
上海交通大学学报(医学版) ›› 2023, Vol. 43 ›› Issue (9): 1153-1161.doi: 10.3969/j.issn.1674-8115.2023.09.009
卢启帆( ), 刘启明, 周红梅, 柴烨子, 姜萌(
), 刘启明, 周红梅, 柴烨子, 姜萌( ), 卜军(
), 卜军( )
)
收稿日期:2023-03-27
接受日期:2023-05-24
出版日期:2023-09-28
发布日期:2023-09-28
通讯作者:
卜 军,电子信箱:pujun310@hotmail.com。作者简介:卢启帆(1997—),女,博士生;电子信箱:czzx_2012_505@126.com。
基金资助:
LU Qifan( ), LIU Qiming, ZHOU Hongmei, CHAI Yezi, JIANG Meng(
), LIU Qiming, ZHOU Hongmei, CHAI Yezi, JIANG Meng( ), PU Jun(
), PU Jun( )
)
Received:2023-03-27
Accepted:2023-05-24
Online:2023-09-28
Published:2023-09-28
Contact:
PU Jun, E-mail: pujun310@hotmail.com.Supported by:摘要:
目的·探讨慢性心力衰竭(心衰)患者躯体化症状、焦虑、抑郁与临床结局的关系。方法·纳入2018年1月—2021年12月上海交通大学医学院附属仁济医院心内科门诊就诊的心衰患者。收集患者人口学资料及临床特征,采用躯体化症状评估量表(Self-reported Somatic Symptom Scale of China,SSS-CN)、9项患者健康问卷(The Patient Health Questionnaire-9,PHQ-9)及7项广泛性焦虑障碍量表(Generalized Anxiety Disorder-7,GAD-7)对患者进行评估。在初次就诊后的第12个月进行电话随访,收集患者终点事件具体信息(包括是否死亡、是否再住院、死亡原因及再住院原因)。采用生存曲线及Cox回归分析评价患者的临床预后。结果·共纳入患者195例。慢性心衰患者SSS-CN得分在不同性别、心率分组、美国纽约心脏病学会(New York Heart Association,NYHA)心功能分级,以及是否焦虑、抑郁人群间的差异具有统计学意义(均P<0.05)。生存曲线分析显示,中-重度躯体化症状组患者的总体生存率低于正常-轻度组(Log rank P=0.020)。Cox回归分析显示,与正常-轻度组相比,中-重度躯体化症状组患者的全因死亡风险更高[风险比(HR)=2.797,95%CI 1.135~6.890];存在抑郁症状的心衰患者全因死亡风险更高(HR=2.883,95%CI 1.150~6.984);与正常-轻度组相比,中-重度躯体化症状组患者心血管死亡风险更高(HR=2.784,95%CI 1.073~7.226);存在抑郁症状的心衰患者心血管死亡的风险更高(HR=2.823,95%CI 1.087~7.330)。心衰患者有无焦虑、抑郁,有无躯体化症状及其不同严重程度在全因住院和因心衰住院中的差异无统计学意义。结论·中-重度的躯体化症状及抑郁状态是慢性心衰患者全因死亡及心血管死亡的危险因素。
中图分类号:
卢启帆, 刘启明, 周红梅, 柴烨子, 姜萌, 卜军. 慢性心力衰竭患者躯体化症状、焦虑、抑郁对临床结局的影响[J]. 上海交通大学学报(医学版), 2023, 43(9): 1153-1161.
LU Qifan, LIU Qiming, ZHOU Hongmei, CHAI Yezi, JIANG Meng, PU Jun. Effect of somatic symptoms, anxiety and depression on clinical prognosis in patients with chronic heart failure[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2023, 43(9): 1153-1161.
