
上海交通大学学报(医学版) ›› 2022, Vol. 42 ›› Issue (8): 1070-1080.doi: 10.3969/j.issn.1674-8115.2022.08.012
邱佳辉1,2( ), 蔡谦谦2, 杨彦2, 程非池2, 裘正军1,2(
), 蔡谦谦2, 杨彦2, 程非池2, 裘正军1,2( ), 黄陈1,2(
), 黄陈1,2( )
)
收稿日期:2022-03-11
接受日期:2022-07-21
出版日期:2022-08-28
发布日期:2022-10-08
通讯作者:
黄 陈,电子信箱:richard-hc@hotmail.com。作者简介:邱佳辉(1993—),男,硕士生;电子信箱:1326880749@qq.com。
基金资助:
QIU Jiahui1,2( ), CAI Qianqian2, YANG Yan2, CHENG Feichi2, QIU Zhengjun1,2(
), CAI Qianqian2, YANG Yan2, CHENG Feichi2, QIU Zhengjun1,2( ), HUANG Chen1,2(
), HUANG Chen1,2( )
)
Received:2022-03-11
Accepted:2022-07-21
Online:2022-08-28
Published:2022-10-08
Contact:
HUANG Chen, E-mail: richard-hc@hotmail.com.#Corresponding authors.Supported by:摘要:
目的·探讨肿瘤间质比(tumor-stroma ratio,TSR)、神经浸润(perineural invasion,PNI)、脉管浸润(lymphovascular invasion,LVI)对结直肠癌(colorectal cancer,CRC)患者预后的预测价值。方法·回顾性分析2014年1月—2018年12月在上海交通大学医学院附属第一人民医院确诊为CRC的948例患者资料,按病理高危因素TSR、PNI、LVI分为高风险组(n=81)和低风险组(n=867),经SPSS软件进行1∶1病例匹配后得到高风险组67例。低风险组67例,比较高风险组患者和低风险组患者的总生存时间(overall survival,OS),并使用该课题组106例结直肠癌组织芯片(tissue microarray,TMA)数据进行验证。比较高风险组和低风险组的临床特点,采用Kaplan-Meier法进行生存分析,COX回归模型分析影响预后的因素。结果·与低风险组患者中位OS(31.1个月)相比,高风险组患者中位OS(27.7个月)缩短,预后更差(P=0.000)。经过配对后发现具有神经脉管浸润阳性联合高肿瘤间质比特征对预测CRC预后的价值更大,并且在TMA数据中也得到了验证。结论·神经脉管浸润阳性联合高TSR的CRC是一类预后不良的CRC,可以弥补肿瘤-淋巴结-转移(tumor-node-metastasis,TNM)病理分期系统对预后预测的缺陷,可以用于预估CRC患者术后病情发展及指导治疗。
中图分类号:
邱佳辉, 蔡谦谦, 杨彦, 程非池, 裘正军, 黄陈. 神经脉管浸润联合肿瘤间质比对结直肠癌预后的预测价值[J]. 上海交通大学学报(医学版), 2022, 42(8): 1070-1080.
QIU Jiahui, CAI Qianqian, YANG Yan, CHENG Feichi, QIU Zhengjun, HUANG Chen. Value of combined perineural lymphovascular invasion and tumor-stroma ratio in guiding the prognosis of colorecatal cancer[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2022, 42(8): 1070-1080.
| Indicator | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| HR | 95%CI | P value | HR | 95%CI | P value | ||
| Grade | |||||||
| Well | ‒ | 1 | ‒ | ||||
| Moderate | 2.333 | 0.945‒5.759 | 0.660 | ||||
| Poor | 3.824 | 1.451‒10.079 | 0.007* | ||||
| T Stage | |||||||
| T1 | ‒ | 1 | ‒ | ||||
| T2 | 1.897 | 0.240‒14.981 | 0.544 | ||||
| T3 | 2.201 | 0.291‒16.676 | 0.445 | ||||
| T4 | 6.070 | 0.845‒43.588 | 0.073 | ||||
| N Stage | |||||||
| N0 | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| N1 | 2.364 | 1.477‒3.784 | 0.000** | 1.742 | 1.065‒2.850 | 0.027* | |
| N2 | 5.832 | 3.725‒9.130 | 0.000** | 5.022 | 3.103‒8.128 | 0.000** | |
| Tumor location | |||||||
| Right | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Left | 0.461 | 0.281‒0.757 | 0.002* | 0.438 | 0.265‒0.723 | 0.001* | |
| Rectal | 0.472 | 0.307‒0.725 | 0.001* | 0.472 | 0.304‒0.735 | 0.001* | |
| Gender | |||||||
