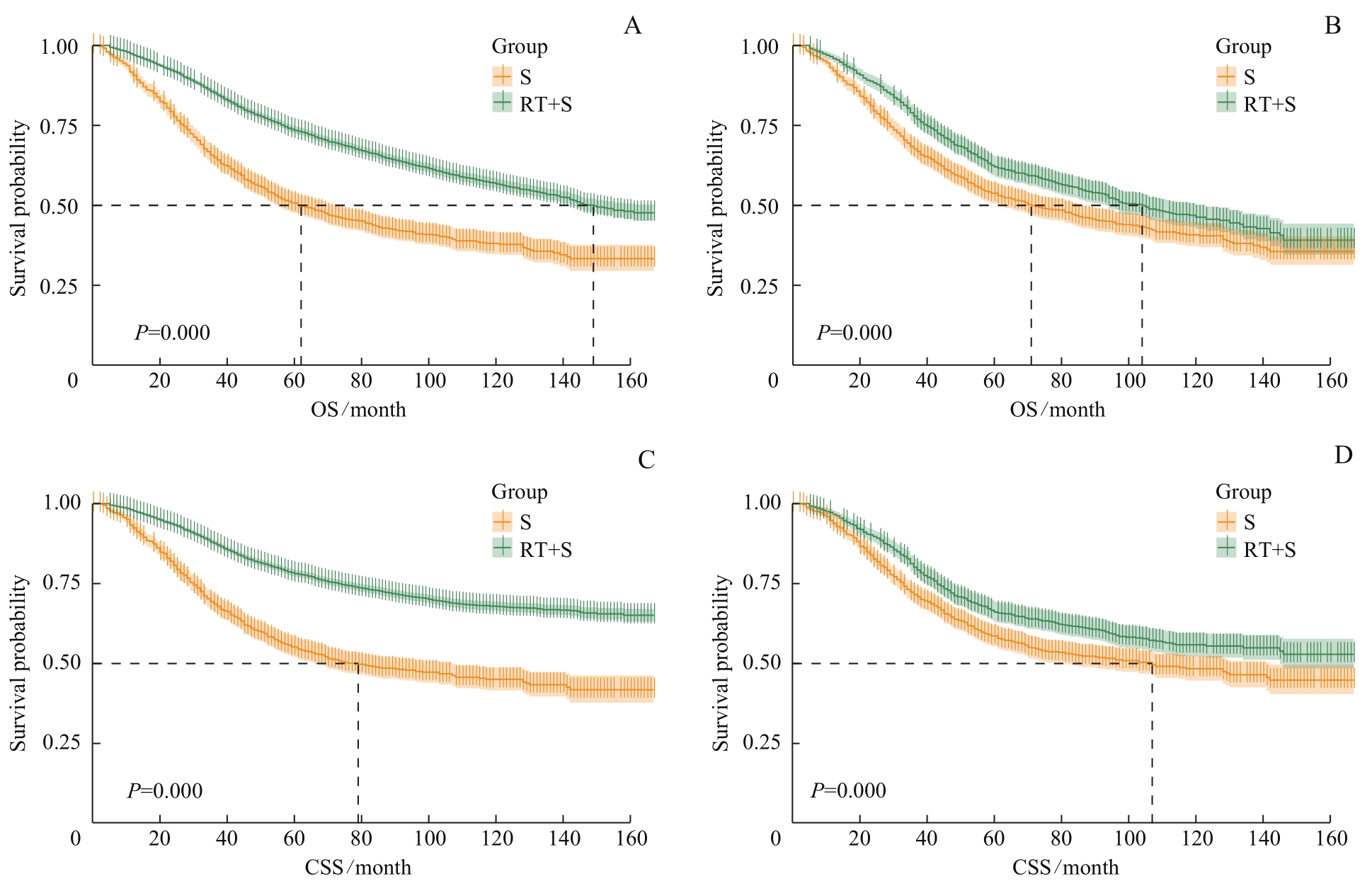
图3 PSM前后RT+S组和S组的生存曲线Note: A. Survival curves of OS of the RT+S group and the S group before PSM. B. Survival curves of OS of the RT+S group and the S group after PSM. C. Survival curves of CSS of the RT+S group and the S group before PSM. D. Survival curves of CSS of the RT+S group and the S group after PSM.