| Item | Participant/n(%) | SSS-CN | |
|---|---|---|---|
| Score/point | P value | ||
| Gender | 0.017 | ||
| Male | 132 (67.69) | 32.0 (27.0, 39.0) | |
| Female | 63 (32.31) | 34.0 (30.0, 42.0) | |
| Age | 0.141 | ||
| <60 years | 88 (45.13) | 31.0 (26.0, 39.0) | |
| ≥60 years | 107 (54.87) | 34.0 (28.8, 41.1) | |
| Marriage status | 0.992 | ||
| Married | 189 (96.92) | 32.5 (28.5, 46.0) | |
| Not married | 4 (2.05) | 33.0 (28.5, 40.0) | |
| Divorced | 2 (1.03) | 36.5 (33.0, 37.5) | |
| Job | 0.401 | ||
| Retired or unemployment | 121 (62.05) | 34.0 (29.0, 41.0) | |
| In service | 74 (37.95) | 32.5 (27.5, 38.5) | |
| Education | 0.881 | ||
| Middle school and below | 68 (34.87) | 33.5 (28.4, 40.1) | |
| High school | 63 (32.31) | 33.5 (29.0, 40.2) | |
| College | 59 (30.26) | 29.5 (25.6, 36.2) | |
| Master and above | 5 (2.56) | 33.0 (28.0, 40.0) | |
| PHQ-9 | 0.000 | ||
| >4 points | 51 (26.15) | 41.0 (36.0, 49.0) | |
| ≤4 points | 144 (83.75) | 30.0 (26.0, 36.0) | |
| GAD-7 | 0.000 | ||
| >4 points | 34 (17.43) | 41.0 (37.9, 41.5) | |
| ≤4 points | 161 (82.57) | 31.0 (27.0, 37.0) | |
| NYHA classification | 0.013 | ||
| Ⅰ-Ⅱ | 144 (73.85) | 30.0 (26.0, 37.0) | |
| Ⅲ-Ⅳ | 51 (26.15) | 37.0 (30.5, 45.5) | |
| Heart rate | 0.016 | ||
| <68 bpm | 51 (26.15) | 36.0 (30.0, 45.3) | |
| ≥68 and <75 bpm | 42 (21.54) | 28.0 (26.0, 32.8) | |
| ≥75 and <81 bpm | 53 (27.18) | 31.0 (27.0, 37.0) | |
| ≥81 bpm | 49 (25.13) | 33.0 (29.0, 42.0) | |
| Blood pressure | 0.710 | ||
| SBP>140 mmHg or DBP>90 mmHg | 44 (22.56) | 32.5 (28.0, 40.0) | |
| SBP≤140 mmHg and DBP≤90 mmHg | 151 (77.44) | 33.0 (28.2, 40.8) | |
| BMI | 0.902 | ||
| ≥25 kg·m-2 | 57 (29.23) | 31.5 (27.2, 38.8) | |
| <25 kg·m-2 | 138 (70.77) | 32.0 (27.0, 41.0) | |
| LVEF | 0.674 | ||
| ≤40% | 84 (43.08) | 31.0 (28.0, 38.0) | |
| 40%<LVEF<50% | 52 (26.67) | 33.0 (29.0, 41.8) | |
| ≥50% | 59 (30.25) | 34.0 (26.0, 40.0) | |
表1 心衰患者人口学、临床基线特征及SSS-CN得分情况(n=195)
Tab 1 Sociodemographic and clinical characteristics and SSS-CN scores of the CHF population (n=195)
| Item | Participant/n(%) | SSS-CN | |
|---|---|---|---|
| Score/point | P value | ||
| Gender | 0.017 | ||
| Male | 132 (67.69) | 32.0 (27.0, 39.0) | |
| Female | 63 (32.31) | 34.0 (30.0, 42.0) | |
| Age | 0.141 | ||
| <60 years | 88 (45.13) | 31.0 (26.0, 39.0) | |