| Male | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Female | 0.602 | 0.402‒0.902 | 0.014* | 0.569 | 0.377‒0.858 | 0.007* | |
| Tumor size | |||||||
| <5 cm | ‒ | 1 | ‒ | ||||
| ≥5 cm | 1.294 | 0.887‒1.888 | 0.182 | ||||
| Age | |||||||
| ≤67 years | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| >67 years | 3.315 | 2.188‒5.022 | 0.000** | 3.426 | 2.245‒5.227 | 0.000** | |
| Risk factor | |||||||
| 0 | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| 1 | 2.122 | 1.156‒3.893 | 0.015* | 2.037 | 1.105‒3.755 | 0.023* | |
| 2 | 3.742 | 2.013‒6.957 | 0.000** | 2.604 | 1.372‒4.942 | 0.003* | |
| 3 | 6.074 | 3.065‒12.037 | 0.000** | 3.564 | 1.732‒7.336 | 0.001* | |
表1 CRC总体生存率影响因素的单因素和多因素COX分析
Tab 1 Univariate and multivariate COX analysis of influencing factors for overall survival of CRC
| Indicator | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| HR | 95%CI | P value | HR | 95%CI | P value | ||
| Grade | |||||||
| Well | ‒ | 1 | ‒ | ||||
| Moderate | 2.333 | 0.945‒5.759 | 0.660 | ||||
| Poor | 3.824 | 1.451‒10.079 | 0.007* | ||||
| T Stage | |||||||
| T1 | ‒ | 1 | ‒ | ||||
| T2 | 1.897 | 0.240‒14.981 | 0.544 | ||||
| T3 | 2.201 | 0.291‒16.676 | 0.445 | ||||
| T4 | 6.070 | 0.845‒43.588 | 0.073 | ||||
| N Stage | |||||||
| N0 | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| N1 | 2.364 | 1.477‒3.784 | 0.000** | 1.742 | 1.065‒2.850 | 0.027* | |
| N2 | 5.832 | 3.725‒9.130 | 0.000** | 5.022 | 3.103‒8.128 | 0.000** | |
| Tumor location | |||||||
| Right | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Left | 0.461 | 0.281‒0.757 | 0.002* | 0.438 | 0.265‒0.723 | 0.001* | |
| Rectal | 0.472 | 0.307‒0.725 | 0.001* | 0.472 | 0.304‒0.735 | 0.001* | |
| Gender | |||||||
| Male | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Female | 0.602 | 0.402‒0.902 | 0.014* | 0.569 | 0.377‒0.858 | 0.007* | |
| Tumor size | |||||||
| <5 cm | ‒ | 1 | ‒ | ||||
| ≥5 cm | 1.294 | 0.887‒1.888 | 0.182 | ||||
| Age | |||||||
| ≤67 years | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| >67 years | 3.315 | 2.188‒5.022 | 0.000** | 3.426 | 2.245‒5.227 | 0.000** | |
| Risk factor | |||||||
| 0 | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| 1 | 2.122 | 1.156‒3.893 | 0.015* | 2.037 | 1.105‒3.755 | 0.023* | |
| 2 | 3.742 | 2.013‒6.957 | 0.000** | 2.604 | 1.372‒4.942 | 0.003* | |
| 3 | 6.074 | 3.065‒12.037 | 0.000** | 3.564 | 1.732‒7.336 | 0.001* | |
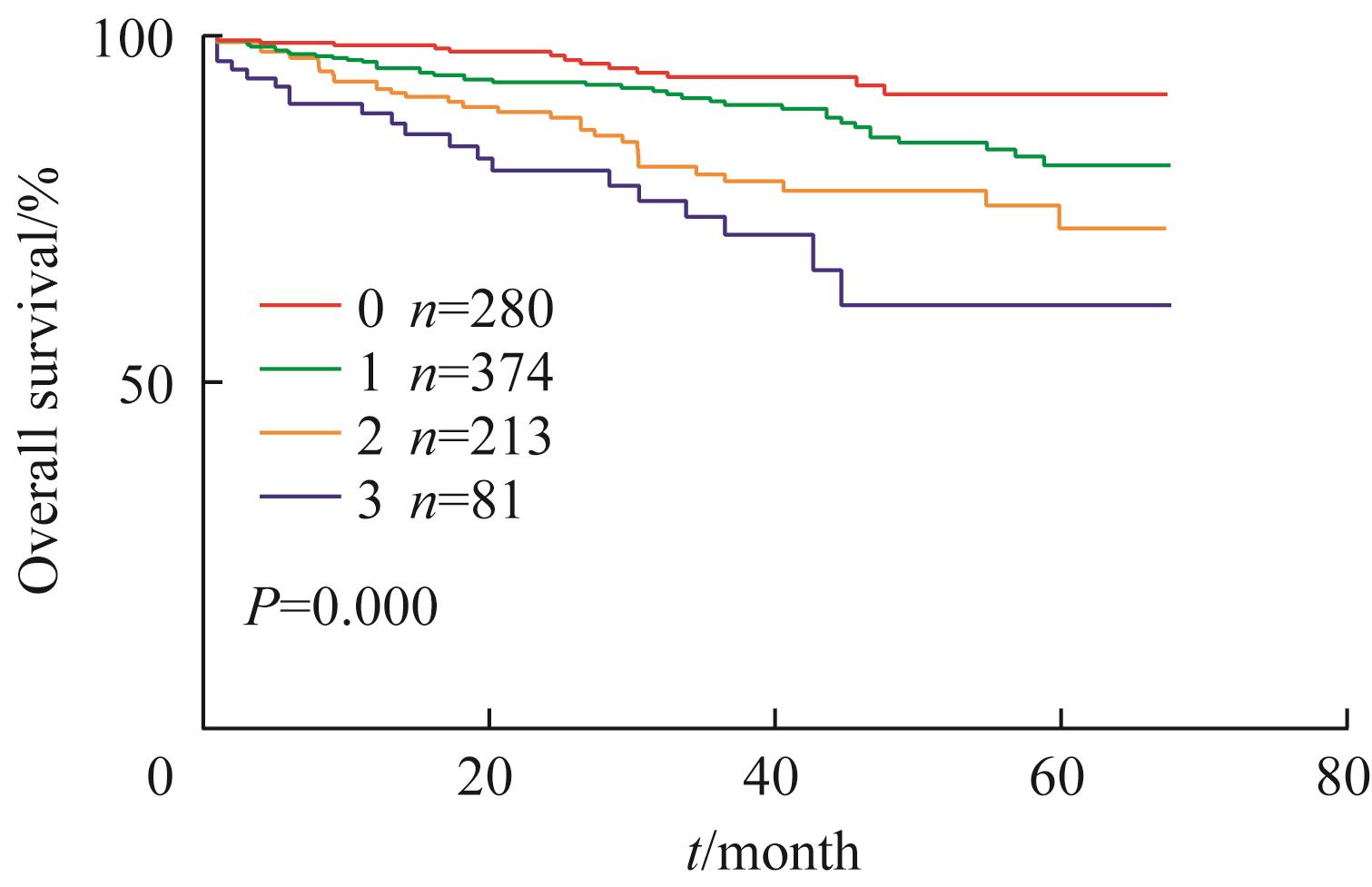
图1 CRC的Kaplan-Meier生存分析曲线Note:0 represents negative for LVI, PNI and TSR; 1 represents one positive for LVI, PNI and TSR; 2 represents two positive for LVI, PNI and TSR; 3 represents three positive for LVI, PNI and TSR.