Fig 3 Survival curves of the RT+S group and the S group before and after PSM
| Test model | Before PSM | After PSM | ||||
|---|---|---|---|---|---|---|
S group (95%CI) | S+RT group (95%CI) | P value | S group (95%CI) | S+RT group (95%CI) | P value | |
| Log-rank | ||||||
| Median OS/month | 62 (55‒72) | 142 (129‒155) | ‒ | 106 (88‒129) | 116 (98‒132) | ‒ |
| Median CSS/month | 79 (66‒107) | NA | ‒ | NA | NA | ‒ |
| RMST | ||||||
| 60 months (5 years) survival time | 44.2 (43.0‒45.3) | 52.2 (51.5‒52.9) | 0.000 | 48.0 (46.7‒49.4) | 50.6 (49.4‒51.7) | 0.005 |
60 months (5 years) cancer specific survival time | 45.9 (44.8‒47.0) | 53.8 (53.2‒54.5) | 0.000 | 49.9 (48.7‒51.2) | 51.7 (50.6‒52.9) | 0.033 |
| 120 months (10 years) survival time | 70.1 (67.3‒72.8) | 90.3 (88.5‒92.1) | 0.000 | 80.3 (77.0‒83.6) | 84.6 (81.5‒87.6) | 0.065 |
120 months (10 years) cancer specific survival time | 75.2 (72.4‒78.1) | 96.6 (94.8‒98.3) | 0.000 | 86.3 (83.0‒89.6) | 89.6 (86.6‒92.7) | 0.147 |
表4 S组和S+RT组直肠癌患者OS和CSS比较
Tab 4 Comparison of OS and CSS in the patients with rectal cancer between the S group and the S+RT group
| Test model | Before PSM | After PSM | ||||
|---|---|---|---|---|---|---|
S group (95%CI) | S+RT group (95%CI) | P value | S group (95%CI) | S+RT group (95%CI) | P value | |
| Log-rank | ||||||
| Median OS/month | 62 (55‒72) | 142 (129‒155) | ‒ | 106 (88‒129) | 116 (98‒132) | ‒ |
| Median CSS/month | 79 (66‒107) | NA | ‒ | NA | NA | ‒ |
| RMST | ||||||
| 60 months (5 years) survival time | 44.2 (43.0‒45.3) | 52.2 (51.5‒52.9) | 0.000 | 48.0 (46.7‒49.4) | 50.6 (49.4‒51.7) | 0.005 |
60 months (5 years) cancer specific survival time | 45.9 (44.8‒47.0) | 53.8 (53.2‒54.5) | 0.000 | 49.9 (48.7‒51.2) | 51.7 (50.6‒52.9) | 0.033 |
| 120 months (10 years) survival time | 70.1 (67.3‒72.8) | 90.3 (88.5‒92.1) | 0.000 | 80.3 (77.0‒83.6) | 84.6 (81.5‒87.6) | 0.065 |
120 months (10 years) cancer specific survival time | 75.2 (72.4‒78.1) | 96.6 (94.8‒98.3) | 0.000 | 86.3 (83.0‒89.6) | 89.6 (86.6‒92.7) | 0.147 |

图4 PSM前后S组和S+RT组的生存曲线Note: A. Survival curves of OS of the S group and the S+RT group before PSM. B. Survival curves of OS of the S group and the S+RT group after PSM. C. Survival curves of CSS of the S group and the S+RT group before PSM. D. Survival curves of CSS of the S group and the S+RT group after PSM.