| ≥60 years | 107 (54.87) | 34.0 (28.8, 41.1) | |
| Marriage status | 0.992 | ||
| Married | 189 (96.92) | 32.5 (28.5, 46.0) | |
| Not married | 4 (2.05) | 33.0 (28.5, 40.0) | |
| Divorced | 2 (1.03) | 36.5 (33.0, 37.5) | |
| Job | 0.401 | ||
| Retired or unemployment | 121 (62.05) | 34.0 (29.0, 41.0) | |
| In service | 74 (37.95) | 32.5 (27.5, 38.5) | |
| Education | 0.881 | ||
| Middle school and below | 68 (34.87) | 33.5 (28.4, 40.1) | |
| High school | 63 (32.31) | 33.5 (29.0, 40.2) | |
| College | 59 (30.26) | 29.5 (25.6, 36.2) | |
| Master and above | 5 (2.56) | 33.0 (28.0, 40.0) | |
| PHQ-9 | 0.000 | ||
| >4 points | 51 (26.15) | 41.0 (36.0, 49.0) | |
| ≤4 points | 144 (83.75) | 30.0 (26.0, 36.0) | |
| GAD-7 | 0.000 | ||
| >4 points | 34 (17.43) | 41.0 (37.9, 41.5) | |
| ≤4 points | 161 (82.57) | 31.0 (27.0, 37.0) | |
| NYHA classification | 0.013 | ||
| Ⅰ-Ⅱ | 144 (73.85) | 30.0 (26.0, 37.0) | |
| Ⅲ-Ⅳ | 51 (26.15) | 37.0 (30.5, 45.5) | |
| Heart rate | 0.016 | ||
| <68 bpm | 51 (26.15) | 36.0 (30.0, 45.3) | |
| ≥68 and <75 bpm | 42 (21.54) | 28.0 (26.0, 32.8) | |
| ≥75 and <81 bpm | 53 (27.18) | 31.0 (27.0, 37.0) | |
| ≥81 bpm | 49 (25.13) | 33.0 (29.0, 42.0) | |
| Blood pressure | 0.710 | ||
| SBP>140 mmHg or DBP>90 mmHg | 44 (22.56) | 32.5 (28.0, 40.0) | |
| SBP≤140 mmHg and DBP≤90 mmHg | 151 (77.44) | 33.0 (28.2, 40.8) | |
| BMI | 0.902 | ||
| ≥25 kg·m-2 | 57 (29.23) | 31.5 (27.2, 38.8) | |
| <25 kg·m-2 | 138 (70.77) | 32.0 (27.0, 41.0) | |
| LVEF | 0.674 | ||
| ≤40% | 84 (43.08) | 31.0 (28.0, 38.0) | |
| 40%<LVEF<50% | 52 (26.67) | 33.0 (29.0, 41.8) | |
| ≥50% | 59 (30.25) | 34.0 (26.0, 40.0) | |
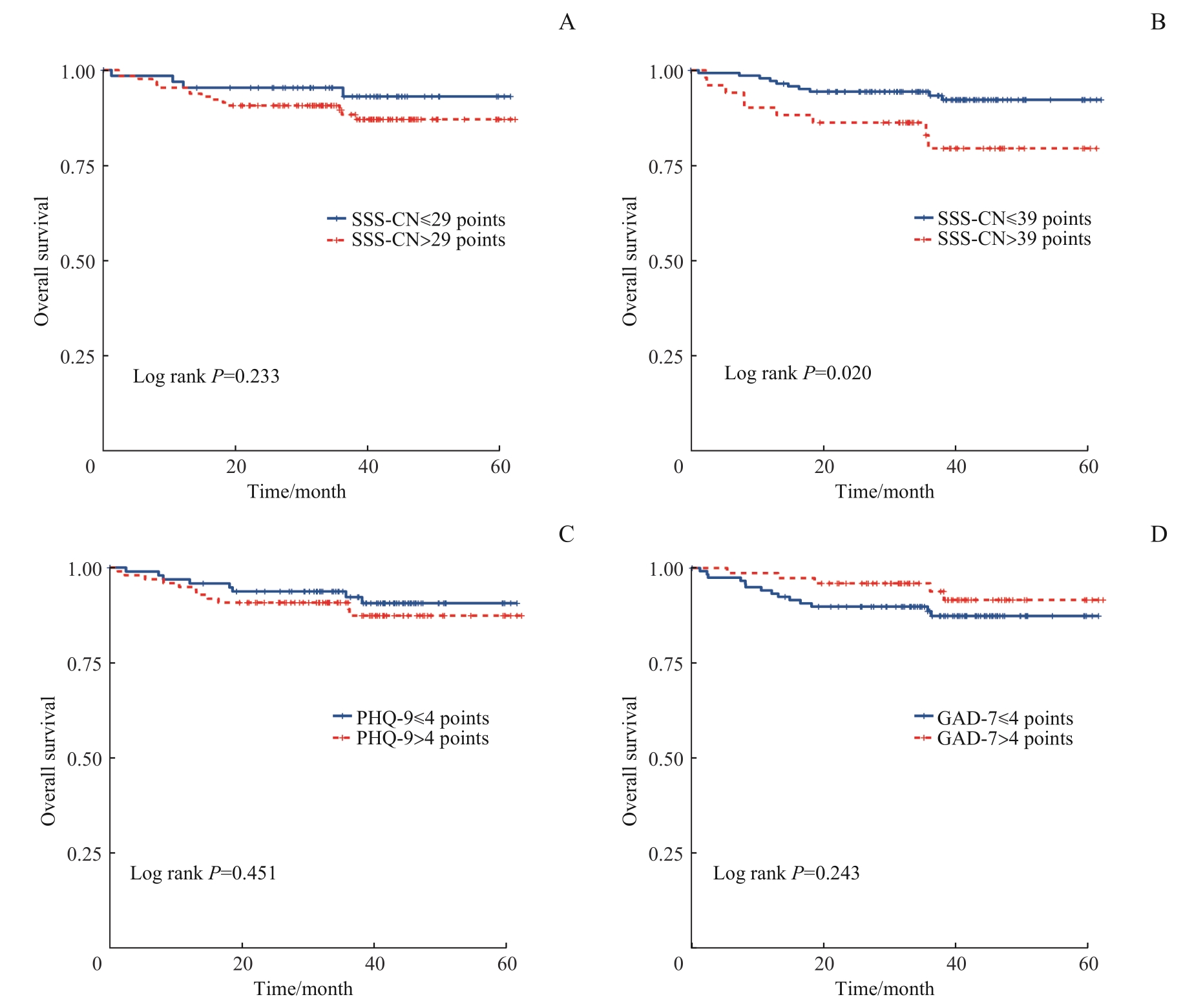
图1 患者基线时躯体化症状、焦虑、抑郁对总体生存率的影响Note: A. Survival curves for SSS-CN>29 points and ≤29 points. B. Survival curves for SSS-CN>39 points and ≤39 points. C. Survival curves for PHQ-9>4 points and ≤4 points. D. Survival curves for GAD-7>4 points and ≤4 points.
Fig 1 Effects of somatization symptoms, anxiety and depression at baseline on the patients′ overall survival rates
| Item | All-cause hospitalization | Heart failure induced hospitalization | |||||
|---|---|---|---|---|---|---|---|
| None (n=174) | Yes (n=21) | P value | None (n=187) | Yes (n=8) | P value | ||
| Gender/n(%) | 0.915 | 0.139 | |||||