Fig 1 Kaplan-Meier survival analysis for CRC
| Indicator | Group | P value | |
|---|---|---|---|
| Low-risk | High-risk | ||
| Gradea | 0.038* | ||
| Well | 80 (8.4) | 2 (0.2) | |
| Moderate | 667 (70.4) | 62 (6.5) | |
| Poor | 120 (12.7) | 17 (1.8) | |
| TNM Stagea | 0.000** | ||
| Ⅰ | 157 (16.6) | 3 (0.3) | |
| Ⅱ | 406 (42.8) | 15 (1.6) | |
| Ⅲ | 298 (31.4) | 61 (6.4) | |
| Ⅳ | 6 (0.7) | 2 (0.2) | |
| T Stagea | 0.014* | ||
| T1 | 36 (3.8) | 2 (0.2) | |
| T2 | 144 (15.2) | 4 (0.4) | |
| T3 | 187 (19.7) | 15 (1.6) | |
| T4 | 500 (52.7) | 60 (6.4) | |
| N Stagea | 0.000** | ||
| N0 | 564 (59.5) | 19 (2.0) | |
| N1 | 187 (19.7) | 34 (3.6) | |
| N2 | 116 (12.2) | 28 (3.0) | |
| Tumor location | 0.729 | ||
| Right | 283 (29.9) | 25 (2.6) | |
| Left | 232 (24.5) | 25 (2.6) | |
| Rectal | 352 (37.1) | 31 (3.3) | |
| Gendera | 0.009* | ||
| Male | 490 (51.7) | 58 (6.1) | |
| Female | 377 (39.8) | 23 (2.4) | |
| Tumor sizea | 0.888 | ||
| <5 cm | 539 (56.9) | 51 (5.4) | |
| ≥5 cm | 328 (34.6) | 30 (3.1) | |
| Agea | 66.0 (58.0‒74.0) | 65.0 (54.5‒75.5) | 0.538 |
| CEAb | 0.051 | ||
| Normal | 432 (58.5) | 35 (4.7) | |
| Abnormal | 240 (32.5) | 32 (4.3) | |
| CA199c | 0.001** | ||
| Normal | 540 (71.9) | 42 (5.6) | |
| Abnormal | 143 (19.0) | 26 (3.5) | |
| CA50d | 0.765 | ||
| Normal | 318 (83.2) | 30 (7.9) | |
| Abnormal | 30 (7.9) | 4 (1.0) | |
| CA125e | 0.398 | ||
| Normal | 334 (83.5) | 28 (7.0) | |
| Abnormal | 33 (8.3) | 5 (1.2) | |
| CA724f | 0.960 | ||
| Normal | 563 (77.4) | 57 (7.8) | |
| Abnormal | 97 (13.3) | 10 (1.5) | |
| KRASg | 0.433 | ||
| Wild type | 186 (51.2) | 27 (7.4) | |
| Mutant type | 135 (37.2) | 15 (4.2) | |
| NRASh | 0.604 | ||
| Wild type | 315 (86.3) | 42 (11.5) | |
| Mutant type | 8 (2.2) | 0 (0) | |
| BRAFi | 1.000 | ||
| Wild type | 235 (86.1) | 27 (9.9) | |
| Mutant type | 10 (3.7) | 1 (0.3) | |
| MMRj | 0.510 | ||
| pMMR | 381 (65.8) | 39 (6.7) | |
| dMMR | 147 (25.4) | 12 (2.1) | |
表2 高风险与低风险患者临床病理因素相关分析[ n (%)]
Tab 2 Correlation analysis of clinicopathological factors between high-risk and low-risk patients [n(%)]
| Indicator | Group | P value | |
|---|---|---|---|
| Low-risk | High-risk | ||
| Gradea | 0.038* | ||
| Well | 80 (8.4) | 2 (0.2) | |
| Moderate | 667 (70.4) | 62 (6.5) | |
| Poor | 120 (12.7) | 17 (1.8) | |
| TNM Stagea | 0.000** | ||
| Ⅰ | 157 (16.6) | 3 (0.3) | |
| Ⅱ | 406 (42.8) | 15 (1.6) | |
| Ⅲ | 298 (31.4) | 61 (6.4) | |
| Ⅳ | 6 (0.7) | 2 (0.2) | |
| T Stagea | 0.014* | ||
| T1 | 36 (3.8) | 2 (0.2) | |
| T2 | 144 (15.2) | 4 (0.4) | |
| T3 | 187 (19.7) | 15 (1.6) | |
| T4 | 500 (52.7) | 60 (6.4) | |
| N Stagea | 0.000** | ||
| N0 | 564 (59.5) | 19 (2.0) | |
| N1 | 187 (19.7) | 34 (3.6) | |
| N2 | 116 (12.2) | 28 (3.0) | |
| Tumor location | 0.729 | ||
| Right | 283 (29.9) | 25 (2.6) | |
| Left | 232 (24.5) | 25 (2.6) | |
| Rectal | 352 (37.1) | 31 (3.3) | |
| Gendera | 0.009* | ||
| Male | 490 (51.7) | 58 (6.1) | |
| Female | 377 (39.8) | 23 (2.4) | |
| Tumor sizea | 0.888 | ||
| <5 cm | 539 (56.9) | 51 (5.4) | |
| ≥5 cm | 328 (34.6) | 30 (3.1) | |
| Agea | 66.0 (58.0‒74.0) | 65.0 (54.5‒75.5) | 0.538 |
| CEAb | 0.051 | ||
| Normal | 432 (58.5) | 35 (4.7) | |
| Abnormal | 240 (32.5) | 32 (4.3) | |
| CA199c | 0.001** | ||
| Normal | 540 (71.9) | 42 (5.6) | |
| Abnormal | 143 (19.0) | 26 (3.5) | |
| CA50d | 0.765 | ||
| Normal | 318 (83.2) | 30 (7.9) | |
| Abnormal | 30 (7.9) | 4 (1.0) | |
| CA125e | 0.398 | ||
| Normal | 334 (83.5) | 28 (7.0) | |
| Abnormal | 33 (8.3) | 5 (1.2) | |
| CA724f | 0.960 | ||
| Normal | 563 (77.4) | 57 (7.8) | |
| Abnormal | 97 (13.3) | 10 (1.5) | |
| KRASg | 0.433 | ||
| Wild type | 186 (51.2) | 27 (7.4) | |
| Mutant type | 135 (37.2) | 15 (4.2) | |
| NRASh | 0.604 | ||
| Wild type | 315 (86.3) | 42 (11.5) | |