Fig 4 Survival curves of the S group and the S+RT group before and after PSM
| Factor | OS | CSS | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | Univariate analysis | Multivariate analysis | |||||
| HR (95%CI) | P value | HR (95%CI) | P value | HR (95%CI) | P value | HR (95%CI) | P value | |
| Group | ||||||||
| S | Reference | Reference | Reference | Reference | ||||
| RT+S | 0.77 (0.68‒0.88) | 0.000 | 0.73 (0.64‒0.83) | 0.000 | 0.75 (0.65‒0.87) | 0.000 | 0.71 (0.62‒0.82) | 0.000 |
| Age | ||||||||
| <50 years | Reference | Reference | Reference | |||||
| ≥50 years | 1.37 (1.15‒1.63) | 0.000 | 1.47 (1.23‒1.75) | 0.000 | 1.14 (0.95‒1.37) | 0.144 | ||
| Gender | ||||||||
| Male | Reference | Reference | ||||||
| Female | 0.90 (0.79‒1.02) | 0.107 | 0.89 (0.77‒1.03) | 0.120 | ||||
| Race | ||||||||
| White | Reference | Reference | Reference | Reference | ||||
| Black | 1.32 (1.07‒1.62) | 0.010 | 1.27 (1.03‒1.57) | 0.025 | 1.43 (1.15‒1.79) | 0.002 | 1.38 (1.10‒1.73) | 0.005 |
| Others | 0.96 (0.80‒1.14) | 0.623 | 1.03 (0.86‒1.23) | 0.733 | 0.96 (0.79‒1.16) | 0.659 | 1.02 (0.84‒1.24) | 0.858 |
| Marital status | ||||||||
| Married | Reference | Reference | Reference | Reference | ||||
| Others | 1.31 (1.15‒1.49) | 0.000 | 1.27 (1.11‒1.44) | 0.000 | 1.30 (1.13‒1.50) | 0.000 | 1.27 (1.10‒1.46) | 0.001 |
| Tumor histology | ||||||||
| Adenocarcinoma | Reference | Reference | ||||||
| Others | 0.96 (0.82‒1.12) | 0.598 | 0.95 (0.80‒1.13) | 0.572 | ||||
| Tumor size | ||||||||
| ≤30 mm | Reference | Reference | Reference | Reference | ||||
| >30‒50 mm | 1.54 (1.29‒1.85) | 0.000 | 1.30 (1.08‒1.57) | 0.007 | 1.59 (1.29‒1.95) | 0.000 | 1.26 (1.02‒1.56) | 0.035 |
| >50 mm | 1.96 (1.62‒2.37) | 0.000 | 1.60 (1.32‒1.95) | 0.000 | 2.13 (1.72‒2.63) | 0.000 | 1.56 (1.26‒1.95) | 0.000 |
| Histologic grade | ||||||||
| Well differentiated | Reference | Reference | Reference | Reference | ||||
| Moderately differentiated | 1.18 (0.81‒1.72) | 0.388 | 1.04 (0.71‒1.52) | 0.834 | 1.26 (0.82‒1.95) | 0.292 | 1.06 (0.68‒1.64) | 0.802 |
| Poorly differentiated/ undifferentiated | 2.03 (1.37‒3.00) | 0.000 | 1.81 (1.22‒2.69) | 0.003 | 2.34 (1.50‒3.67) | 0.000 | 1.98 (1.26‒3.11) | 0.003 |
| TNM stage | ||||||||
| Ⅰ | Reference | Reference | Reference | Reference | ||||
| Ⅱ | 0.86 (0.59‒1.26) | 0.443 | 0.73 (0.49‒1.08) | 0.112 | 0.96 (0.60‒1.54) | 0.881 | 0.85 (0.53‒1.37) | 0.502 |
| Ⅲ | 1.24 (0.89‒1.74) | 0.209 | 1.03 (0.73‒1.46) | 0.852 | 1.41 (0.93‒2.14) | 0.107 | 1.20 (0.79‒1.83) | 0.398 |
| Ⅳ | 3.70 (2.64‒5.19) | 0.000 | 3.05 (2.16‒4.32) | 0.000 | 4.91 (3.25‒7.43) | 0.000 | 4.17 (2.73‒6.36) | 0.000 |
| Regional nodes examined | ||||||||
| <12 | Reference | Reference | ||||||
| ≥12 | 0.90 (0.79‒1.02) | 0.099 | 0.96 (0.83‒1.10) | 0.539 | ||||
表5 RT+S组和S组直肠癌患者OS和CSS的单因素和多因素Cox回归分析
Tab 5 Univariate and multivariate Cox regression analysis of OS and CSS of rectal cancer patients between the RT+S group and the S group