| Female | 56 (32.18) | 7 (33.33) | 58 (31.02) | 5 (62.50) | |||
| Male | 118 (67.82) | 14 (66.67) | 129 (68.98) | 3 (37.50) | |||
| Age/year | 57.0±14.4 | 65.8±14.6 | 0.000 | 57.5±14.4 | 68.1±16.5 | 0.043 | |
| SSS-CN/n(%) | 0.589 | 0.874 | |||||
| ≤29 points | 60 (34.48) | 6 (28.57) | 64 (34.22) | 2 (25.00) | |||
| >29 points | 114 (65.52) | 15 (71.43) | 123 (65.78) | 6 (75.00) | |||
| SSS-CN/n(%) | 0.428 | 0.738 | |||||
| ≤39 points | 130 (74.71) | 14 (66.67) | 139 (74.33) | 5 (62.50) | |||
| >39 points | 44 (25.29) | 7 (33.33) | 48 (25.67) | 3 (37.50) | |||
| PHQ-9/n(%) | 0.240 | 0.247 | |||||
| >4 points | 131 (75.29) | 13 (61.90) | 140 (74.87) | 4 (50.00) | |||
| ≤4 points | 43 (24.71) | 8 (38.10) | 47 (25.13) | 4 (50.00) | |||
| GAD-7/n(%) | 0.965 | 0.957 | |||||
| >4 points | 139 (79.89) | 18 (85.71) | 150 (80.21) | 7 (87.50) | |||
| ≤4 points | 35 (20.11) | 3 (14.29) | 37 (19.79) | 1 (12.50) | |||
| NYHA classification/n(%) | 0.037 | 0.039 | |||||
| Ⅰ-Ⅱ | 133 (76.4) | 11 (52.63) | 141 (75.41) | 3 (37.50) | |||
| Ⅲ-Ⅳ | 41 (23.5) | 10 (47.37) | 46 (24.59) | 5 (62.50) | |||
| Heart rate/bpm | 76.1±12.0 | 76.4±12.4 | 0.562 | 76.4±12.1 | 72.4±10.2 | 0.365 | |
| SBP/mmHg | 127.06±19.11 | 127.39±19.81 | 0.606 | 127.23±19.47 | 124.25±12.19 | 0.670 | |
| DBP/mmHg | 79.38±13.23 | 80.18±13.17 | 0.073 | 79.89±13.13 | 71.00±12.80 | 0.065 | |
| Height/cm | 168.62±8.09 | 168.19±8.42 | 0.843 | 168.63±7.97 | 167.57±10.61 | 0.740 | |
| Weight/kg | 72.38±16.61 | 66.31±11.35 | 0.163 | 72.17±16.21 | 61.71±9.88 | 0.096 | |
| BMI/(kg·m-2) | 25.36±4.99 | 23.31±2.63 | 0.112 | 25.28±4.83 | 21.86±1.80 | 0.066 | |
| TNI/(ng·mL-1) | 0.03 (0.01, 0.16) | 0.01 (0.01, 0.03) | 0.174 | 0.04 (0, 0.07) | 0.04 (0, 0.07) | 0.750 | |
| BNP/(pg·mL-1) | 214.0 (100.0, 573.5) | 225.5 (49.0, 510.7) | 0.736 | 205.0 (49.0, 491.0) | 508.0 (241.0, 980.0) | 0.467 | |
| LVEF/n(%) | 0.531 | 0.195 | |||||
| ≤40% | 71 (40.80) | 13 (61.90) | 79 (42.25) | 5 (62.50) | |||
| 40%<LVEF<50% | 47 (27.01) | 5 (23.81) | 50 (26.73) | 2 (25.00) | |||
| ≥50% | 56 (32.19) | 3 (14.29) | 58 (31.02) | 1 (12.50) | |||
表4 心衰患者1年内全因住院和因心衰再住院的单因素分析
Tab 4 Univariate analysis of all-cause hospitalization and heart failure-induced hospitalization within 1 year in the CHF patients