| Mutant type | 8 (2.2) | 0 (0) | |
| BRAFi | 1.000 | ||
| Wild type | 235 (86.1) | 27 (9.9) | |
| Mutant type | 10 (3.7) | 1 (0.3) | |
| MMRj | 0.510 | ||
| pMMR | 381 (65.8) | 39 (6.7) | |
| dMMR | 147 (25.4) | 12 (2.1) | |
| Indicator | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| HR | 95%CI | P value | HR | 95%CI | P value | ||
| Grade | |||||||
| Well | ‒ | 1 | ‒ | ||||
| Moderate | 2.333 | 0.945‒5.759 | 0.660 | ||||
| Poor | 3.824 | 1.451‒10.079 | 0.007 | ||||
| T Stage | |||||||
| T1 | ‒ | 1 | ‒ | ||||
| T2 | 1.897 | 0.240‒14.981 | 0.544 | ||||
| T3 | 2.201 | 0.291‒16.676 | 0.445 | ||||
| T4 | 6.070 | 0.845‒43.588 | 0.073 | ||||
| N Stage | |||||||
| N0 | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| N1 | 2.364 | 1.477‒3.784 | 0.000** | 1.971 | 1.211‒3.209 | 0.006* | |
| N2 | 5.832 | 3.725‒9.130 | 0.000** | 5.648 | 3.510‒9.087 | 0.000** | |
| Tumor location | |||||||
| Right | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Left | 0.461 | 0.281‒0.757 | 0.002* | 0.483 | 0.291‒0.803 | 0.005* | |
| Rectal | 0.472 | 0.307‒0.725 | 0.001* | 0.574 | 0.363‒0.906 | 0.017* | |
| Gender | |||||||
| Male | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Female | 0.602 | 0.402‒0.902 | 0.014* | 0.617 | 0.406‒0.937 | 0.023* | |
| Tumor size | |||||||
| <5 cm | ‒ | 1 | ‒ | ||||
| ≥5 cm | 1.294 | 0.887‒1.888 | 0.182 | ||||
| Age | |||||||
| ≤67 years | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| >67 years | 3.315 | 2.188‒5.022 | 0.000** | 3.354 | 2.183‒5.152 | 0.000** | |
| Risk group | |||||||
| Low | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| High | 2.876 | 1.769‒4.676 | 0.000** | 2.078 | 1.236‒3.496 | 0.006* | |
| CEA | |||||||
| Normal | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Abnormal | 2.463 | 1.561‒3.887 | 0.000** | 1.729 | 1.045‒2.859 | 0.033* | |
| CA199 | |||||||
| Normal | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Abnormal | 1.719 | 1.053‒2.806 | 0.030* | 0.701 | 0.385‒1.275 | 0.244 | |
| CA50 | |||||||
| Normal | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Abnormal | 2.478 | 1.095‒5.607 | 0.029* | 1.975 | 0.772‒5.050 | 0.155 | |
| CA125 | |||||||
| Normal | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Abnormal | 2.690 | 1.293‒5.598 | 0.008* | 1.752 | 0.815‒3.766 | 0.151 | |
| CA724 | |||||||
| Normal | ‒ | 1 | ‒ | ||||
| Abnormal | 1.044 | 0.548‒1.989 | 0.897 | ||||
| KRAS | |||||||
| Wild type | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Mutant type | 2.818 | 1.559‒5.092 | 0.001* | 2.048 | 1.108‒3.786 | 0.022* | |
| NRAS | |||||||
| Wild type | ‒ | 1 | ‒ | ||||
| Mutant type | 2.009 | 0.487‒8.283 | 0.334 | ||||
| BRAF | |||||||
| Wild type | ‒ | 1 | ‒ | ||||
| Mutant type | 2.242 | 0.534‒9.412 | 0.270 | ||||
| MMR | |||||||
| pMMR | ‒ | 1 | ‒ | ||||
| dMMR | 1.343 | 0.767‒2.351 | 0.301 | ||||
表3 CRC总体生存率影响因素的单因素和多因素COX 分析(SGH未匹配队列)
Tab 3 Univariate and multivariate COX analysis of influencing factors for overall survival of CRC (Unmatched queue of SGH)
| Indicator | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| HR | 95%CI | P value | HR | 95%CI | P value | ||
| Grade | |||||||
| Well | ‒ | 1 | ‒ | ||||
| Moderate | 2.333 | 0.945‒5.759 | 0.660 | ||||
| Poor | 3.824 | 1.451‒10.079 | 0.007 | ||||
| T Stage | |||||||
| T1 | ‒ | 1 | ‒ | ||||
| T2 | 1.897 | 0.240‒14.981 | 0.544 | ||||
| T3 | 2.201 | 0.291‒16.676 | 0.445 | ||||
| T4 | 6.070 | 0.845‒43.588 | 0.073 | ||||
| N Stage | |||||||
| N0 | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| N1 | 2.364 | 1.477‒3.784 | 0.000** | 1.971 | 1.211‒3.209 | 0.006* | |
| N2 | 5.832 | 3.725‒9.130 | 0.000** | 5.648 | 3.510‒9.087 | 0.000** | |
| Tumor location | |||||||
| Right | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Left | 0.461 | 0.281‒0.757 | 0.002* | 0.483 | 0.291‒0.803 | 0.005* | |