| Factor | OS | CSS | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | Univariate analysis | Multivariate analysis | |||||
| HR (95%CI) | P value | HR (95%CI) | P value | HR (95%CI) | P value | HR (95%CI) | P value | |
| Group | ||||||||
| S | Reference | Reference | Reference | Reference | ||||
| RT+S | 0.77 (0.68‒0.88) | 0.000 | 0.73 (0.64‒0.83) | 0.000 | 0.75 (0.65‒0.87) | 0.000 | 0.71 (0.62‒0.82) | 0.000 |
| Age | ||||||||
| <50 years | Reference | Reference | Reference | |||||
| ≥50 years | 1.37 (1.15‒1.63) | 0.000 | 1.47 (1.23‒1.75) | 0.000 | 1.14 (0.95‒1.37) | 0.144 | ||
| Gender | ||||||||
| Male | Reference | Reference | ||||||
| Female | 0.90 (0.79‒1.02) | 0.107 | 0.89 (0.77‒1.03) | 0.120 | ||||
| Race | ||||||||
| White | Reference | Reference | Reference | Reference | ||||
| Black | 1.32 (1.07‒1.62) | 0.010 | 1.27 (1.03‒1.57) | 0.025 | 1.43 (1.15‒1.79) | 0.002 | 1.38 (1.10‒1.73) | 0.005 |
| Others | 0.96 (0.80‒1.14) | 0.623 | 1.03 (0.86‒1.23) | 0.733 | 0.96 (0.79‒1.16) | 0.659 | 1.02 (0.84‒1.24) | 0.858 |
| Marital status | ||||||||
| Married | Reference | Reference | Reference | Reference | ||||
| Others | 1.31 (1.15‒1.49) | 0.000 | 1.27 (1.11‒1.44) | 0.000 | 1.30 (1.13‒1.50) | 0.000 | 1.27 (1.10‒1.46) | 0.001 |
| Tumor histology | ||||||||
| Adenocarcinoma | Reference | Reference | ||||||
| Others | 0.96 (0.82‒1.12) | 0.598 | 0.95 (0.80‒1.13) | 0.572 | ||||
| Tumor size | ||||||||
| ≤30 mm | Reference | Reference | Reference | Reference | ||||
| >30‒50 mm | 1.54 (1.29‒1.85) | 0.000 | 1.30 (1.08‒1.57) | 0.007 | 1.59 (1.29‒1.95) | 0.000 | 1.26 (1.02‒1.56) | 0.035 |
| >50 mm | 1.96 (1.62‒2.37) | 0.000 | 1.60 (1.32‒1.95) | 0.000 | 2.13 (1.72‒2.63) | 0.000 | 1.56 (1.26‒1.95) | 0.000 |
| Histologic grade | ||||||||
| Well differentiated | Reference | Reference | Reference | Reference | ||||
| Moderately differentiated | 1.18 (0.81‒1.72) | 0.388 | 1.04 (0.71‒1.52) | 0.834 | 1.26 (0.82‒1.95) | 0.292 | 1.06 (0.68‒1.64) | 0.802 |
| Poorly differentiated/ undifferentiated | 2.03 (1.37‒3.00) | 0.000 | 1.81 (1.22‒2.69) | 0.003 | 2.34 (1.50‒3.67) | 0.000 | 1.98 (1.26‒3.11) | 0.003 |
| TNM stage | ||||||||
| Ⅰ | Reference | Reference | Reference | Reference | ||||
| Ⅱ | 0.86 (0.59‒1.26) | 0.443 | 0.73 (0.49‒1.08) | 0.112 | 0.96 (0.60‒1.54) | 0.881 | 0.85 (0.53‒1.37) | 0.502 |
| Ⅲ | 1.24 (0.89‒1.74) | 0.209 | 1.03 (0.73‒1.46) | 0.852 | 1.41 (0.93‒2.14) | 0.107 | 1.20 (0.79‒1.83) | 0.398 |
| Ⅳ | 3.70 (2.64‒5.19) | 0.000 | 3.05 (2.16‒4.32) | 0.000 | 4.91 (3.25‒7.43) | 0.000 | 4.17 (2.73‒6.36) | 0.000 |
| Regional nodes examined | ||||||||
| <12 | Reference | Reference | ||||||
| ≥12 | 0.90 (0.79‒1.02) | 0.099 | 0.96 (0.83‒1.10) | 0.539 | ||||
| Factor | OS | CSS | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | Univariate analysis | Multivariate analysis | |||||
| HR (95%CI) | P value | HR (95%CI) | P value | HR (95%CI) | P value | HR (95%CI) | P value | |
| Group | ||||||||
| S | Reference | Reference | ||||||
| S+RT | 1.12 (0.96‒1.30) | 0.150 | 1.13 (0.95‒1.34) | 0.166 | ||||
| Age | ||||||||