| Item | All-cause hospitalization | Heart failure induced hospitalization | |||||
|---|---|---|---|---|---|---|---|
| None (n=174) | Yes (n=21) | P value | None (n=187) | Yes (n=8) | P value | ||
| Gender/n(%) | 0.915 | 0.139 | |||||
| Female | 56 (32.18) | 7 (33.33) | 58 (31.02) | 5 (62.50) | |||
| Male | 118 (67.82) | 14 (66.67) | 129 (68.98) | 3 (37.50) | |||
| Age/year | 57.0±14.4 | 65.8±14.6 | 0.000 | 57.5±14.4 | 68.1±16.5 | 0.043 | |
| SSS-CN/n(%) | 0.589 | 0.874 | |||||
| ≤29 points | 60 (34.48) | 6 (28.57) | 64 (34.22) | 2 (25.00) | |||
| >29 points | 114 (65.52) | 15 (71.43) | 123 (65.78) | 6 (75.00) | |||
| SSS-CN/n(%) | 0.428 | 0.738 | |||||
| ≤39 points | 130 (74.71) | 14 (66.67) | 139 (74.33) | 5 (62.50) | |||
| >39 points | 44 (25.29) | 7 (33.33) | 48 (25.67) | 3 (37.50) | |||
| PHQ-9/n(%) | 0.240 | 0.247 | |||||
| >4 points | 131 (75.29) | 13 (61.90) | 140 (74.87) | 4 (50.00) | |||
| ≤4 points | 43 (24.71) | 8 (38.10) | 47 (25.13) | 4 (50.00) | |||
| GAD-7/n(%) | 0.965 | 0.957 | |||||
| >4 points | 139 (79.89) | 18 (85.71) | 150 (80.21) | 7 (87.50) | |||
| ≤4 points | 35 (20.11) | 3 (14.29) | 37 (19.79) | 1 (12.50) | |||
| NYHA classification/n(%) | 0.037 | 0.039 | |||||
| Ⅰ-Ⅱ | 133 (76.4) | 11 (52.63) | 141 (75.41) | 3 (37.50) | |||
| Ⅲ-Ⅳ | 41 (23.5) | 10 (47.37) | 46 (24.59) | 5 (62.50) | |||
| Heart rate/bpm | 76.1±12.0 | 76.4±12.4 | 0.562 | 76.4±12.1 | 72.4±10.2 | 0.365 | |
| SBP/mmHg | 127.06±19.11 | 127.39±19.81 | 0.606 | 127.23±19.47 | 124.25±12.19 | 0.670 | |
| DBP/mmHg | 79.38±13.23 | 80.18±13.17 | 0.073 | 79.89±13.13 | 71.00±12.80 | 0.065 | |
| Height/cm | 168.62±8.09 | 168.19±8.42 | 0.843 | 168.63±7.97 | 167.57±10.61 | 0.740 | |
| Weight/kg | 72.38±16.61 | 66.31±11.35 | 0.163 | 72.17±16.21 | 61.71±9.88 | 0.096 | |
| BMI/(kg·m-2) | 25.36±4.99 | 23.31±2.63 | 0.112 | 25.28±4.83 | 21.86±1.80 | 0.066 | |
| TNI/(ng·mL-1) | 0.03 (0.01, 0.16) | 0.01 (0.01, 0.03) | 0.174 | 0.04 (0, 0.07) | 0.04 (0, 0.07) | 0.750 | |
| BNP/(pg·mL-1) | 214.0 (100.0, 573.5) | 225.5 (49.0, 510.7) | 0.736 | 205.0 (49.0, 491.0) | 508.0 (241.0, 980.0) | 0.467 | |
| LVEF/n(%) | 0.531 | 0.195 | |||||
| ≤40% | 71 (40.80) | 13 (61.90) | 79 (42.25) | 5 (62.50) | |||
| 40%<LVEF<50% | 47 (27.01) | 5 (23.81) | 50 (26.73) | 2 (25.00) | |||
| ≥50% | 56 (32.19) | 3 (14.29) | 58 (31.02) | 1 (12.50) | |||