| Rectal | 0.472 | 0.307‒0.725 | 0.001* | 0.574 | 0.363‒0.906 | 0.017* | |
| Gender | |||||||
| Male | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Female | 0.602 | 0.402‒0.902 | 0.014* | 0.617 | 0.406‒0.937 | 0.023* | |
| Tumor size | |||||||
| <5 cm | ‒ | 1 | ‒ | ||||
| ≥5 cm | 1.294 | 0.887‒1.888 | 0.182 | ||||
| Age | |||||||
| ≤67 years | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| >67 years | 3.315 | 2.188‒5.022 | 0.000** | 3.354 | 2.183‒5.152 | 0.000** | |
| Risk group | |||||||
| Low | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| High | 2.876 | 1.769‒4.676 | 0.000** | 2.078 | 1.236‒3.496 | 0.006* | |
| CEA | |||||||
| Normal | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Abnormal | 2.463 | 1.561‒3.887 | 0.000** | 1.729 | 1.045‒2.859 | 0.033* | |
| CA199 | |||||||
| Normal | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Abnormal | 1.719 | 1.053‒2.806 | 0.030* | 0.701 | 0.385‒1.275 | 0.244 | |
| CA50 | |||||||
| Normal | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Abnormal | 2.478 | 1.095‒5.607 | 0.029* | 1.975 | 0.772‒5.050 | 0.155 | |
| CA125 | |||||||
| Normal | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Abnormal | 2.690 | 1.293‒5.598 | 0.008* | 1.752 | 0.815‒3.766 | 0.151 | |
| CA724 | |||||||
| Normal | ‒ | 1 | ‒ | ||||
| Abnormal | 1.044 | 0.548‒1.989 | 0.897 | ||||
| KRAS | |||||||
| Wild type | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Mutant type | 2.818 | 1.559‒5.092 | 0.001* | 2.048 | 1.108‒3.786 | 0.022* | |
| NRAS | |||||||
| Wild type | ‒ | 1 | ‒ | ||||
| Mutant type | 2.009 | 0.487‒8.283 | 0.334 | ||||
| BRAF | |||||||
| Wild type | ‒ | 1 | ‒ | ||||
| Mutant type | 2.242 | 0.534‒9.412 | 0.270 | ||||
| MMR | |||||||
| pMMR | ‒ | 1 | ‒ | ||||
| dMMR | 1.343 | 0.767‒2.351 | 0.301 | ||||
| Indicator | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| HR | 95%CI | P value | HR | 95%CI | P value | ||
| Grade | |||||||
| Well | ‒ | 1 | ‒ | ||||
| Moderate | 7 939.246 | 0‒3.338×1081 | 0.922 | ||||
| Poor | 14 304.201 | 0‒6.019×1081 | 0.916 | ||||
| T Stage | |||||||
| T1 | ‒ | ‒ | ‒ | ||||
| T2 | ‒ | 1 | ‒ | ||||
| T3 | 23 440.882 | 0‒2.765×10167 | 0.958 | ||||
| T4 | 75 016.020 | 0‒8.807×10167 | 0.953 | ||||
| N Stage | |||||||
| N0 | ‒ | 1 | ‒ | ||||
| N1 | 1.474 | 0.453‒4.793 | 0.519 | ||||
| N2 | 2.607 | 0.870‒8.192 | 0.086 | ||||
| Tumor location | |||||||
| Right | ‒ | 1 | ‒ | ||||
| Left | 0.500 | 0.204‒1.227 | 0.130 | ||||
| Rectal | 0.204 | 0.068‒0.615 | 0.005* | ||||
| Gender | |||||||
| Male | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Female | 0.602 | 0.402‒0.902 | 0.014* | 0.428 | 0.147‒1.246 | 0.120 | |
| Tumor size | |||||||
| <5 cm | ‒ | 1 | ‒ | ||||
| ≥5 cm | 1.846 | 0.855‒3.987 | 0.118 | ||||
| Age | |||||||
| ≤67 years | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| >67 years | 3.092 | 1.377‒6.944 | 0.006* | 2.890 | 1.286‒6.494 | 0.010* | |
| Risk group | |||||||
| Low | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| High | 2.483 | 1.078‒5.720 | 0.033* | 2.380 | 1.030‒5.502 | 0.042* | |
表4 CRC总体生存率影响因素的单因素和多因素COX 分析(SGH匹配队列)
Tab 4 Univariate and multivariate COX analysis of influencing factors for overall survival of CRC (matched queue of SGH)
| Indicator | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| HR | 95%CI | P value | HR | 95%CI | P value | ||
| Grade | |||||||
| Well | ‒ | 1 | ‒ | ||||
| Moderate | 7 939.246 | 0‒3.338×1081 | 0.922 | ||||
| Poor | 14 304.201 | 0‒6.019×1081 | 0.916 | ||||
| T Stage | |||||||
| T1 | ‒ | ‒ | ‒ | ||||
| T2 | ‒ | 1 | ‒ | ||||
| T3 | 23 440.882 | 0‒2.765×10167 | 0.958 | ||||
| T4 | 75 016.020 | 0‒8.807×10167 | 0.953 | ||||
| N Stage | |||||||
| N0 | ‒ | 1 | ‒ | ||||
| N1 | 1.474 | 0.453‒4.793 | 0.519 | ||||