| <50 years | Reference | Reference | Reference | Reference | ||||
| ≥50 years | 1.55 (1.25‒1.92) | 0.000 | 1.82 (1.46‒2.26) | 0.000 | 1.30 (1.04‒1.64) | 0.024 | 1.81 (1.45‒2.24) | 0.000 |
| Gender | ||||||||
| Male | Reference | Reference | ||||||
| Female | 0.98 (0.84‒1.14) | 0.750 | 1.00 (0.84‒1.19) | 0.992 | ||||
| Race | ||||||||
| White | Reference | Reference | Reference | |||||
| Black | 1.30 (1.01‒1.67) | 0.045 | 1.35 (1.04‒1.75) | 0.024 | 1.25 (0.94‒1.67) | 0.125 | ||
| Others | 0.81 (0.65‒1.01) | 0.065 | 0.99 (0.79‒1.24) | 0.914 | 0.81 (0.63‒1.04) | 0.101 | ||
| Marital status | ||||||||
| Married | Reference | Reference | Reference | Reference | ||||
| Others | 1.43 (1.23‒1.67) | 0.000 | 1.35 (1.16‒1.58) | 0.000 | 1.42 (1.19‒1.68) | 0.000 | 1.39 (1.19‒1.62) | 0.000 |
| Tumor histology | ||||||||
| Adenocarcinoma | Reference | Reference | ||||||
| Others | 1.07 (0.90‒1.27) | 0.426 | 1.14 (0.94‒1.38) | 0.185 | ||||
| Tumor size | ||||||||
| ≤30 mm | Reference | Reference | Reference | Reference | ||||
| >30‒50 mm | 1.78 (1.44‒2.21) | 0.000 | 1.64 (1.32‒2.05) | 0.000 | 1.90 (1.48‒2.43) | 0.000 | 1.64 (1.32‒2.05) | 0.000 |
| >50 mm | 2.15 (1.72‒2.70) | 0.000 | 2.01 (1.59‒2.54) | 0.000 | 2.41 (1.86‒3.12) | 0.000 | 2.02 (1.60‒2.56) | 0.000 |
| Histologic grade | ||||||||
| Well differentiated | Reference | Reference | Reference | Reference | ||||
| Moderately differentiated | 0.94 (0.62‒1.44) | 0.790 | 0.88 (0.58‒1.34) | 0.549 | 1.08 (0.65‒1.78) | 0.771 | 0.89 (0.58‒1.35) | 0.574 |
| Poorly differentiated/ undifferentiated | 1.58 (1.02‒2.45) | 0.041 | 1.38 (0.89‒2.16) | 0.150 | 1.86 (1.11‒3.13) | 0.019 | 1.40 (0.90‒2.17) | 0.139 |
| TNM stage | ||||||||
| Ⅰ | Reference | Reference | Reference | Reference | ||||
| Ⅱ | 1.11 (0.72‒1.70) | 0.635 | 0.78 (0.50‒1.22) | 0.280 | 1.48 (0.86‒2.55) | 0.160 | 0.76 (0.49‒1.19) | 0.232 |
| Ⅲ | 1.45 (0.98‒2.12) | 0.060 | 1.10 (0.74‒1.64) | 0.634 | 1.88 (1.14‒3.12) | 0.014 | 1.07 (0.72‒1.58) | 0.753 |
| Ⅳ | 4.67 (3.13‒6.98) | 0.000 | 3.54 (2.33‒5.38) | 0.000 | 7.30 (4.36‒12.23) | 0.000 | 3.39 (2.24‒5.15) | 0.000 |
| Regional nodes examined | ||||||||
| <12 | Reference | Reference | ||||||
| ≥12 | 0.89 (0.76‒1.04) | 0.137 | 0.99 (0.83‒1.18) | 0.894 | ||||
表6 S组和S+RT组直肠癌患者OS和CSS的单因素和多因素Cox回归分析
Tab 6 Univariate and multivariate Cox regression analysis of OS and CSS of rectal cancer patients between the S group and the S+RT group
| Factor | OS | CSS | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | Univariate analysis | Multivariate analysis | |||||
| HR (95%CI) | P value | HR (95%CI) | P value | HR (95%CI) | P value | HR (95%CI) | P value | |
| Group | ||||||||
| S | Reference | Reference | ||||||
| S+RT | 1.12 (0.96‒1.30) | 0.150 | 1.13 (0.95‒1.34) | 0.166 | ||||
| Age | ||||||||
| <50 years | Reference | Reference | Reference | Reference | ||||
| ≥50 years | 1.55 (1.25‒1.92) | 0.000 | 1.82 (1.46‒2.26) | 0.000 | 1.30 (1.04‒1.64) | 0.024 | 1.81 (1.45‒2.24) | 0.000 |
| Gender | ||||||||
| Male | Reference | Reference | ||||||