| 1 | 中华医学会心血管病学分会心力衰竭学组, 中国医师协会心力衰竭专业委员会, 中华心血管病杂志编辑委员会. 中国心力衰竭诊断和治疗指南2018[J]. 中华心血管病杂志, 2018, 46(10): 760-789. |
| Heart Failure Group of Chinese Society of Cardiology of Chinese Medical Association, Chinese Heart Failure Association of Chinese Medical Doctor Association, Editorial Board of Chinese Journal of Cardiology. Chinese guidelines for the diagnosis and treatment of heart failure 2018[J]. Chinese Journal of Cardiology, 2018, 46(10): 760-789. | |
| 2 | PONIKOWSKI P, VOORS A A, ANKER S D, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Eur Heart J, 2016, 37(27): 2129-2200. |
| 3 | ZHANG Y, LV X Z, JIANG W, et al. Effectiveness of a telephone-delivered psycho-behavioural intervention on depression in elderly with chronic heart failure: rationale and design of a randomized controlled trial[J]. BMC Psychiatry, 2019, 19(1): 161. |
| 4 | DIMSDALE J E, CREED F, ESCOBAR J, et al. Somatic symptom disorder: an important change in DSM[J]. J Psychosom Res, 2013, 75(3): 223-228. |
| 5 | BATTLE D E. Diagnostic and statistical manual of mental disorders (DSM)[J]. Codas, 2013, 25(2): 191-192. |
| 6 | LIANG D, MAYS V M, HWANG W C. Integrated mental health services in China: challenges and planning for the future[J]. Health Policy Plan, 2018, 33(1): 107-122. |
| 7 | GUIDI J, RAFANELLI C, RONCUZZI R, et al. Assessing psychological factors affecting medical conditions: comparison between different proposals[J]. Gen Hosp Psychiatry, 2013, 35(2): 141-146. |
| 8 | CELANO C M, VILLEGAS A C, ALBANESE A M, et al. Depression and anxiety in heart failure: a review[J]. Harv Rev Psychiatry, 2018, 26(4): 175-184. |
| 9 | HERR J K, SALYER J, FLATTERY M, et al. Heart failure symptom clusters and functional status: a cross-sectional study[J]. J Adv Nurs, 2015, 71(6): 1274-1287. |
| 10 | SALYER J, FLATTERY M, LYON D E. Heart failure symptom clusters and quality of life[J]. Heart Lung, 2019, 48(5): 366-372. |
| 11 | CAO L H, LUO G, CAO L F, et al. Somatization disorder mediates the association of depression and anxiety with functional impairment in patients with heart failure[J]. Psychol Health Med, 2021, 26(7): 911-916. |
| 12 | RUTLEDGE T, REIS V A, LINKE S E, et al. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes[J]. J Am Coll Cardiol, 2006, 48(8): 1527-1537. |