| N2 | 2.607 | 0.870‒8.192 | 0.086 | ||||
| Tumor location | |||||||
| Right | ‒ | 1 | ‒ | ||||
| Left | 0.500 | 0.204‒1.227 | 0.130 | ||||
| Rectal | 0.204 | 0.068‒0.615 | 0.005* | ||||
| Gender | |||||||
| Male | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Female | 0.602 | 0.402‒0.902 | 0.014* | 0.428 | 0.147‒1.246 | 0.120 | |
| Tumor size | |||||||
| <5 cm | ‒ | 1 | ‒ | ||||
| ≥5 cm | 1.846 | 0.855‒3.987 | 0.118 | ||||
| Age | |||||||
| ≤67 years | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| >67 years | 3.092 | 1.377‒6.944 | 0.006* | 2.890 | 1.286‒6.494 | 0.010* | |
| Risk group | |||||||
| Low | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| High | 2.483 | 1.078‒5.720 | 0.033* | 2.380 | 1.030‒5.502 | 0.042* | |
| Indicator | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| HR | 95%CI | P value | HR | 95%CI | P value | ||
| Grade | |||||||
| Well | ‒ | 1 | ‒ | ||||
| Moderate | 0.975 | 0.424‒2.239 | 0.952 | ||||
| Poor | 2.183 | 0.813‒5.866 | 0.122 | ||||
| T Stage | |||||||
| T1 | ‒ | 1 | ‒ | ||||
| T2 | 12 594.988 | 0‒2.436×1059 | 0.884 | ||||
| T3 | 8 970.864 | 0‒1.730×1059 | 0.889 | ||||
| T4 | 7 939.965 | 0‒1.532×1059 | 0.890 | ||||
| N Stage | |||||||
| N0 | ‒ | 1 | ‒ | ||||
| N1 | 2.137 | 1.078‒4.237 | 0.030* | ||||
| N2 | 1.379 | 0.626‒3.038 | 0.426 | ||||
| Tumor location | |||||||
| Right | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Left | 0.409 | 0.183‒0.916 | 0.030* | 0.475 | 0.208‒1.085 | 0.077 | |
| Rectal | 0.440 | 0.219‒0.886 | 0.021* | 0.450 | 0.223‒0.906 | 0.025* | |
| Gender | |||||||
| Male | ‒ | 1 | ‒ | ||||
| Female | 0.708 | 0.386‒1.299 | 0.265 | ||||
| Tumor size | |||||||
| <5 cm | ‒ | 1 | ‒ | ||||
| ≥5 cm | 0.990 | 0.542‒1.808 | 0.975 | ||||
| Age | |||||||
| ≤67 years | ‒ | 1 | ‒ | ||||
| >67 years | 1.729 | 0.950‒3.147 | 0.073 | ||||
| Risk group | |||||||
| Low | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| High | 2.403 | 1.183‒4.882 | 0.015* | 2.121 | 1.024‒4.392 | 0.043* | |
表5 CRC总体生存率影响因素的单因素和多因素COX分析(TMA队列)
Tab 5 Univariate and multivariate COX analysis of influencing factors for overall survival of CRC (TMA cohort)
| Indicator | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| HR | 95%CI | P value | HR | 95%CI | P value | ||
| Grade | |||||||
| Well | ‒ | 1 | ‒ | ||||
| Moderate | 0.975 | 0.424‒2.239 | 0.952 | ||||
| Poor | 2.183 | 0.813‒5.866 | 0.122 | ||||
| T Stage | |||||||
| T1 | ‒ | 1 | ‒ | ||||
| T2 | 12 594.988 | 0‒2.436×1059 | 0.884 | ||||
| T3 | 8 970.864 | 0‒1.730×1059 | 0.889 | ||||
| T4 | 7 939.965 | 0‒1.532×1059 | 0.890 | ||||
| N Stage | |||||||
| N0 | ‒ | 1 | ‒ | ||||
| N1 | 2.137 | 1.078‒4.237 | 0.030* | ||||
| N2 | 1.379 | 0.626‒3.038 | 0.426 | ||||
| Tumor location | |||||||
| Right | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| Left | 0.409 | 0.183‒0.916 | 0.030* | 0.475 | 0.208‒1.085 | 0.077 | |
| Rectal | 0.440 | 0.219‒0.886 | 0.021* | 0.450 | 0.223‒0.906 | 0.025* | |
| Gender | |||||||
| Male | ‒ | 1 | ‒ | ||||
| Female | 0.708 | 0.386‒1.299 | 0.265 | ||||
| Tumor size | |||||||
| <5 cm | ‒ | 1 | ‒ | ||||
| ≥5 cm | 0.990 | 0.542‒1.808 | 0.975 | ||||
| Age | |||||||
| ≤67 years | ‒ | 1 | ‒ | ||||
| >67 years | 1.729 | 0.950‒3.147 | 0.073 | ||||
| Risk group | |||||||
| Low | ‒ | 1 | ‒ | ‒ | 1 | ‒ | |
| High | 2.403 | 1.183‒4.882 | 0.015* | 2.121 | 1.024‒4.392 | 0.043* | |
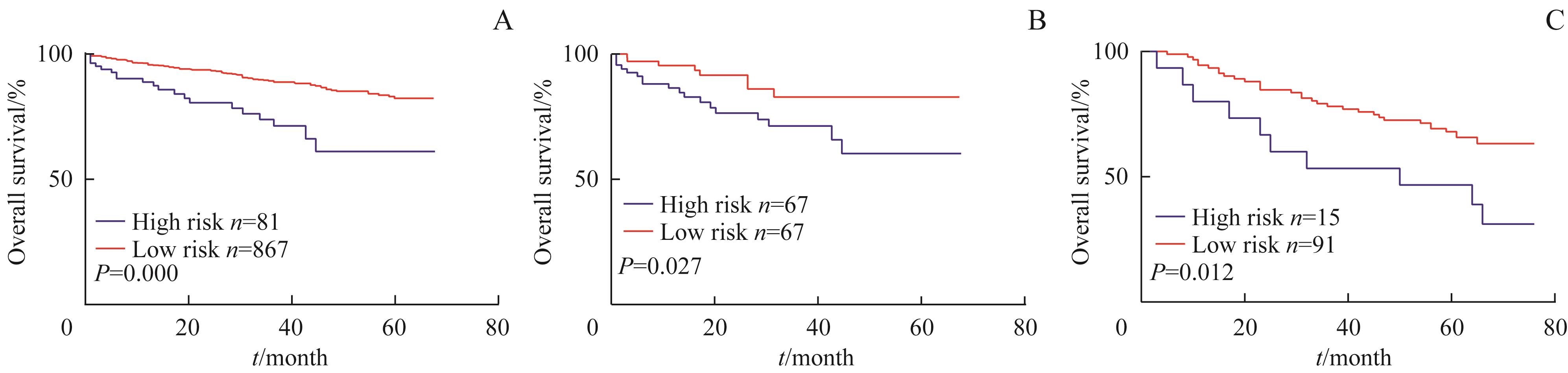
图2 高风险组与低风险组的Kaplan-Meier生存分析曲线Note:A. SGH cohort (no matching). B. SGH cohort (matching). C. TMA cohort.
Fig 2 Kaplan-Meier survival analysis for overall survival of high-risk group and low-risk group
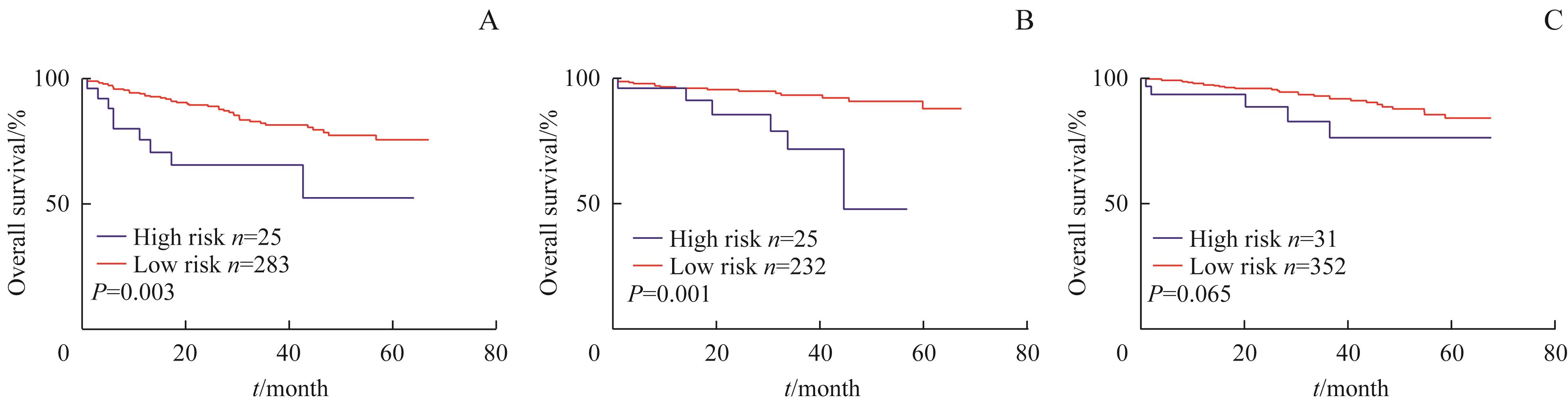
图3 高风险组与低风险组在肿瘤部位中的Kaplan-Meier生存分析曲线Note:A. Right-side colon cancer. B. Left-side colon cancer. C. Rectal cancer.