| Female | 0.98 (0.84‒1.14) | 0.750 | 1.00 (0.84‒1.19) | 0.992 | ||||
| Race | ||||||||
| White | Reference | Reference | Reference | |||||
| Black | 1.30 (1.01‒1.67) | 0.045 | 1.35 (1.04‒1.75) | 0.024 | 1.25 (0.94‒1.67) | 0.125 | ||
| Others | 0.81 (0.65‒1.01) | 0.065 | 0.99 (0.79‒1.24) | 0.914 | 0.81 (0.63‒1.04) | 0.101 | ||
| Marital status | ||||||||
| Married | Reference | Reference | Reference | Reference | ||||
| Others | 1.43 (1.23‒1.67) | 0.000 | 1.35 (1.16‒1.58) | 0.000 | 1.42 (1.19‒1.68) | 0.000 | 1.39 (1.19‒1.62) | 0.000 |
| Tumor histology | ||||||||
| Adenocarcinoma | Reference | Reference | ||||||
| Others | 1.07 (0.90‒1.27) | 0.426 | 1.14 (0.94‒1.38) | 0.185 | ||||
| Tumor size | ||||||||
| ≤30 mm | Reference | Reference | Reference | Reference | ||||
| >30‒50 mm | 1.78 (1.44‒2.21) | 0.000 | 1.64 (1.32‒2.05) | 0.000 | 1.90 (1.48‒2.43) | 0.000 | 1.64 (1.32‒2.05) | 0.000 |
| >50 mm | 2.15 (1.72‒2.70) | 0.000 | 2.01 (1.59‒2.54) | 0.000 | 2.41 (1.86‒3.12) | 0.000 | 2.02 (1.60‒2.56) | 0.000 |
| Histologic grade | ||||||||
| Well differentiated | Reference | Reference | Reference | Reference | ||||
| Moderately differentiated | 0.94 (0.62‒1.44) | 0.790 | 0.88 (0.58‒1.34) | 0.549 | 1.08 (0.65‒1.78) | 0.771 | 0.89 (0.58‒1.35) | 0.574 |
| Poorly differentiated/ undifferentiated | 1.58 (1.02‒2.45) | 0.041 | 1.38 (0.89‒2.16) | 0.150 | 1.86 (1.11‒3.13) | 0.019 | 1.40 (0.90‒2.17) | 0.139 |
| TNM stage | ||||||||
| Ⅰ | Reference | Reference | Reference | Reference | ||||
| Ⅱ | 1.11 (0.72‒1.70) | 0.635 | 0.78 (0.50‒1.22) | 0.280 | 1.48 (0.86‒2.55) | 0.160 | 0.76 (0.49‒1.19) | 0.232 |
| Ⅲ | 1.45 (0.98‒2.12) | 0.060 | 1.10 (0.74‒1.64) | 0.634 | 1.88 (1.14‒3.12) | 0.014 | 1.07 (0.72‒1.58) | 0.753 |
| Ⅳ | 4.67 (3.13‒6.98) | 0.000 | 3.54 (2.33‒5.38) | 0.000 | 7.30 (4.36‒12.23) | 0.000 | 3.39 (2.24‒5.15) | 0.000 |
| Regional nodes examined | ||||||||
| <12 | Reference | Reference | ||||||
| ≥12 | 0.89 (0.76‒1.04) | 0.137 | 0.99 (0.83‒1.18) | 0.894 | ||||
| 1 | SUNG H, FERLAY J, SIEGEL R L, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71(3): 209-249. |
| 2 | ZHENG R S, ZHANG S W, ZENG H M, et al. Cancer incidence and mortality in China, 2016[J]. J Natl Cancer Cent, 2022, 2(1): 1-9. |
| 3 | BENSON A B, VENOOK A P, AL-HAWARY M M, et al. NCCN guidelines insights: colon cancer, version 2.2018[J]. J Natl Compr Canc Netw, 2018, 16(4): 359-369. |
| 4 | ROH M S, COLANGELO L H, O′CONNELL M J, et al. Preoperative multimodality therapy improves disease-free survival in patients with carcinoma of the rectum: NSABP R-03[J]. J Clin Oncol, 2009, 27(31): 5124-5130. |
| 5 | Colorectal Cancer Collaborative Group. Adjuvant radiotherapy for rectal cancer: a systematic overview of 8,507 patients from 22 randomised trials[J]. Lancet, 2001, 358(9290): 1291-1304. |
| 6 | MA B, GAO P, WANG H C, et al. What has preoperative radio(chemo)therapy brought to localized rectal cancer patients in terms of perioperative and long-term outcomes over the past decades? A systematic review and meta-analysis based on 41,121 patients[J]. Int J Cancer, 2017, 141(5): 1052-1065. |