| 13 | SCHIFFER A A, PELLE A J, SMITH O R, et al. Somatic versus cognitive symptoms of depression as predictors of all-cause mortality and health status in chronic heart failure[J]. J Clin Psychiatry, 2009, 70(12): 1667-1673. |
| 14 | 庄琦, 毛家亮, 李春波, 等. 躯体化症状自评量表的初步编制及信度和效度研究[J]. 中华行为医学与脑科学杂志, 2010, 19(9): 847-849. |
| ZHUANG Q, MAO J L, LI C B, et al. Developing of Somatic Self-rating Scale and its reliability and validity[J]. Chinese Journal of Behavioral Medical and Brain Science, 2010, 19(9): 847-849. | |
| 15 | KROENKE K, SPITZER R L, WILLIAMS J B. The PHQ-9: validity of a brief depression severity measure[J]. J Gen Intern Med, 2001, 16(9): 606-613. |
| 16 | SPITZER R L, KROENKE K, WILLIAMS J B W, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7[J]. Arch Intern Med, 2006, 166(10): 1092-1097. |
| 17 | 中华医学会神经病学分会神经心理学与行为神经病学组. 综合医院焦虑、抑郁与躯体化症状诊断治疗的专家共识[J]. 中华神经科杂志, 2016, 49(12): 908-917. |
| Neuropsychology and Behavioral Neurology Group of Chinese Society of Neurology of Chinese Medical Association. Expert consensus on the diagnosis and treatment of anxiety, depression and somatic symptoms in general hospitals[J]. Chinese Journal of Neurology, 2016, 49(12): 908-917. | |
| 18 | HEIDENREICH P A, BOZKURT B, AGUILAR D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines[J]. Circulation, 2022, 145(18): e876-e894. |
| 19 | PARKER G, BROTCHIE H. Gender differences in depression[J]. Int Rev Psychiatry, 2010, 22(5): 429-436. |
| 20 | SCIOMER S, MOSCUCCI F, SALVIONI E, et al. Role of gender, age and BMI in prognosis of heart failure[J]. Eur J Prev Cardiol, 2020, 27(2_suppl): 46-51. |
| 21 | FERRARI R. Ivabradine: heart rate and left ventricular function[J]. Cardiology, 2014, 128(2): 226-230. |
| 22 | SWEDBERG K, KOMAJDA M, BÖHM M, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study[J]. Lancet, 2010, 376(9744): 875-885. |
| 23 | LEE C S, GELOW J M, DENFELD Q E, et al. Physical and psychological symptom profiling and event-free survival in adults with moderate to advanced heart failure[J]. J Cardiovasc Nurs, 2014, 29(4): 315-323. |
| 24 | PATEL H, SHAFAZAND M, SCHAUFELBERGER M, et al. Reasons for seeking acute care in chronic heart failure[J]. Eur J Heart Fail, 2007, 9(6/7): 702-708. |