Fig 3 Kaplan-Meier survival analysis curves in tumor site between high risk group and low risk group
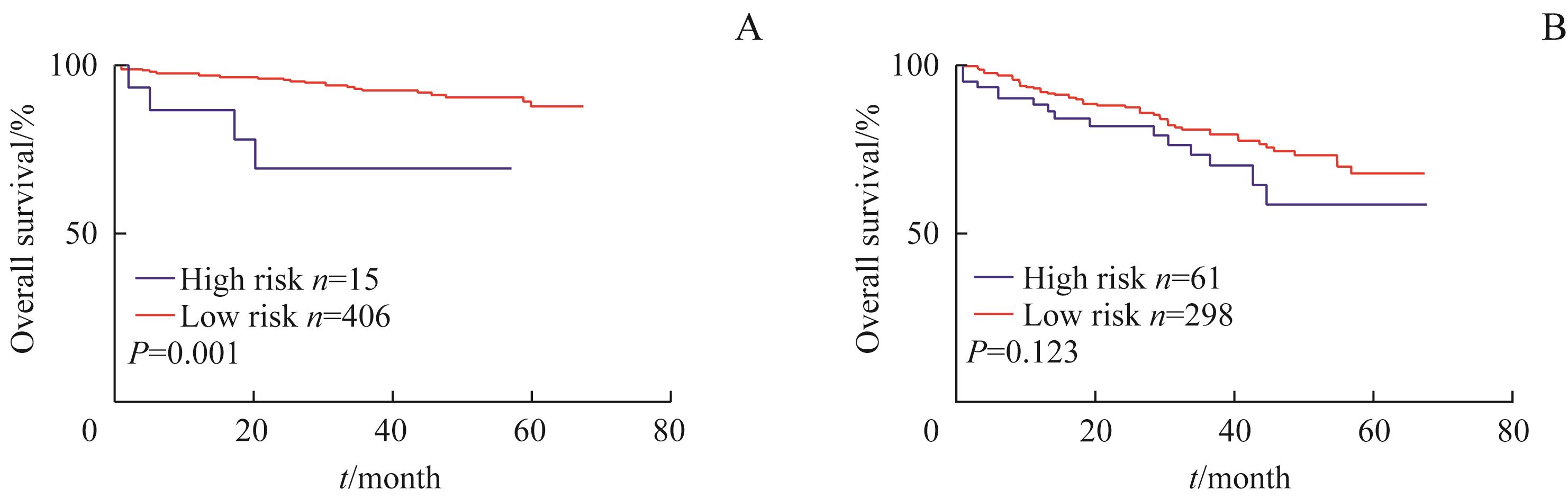
图4 高风险组与低风险组在TNM分期中的Kaplan-Meier生存分析曲线Note:A. Ⅱ stage. B. Ⅲ stage.
Fig 4 Kaplan-Meier survival analysis curves in TNM stage between high risk group and low risk group
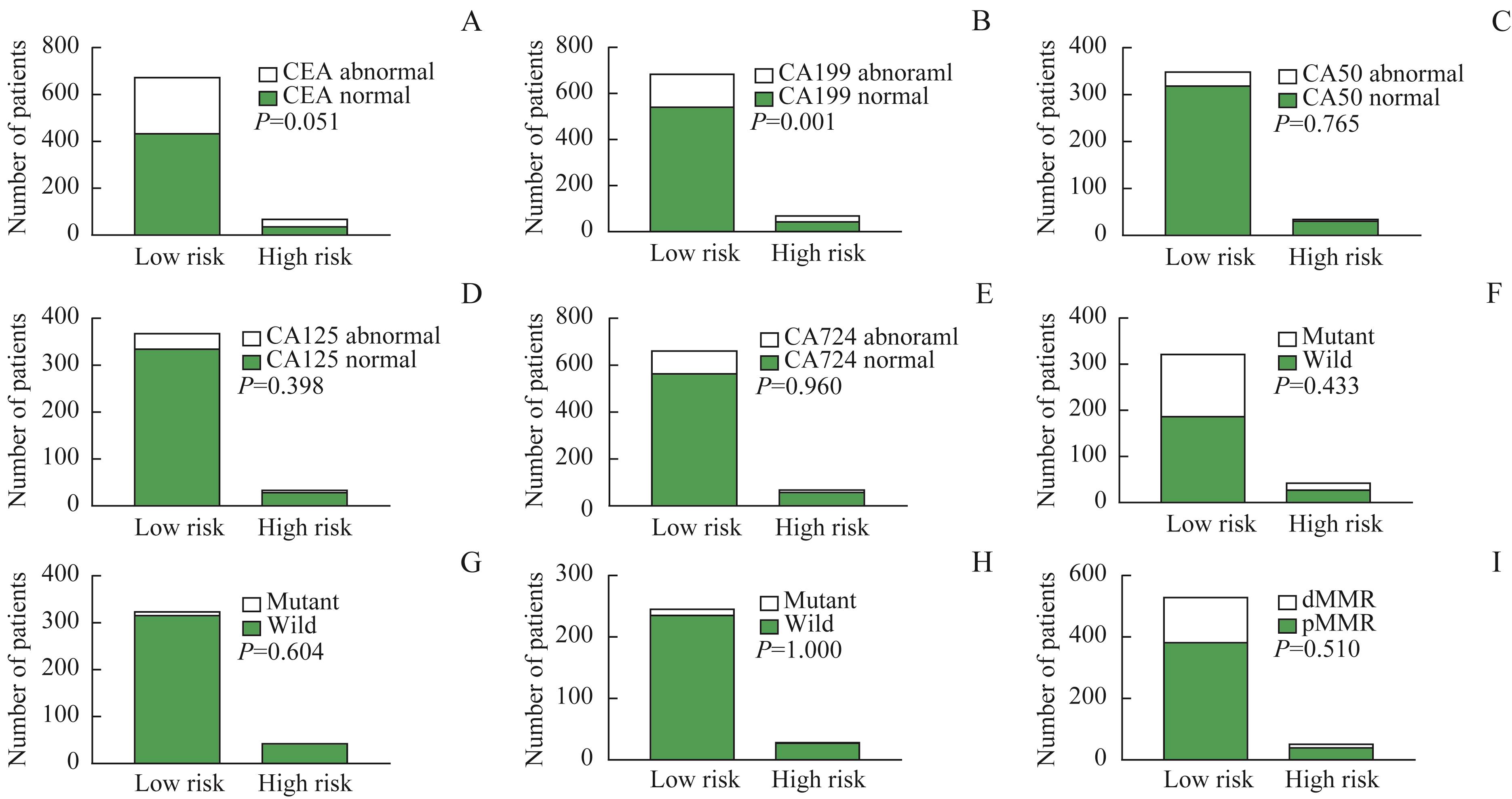
图5 高风险组与低风险组在术前血清肿瘤标志物、基因突变状态、错配修复基因状态分布差异Note:A. CEA. B. CA199. C. CA50. D. CA125. E. CA724. F. KRAS. G. NRAS. H. BRAF. I. MMR.