| 7 | ZHONG W, XUE X J, DAI L Z, et al. Neoadjuvant treatments for resectable rectal cancer: a network meta-analysis[J]. Exp Ther Med, 2020, 19(4): 2604-2614. |
| 8 | MARTIN S T, HENEGHAN H M, WINTER D C. Systematic review and meta-analysis of outcomes following pathological complete response to neoadjuvant chemoradiotherapy for rectal cancer[J]. Br J Surg, 2012, 99(7): 918-928. |
| 9 | TRINQUART L, JACOT J, CONNER S C, et al. Comparison of treatment effects measured by the hazard ratio and by the ratio of restricted mean survival times in oncology randomized controlled trials[J]. J Clin Oncol, 2016, 34(15): 1813-1819. |
| 10 | WOLSKI A, GRAFFÉO N, GIORGI R, et al. A permutation test based on the restricted mean survival time for comparison of net survival distributions in non-proportional excess hazard settings[J]. Stat Methods Med Res, 2020, 29(6): 1612-1623. |
| 11 | IRWIN J O. The standard error of an estimate of expectation of life, with special reference to expectation of tumourless life in experiments with mice[J]. J Hyg (Lond), 1949, 47(2): 188. |
| 12 | MAAS M, NELEMANS P J, VALENTINI V, et al. Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: a pooled analysis of individual patient data[J]. Lancet Oncol, 2010, 11(9): 835-844. |
| 13 | PARK I J, YOU Y N, AGARWAL A, et al. Neoadjuvant treatment response as an early response indicator for patients with rectal cancer[J]. J Clin Oncol, 2012, 30(15): 1770-1776. |
| 14 | ARENAS PRAT M, SABATER S, BONET M, et al. EP-2303: should radiotherapy be avoided after neoadjuvant chemotherapy in complete response breast cancer?[J]. Radiother Oncol, 2018, 127: S1271. |
| 15 | LOGAN J K, HUBER K E, DIPETRILLO T A, et al. Patterns of care of radiation therapy in patients with stage Ⅳ rectal cancer: a Surveillance, Epidemiology, and End Results analysis of patients from 2004 to 2009[J]. Cancer, 2014, 120(5): 731-737. |
| 16 | BUJKO K, PARTYCKI M, PIETRZAK L. Neoadjuvant radiotherapy (5×5 Gy): immediate versus delayed surgery[J]. Recent Results Cancer Res, 2014, 203: 171-187. |
| 17 | BACH S P, GILBERT A, BROCK K, et al. Radical surgery versus organ preservation via short-course radiotherapy followed by transanal endoscopic microsurgery for early-stage rectal cancer (TREC): a randomised, open-label feasibility study[J]. Lancet Gastroenterol Hepatol, 2021, 6(2): 92-105. |
| 18 | HAYES I P, MILANZI E, GIBBS P, et al. Neoadjuvant chemoradiotherapy and tumor recurrence in patients with early T-stage cancer of the lower rectum[J]. Ann Surg Oncol, 2020, 27(5): 1570-1579. |
| 19 | MCLAUGHLIN C, KIM N K, BANDYOPADHYAY D, et al. Adjuvant radiation therapy for T4 non-rectal colon adenocarcinoma provides a cause-specific survival advantage: a SEER database analysis[J]. Radiother Oncol, 2019, 133: 50-53. |