| 25 | DASKALOPOULOU M, GEORGE J, WALTERS K, et al. Depression as a risk factor for the initial presentation of twelve cardiac, cerebrovascular, and peripheral arterial diseases: data linkage study of 1.9 million women and men[J]. PLoS One, 2016, 11(4): e0153838. |
| 26 | FRIEDMANN E, THOMAS S A, LIU F, et al. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality[J]. Am Heart J, 2006, 152(5): 940.e1-940.e8. |
| 27 | CELANO C M, MILLSTEIN R A, BEDOYA C A, et al. Association between anxiety and mortality in patients with coronary artery disease: a meta-analysis[J]. Am Heart J, 2015, 170(6): 1105-1115. |
| 28 | CELANO C M, MASTROMAURO C A, LENIHAN E C, et al. Association of baseline anxiety with depression persistence at 6 months in patients with acute cardiac illness[J]. Psychosom Med, 2012, 74(1): 93-99. |
| [1] | 周亦凝, 叶之韵, 陈慧文, 谢欣宜, 周薇, 宋忠臣. Th17细胞特异性敲除Stat3对牙周炎小鼠焦虑抑郁样行为的影响[J]. 上海交通大学学报(医学版), 2025, 45(7): 838-845. |
| [2] | 王思睿, 孔盖, 李惠, 钱禛颖, 崔慧茹, 唐莺莹. 经颅磁刺激治疗对抑郁症患者杏仁核及海马亚区体积的影响[J]. 上海交通大学学报(医学版), 2025, 45(4): 434-442. |
| [3] | 孙一丹, 杨鑫. 焦虑增强颞下颌关节疼痛的脑功能磁共振成像研究[J]. 上海交通大学学报(医学版), 2025, 45(3): 342-348. |
| [4] | 耿梦璐, 李春波. 抑郁障碍患者记忆提取抑制受损的研究进展[J]. 上海交通大学学报(医学版), 2025, 45(10): 1378-1382. |
| [5] | 陈深册, 陈依明, 王凡, 张梦珂, 杨惟杰, 吕洞宾, 洪武. 饮食干预治疗抑郁相关症状的研究进展[J]. 上海交通大学学报(医学版), 2024, 44(8): 1050-1055. |
| [6] | 苏珊珊, 蒋文晖, 王书婷, 徐觅真, 任雪晴, 仇剑崟. 焦虑障碍患者的焦虑水平、述情障碍程度对其生活质量的影响[J]. 上海交通大学学报(医学版), 2024, 44(5): 584-590. |
| [7] | 孙晨寅, 吴百川, 张慧凤, 方贻儒, 彭代辉. 体动记录仪评估抑郁症昼夜节律:一项系统综述和meta分析[J]. 上海交通大学学报(医学版), 2024, 44(5): 606-616. |
| [8] | 廖冰冰, 王振. 情感性触觉干预早期应激相关的焦虑障碍的研究进展[J]. 上海交通大学学报(医学版), 2024, 44(5): 647-652. |
| [9] | 谷涓华, 焦扬, 鲁琳, 王琳琳. 胶质细胞内SNARE复合体功能及其与抑郁障碍发生的关系[J]. 上海交通大学学报(医学版), 2024, 44(5): 653-657. |
| [10] | 郑梦奕, 毛家亮, 邹治国, 张瑞雷, 张厚, 李世光. 全身免疫炎症指数及躯体化症状评分对首发心梗PCI术后发生院内主要不良心血管事件的预测价值[J]. 上海交通大学学报(医学版), 2024, 44(3): 334-341. |
| [11] | 杨瑞君, 吕书红, 刘志业, 张新, 刘志浩. 中国5省初中生视屏时间和饮食行为与抑郁症状的关联[J]. 上海交通大学学报(医学版), 2024, 44(3): 358-364. |
| [12] | 王晓玉, 彭银辉, 马文琳, 姚博爽, 李一凡, 赵莉, 杨春霞. 新冠疫情大流行期间儿童及青少年新发焦虑症状的纵向研究[J]. 上海交通大学学报(医学版), 2023, 43(8): 963-970. |
| [13] | 马文琳, 林元杰, 金婷婷, 石薇, 蒋莉华, 赵莉. 初中生自我中心主义与非自杀性自伤的关系研究[J]. 上海交通大学学报(医学版), 2023, 43(8): 971-976. |
| [14] | 张硕渊, 李春波. 运动治疗抑郁障碍的研究进展[J]. 上海交通大学学报(医学版), 2023, 43(7): 916-922. |
| [15] | 马翠, 叶钰娟, 严兴科. 杏仁核介导的痛情绪神经环路研究进展[J]. 上海交通大学学报(医学版), 2023, 43(10): 1304-1310. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||