| 20 | HUANG Y, GU X, GE K X, et al. The survival benefit of adjuvant radiotherapy for pathological T4N2M0 colon cancer in the Modern Chemotherapy Era: evidence from the SEER database 2004‒2015[J]. Artif Cells Nanomed Biotechnol, 2020, 48(1): 834-840. |
| 21 | SIEGEL R L, JEMAL A, WARD E M. Increase in incidence of colorectal cancer among young men and women in the United States[J]. Cancer Epidemiol Biomarkers Prev, 2009, 18(6): 1695-1698. |
| 22 | WANG L, ZHONG X H, LIN H Q, et al. Identifying the long-term survival beneficiary of preoperative radiotherapy for rectal cancer in the TME era[J]. Sci Rep, 2022, 12(1): 4617. |
| 23 | KOLARICH A, GEORGE T J Jr, HUGHES S J, et al. Rectal cancer patients younger than 50 years lack a survival benefit from NCCN guideline-directed treatment for stage Ⅱ and Ⅲ disease[J]. Cancer, 2018, 124(17): 3510-3519. |
| 24 | STEINHAGEN E, SHIA, RIEDEL E, et al. Response to neoadjuvant therapy in patients with early age-of-onset rectal cancer[J]. Dis Colon Rectum, 2013, 56(1): 58-63. |
| 25 | ZHANG Y Y, YAN L L, WU Y, et al. Worse treatment response to neoadjuvant chemoradiotherapy in young patients with locally advanced rectal cancer[J]. BMC Cancer, 2020, 20(1): 854. |
| 26 | LEE S, MA C, ZHANG S, et al. Marital status, living arrangement, and cancer recurrence and survival in patients with stage Ⅲ colon cancer: findings from CALGB 89803 (Alliance)[J]. Oncologist, 2022, 27(6): e494-e505. |
| [1] | 何嘉音, 陈思远, 施晴, 张慕晨, 易红梅, 董磊, 钱樱, 王黎, 程澍, 许彭鹏, 赵维莅. 肾上腺累及的弥漫性大B细胞淋巴瘤患者临床病理特征、基因突变谱及预后分析[J]. 上海交通大学学报(医学版), 2025, 45(9): 1194-1201. |
| [2] | 陈思远, 施晴, 付迪, 王黎, 程澍, 许彭鹏, 赵维莅. 肺受累弥漫大B细胞淋巴瘤临床病理特征、基因突变谱及预后分析[J]. 上海交通大学学报(医学版), 2025, 45(9): 1214-1220. |
| [3] | 江怡, 黄晨浩, 李祉良, 吴珺玮, 赵任, 张弢. 1例KRAS突变的结直肠癌患者术前接受化疗联合免疫治疗的效果报道[J]. 上海交通大学学报(医学版), 2025, 45(9): 1256-1260. |
| [4] | 严治, 吴星玥, 姚卫芹, 颜灵芝, 金松, 商京晶, 施晓兰, 吴德沛, 傅琤琤. 免疫不全麻痹在新诊断多发性骨髓瘤患者中的动态变化及预后意义[J]. 上海交通大学学报(医学版), 2025, 45(7): 807-814. |
| [5] | 李卓杭, 于新迪, 任婧雅, 沈佳, 董素贞, 王伟. 主动脉缩窄端侧吻合纠治术后的神经系统预后分析[J]. 上海交通大学学报(医学版), 2025, 45(6): 753-759. |
| [6] | 汤开然, 冯成领, 韩邦旻. 基于单细胞测序与转录组测序构建M2巨噬细胞基因相关的前列腺癌预后模型[J]. 上海交通大学学报(医学版), 2025, 45(5): 549-561. |
| [7] | 许天芸, 沈奕茗, 姜萌. 射血分数改善型心力衰竭的临床管理: 治疗与维持[J]. 上海交通大学学报(医学版), 2025, 45(4): 493-499. |
| [8] | 刘田恬, 赵奕琳, 宁菁菁, 张育才, 王春霞. 儿童脓毒症预后相关长链非编码RNA筛选及竞争性内源RNA网络的构建[J]. 上海交通大学学报(医学版), 2025, 45(3): 282-291. |
| [9] | 陈佳莹, 褚以忞, 彭海霞. 结直肠癌无进展生存时间预测模型及影响因素研究[J]. 上海交通大学学报(医学版), 2025, 45(3): 324-334. |
| [10] | 梁乐斌, 陈慧芳, 赖淑静, 顾靓, 苏冰. 基于空间ATAC-seq技术的Apcmin/+小鼠结肠肿瘤表观特征分析[J]. 上海交通大学学报(医学版), 2025, 45(10): 1261-1270. |
| [11] | 钱立恒, 温凯玲, 廖颖娜, 李书鑫, 聂惠贞. 分选链接蛋白1抑制结直肠癌细胞增殖和迁移的作用和机制研究[J]. 上海交通大学学报(医学版), 2024, 44(9): 1124-1135. |
| [12] | 王博恩, 陈思远, 施晴, 张慕晨, 易红梅, 董磊, 王黎, 程澍, 许彭鹏, 赵维莅. 肾脏累及的弥漫性大B细胞淋巴瘤患者临床病理特征[J]. 上海交通大学学报(医学版), 2024, 44(9): 1162-1168. |
| [13] | 冯昫皎, 刘健悦, 戚炀炀, 孙晶, 沈蕾. 结直肠癌中自然杀伤细胞表型及功能初探[J]. 上海交通大学学报(医学版), 2024, 44(6): 713-722. |
| [14] | 俞洋, 孟丹, 仇奕文, 袁见, 朱莹杰. 两样本孟德尔随机化法分析1型糖尿病对结直肠癌的影响[J]. 上海交通大学学报(医学版), 2024, 44(6): 755-761. |
| [15] | 宋晨璐, 向军, 杨惠忠. 血清肝素结合蛋白对重度烧伤患者预后及脓毒症发生的早期预警价值[J]. 上海交通大学学报(医学版), 2024, 44(4): 474-481. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||