Fig 5 Distributional difference of preoperative serum tumor markers, gene mutation status and mismatch repair gene status for high-risk group and low-risk group

图6 高风险组与低风险组Kaplan-Meier生存分析曲线Note:A. CEA in high risk group. B. CEA in low risk group. C. CEA in combined risk group. D. CA199 in high risk group. E. CA199 in low risk group. F. CA199 in combined risk group. G. KRAS in high risk group. H. KRAS in low risk group. I. KRAS in combined risk group.
Fig 6 Kaplan-Meier survival analysis curves for high risk group and low risk group
| 1 | SUNG H, FERLAY J, SIEGEL R L, et al. Global cancer statistics 2020: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71(3): 209-249. |
| 2 | ZHENG R S, ZHANG S W, ZENG H M, et al. Cancer incidence and mortality in China, 2016[J]. J Natl Cancer Cent, 2022, 2(1): 1-9. |
| 3 | YUAN H, DONG Q J, ZHENG B A, et al. Lymphovascular invasion is a high risk factor for stage Ⅰ/Ⅱ colorectal cancer: a systematic review and meta-analysis[J]. Oncotarget, 2017, 8(28): 46565-46579. |
| 4 | JIANG H H, ZHANG Z Y, WANG X Y, et al. Prognostic significance of lymphovascular invasion in colorectal cancer and its association with genomic alterations[J]. World J Gastroenterol, 2019, 25(20): 2489-2502. |
| 5 | KNIJN N, MOGK S C, TEERENSTRA S, et al. Perineural invasion is a strong prognostic factor in colorectal cancer: a systematic review[J]. Am J Surg Pathol, 2016, 40(1): 103-112. |
| 6 | CONTE G A, QARI O, FASANO G A, et al. S100 staining adds to the prognostic significance of the combination of perineural invasion and lymphovascular invasion in colorectal cancer[J]. Appl Immunohistochem Mol Morphol, 2020, 28(5): 354-359. |
| 7 | MESKER W E, JUNGGEBURT J M C, SZUHAI K, et al. The carcinoma-stromal ratio of colon carcinoma is an independent factor for survival compared to lymph node status and tumor stage[J]. Cell Oncol, 2007, 29(5): 387-398. |
| 8 | LUO Z, FU Z M, LI T F, et al. Development and validation of the individualized prognostic nomograms in patients with right- and left-sided colon cancer[J]. Front Oncol, 2021, 11: 709835. |
| 9 | 李腾飞, 杨彦, 黄陈. 肿瘤间质比在Ⅱ、Ⅲ期结直肠癌患者预后评估中的价值[J]. 中华结直肠疾病电子杂志, 2021, 10(2): 158-163. |
| LI T F, YANG Y, HUANG C. The prognostic value of tumor stroma ratio in patients with stageⅡand Ⅲ colorevtal caner[J]. Chin J Colorec Dis ( Electronic Edition ), 2021, 10(2): 158-163. | |
| 10 | NASO J R, YANG H M, SCHAEFFER D F. Variability in synoptic reporting of colorectal cancer pT4a category and lymphovascular invasion[J]. Arch Pathol Lab Med, 2021, 145(3): 343-351. |
| 11 | ALOTAIBI A M, LEE J L, KIM J, et al. Prognostic and oncologic significance of perineural invasion in sporadic colorectal cancer[J]. Ann Surg Oncol, 2017, 24(6): 1626-1634. |
| 12 | LI T F, YU Z K, YANG Y, et al. Rapid multi-dynamic algorithm for gray image analysis of the stroma percentage on colorectal cancer[J]. J Cancer, 2021, 12(15): 4561-4573. |
| 13 | LIZARDO D Y, KUANG C Y, HAO S S, et al. Immunotherapy efficacy on mismatch repair-deficient colorectal cancer: from bench to bedside[J]. Biochim Biophys Acta Rev Cancer, 2020, 1874(2): 188447. |
| 14 | 蔡建, 王磊. 回眸2018: 聚焦结直肠癌研究领域[J]. 中华胃肠外科杂志, 2019, 22(1): 9-16. |
| CAI J, WANG L. Focus on colorectal cancer research, 2018[J]. Chin J Gastrointest Surg, 2019, 22(1): 9-16. | |
| 15 | DIENSTMANN R, MASON M J, SINICROPE F A, et al. Prediction of overall survival in stage Ⅱ and Ⅲ colon cancer beyond TNM system: a retrospective, pooled biomarker study[J]. Ann Oncol, 2017, 28(5): 1023-1031. |
| 16 | ZHANG C C, WANG Z, YANG Z, et al. Phase Ⅰ escalating-dose trial of CAR-T therapy targeting CEA+ metastatic colorectal cancers[J]. Mol Ther, 2017, 25(5): 1248-1258. |
| 17 | THOMSEN M, SKOVLUND E, SORBYE H, et al. Prognostic role of carcinoembryonic antigen and carbohydrate antigen 19-9 in metastatic colorectal cancer: a BRAF-mutant subset with high CA 19-9 level and poor outcome[J]. Br J Cancer, 2018, 118(12): 1609-1616. |
| 18 | ZHU G M, PEI L J, XIA H W, et al. Role of oncogenic KRAS in the prognosis, diagnosis and treatment of colorectal cancer[J]. Mol Cancer, 2021, 20(1): 143. |
| 19 | YOTHERS G, O'CONNELL M J, ALLEGRA C J, et al. Oxaliplatin as adjuvant therapy for colon cancer: updated results of NSABP C-07 trial, including survival and subset analyses[J]. J Clin Oncol, 2011, 29(28): 3768-3774. |
| 20 | BENSON A B, VENOOK A P, AL-HAWARY M M, et al. NCCN guidelines insights: colon cancer, version 2.2018[J]. J Natl Compr Canc Netw, 2018, 16(4): 359-369. |
| 21 | LABIANCA R, NORDLINGER B, BERETTA G D, et al. Early colon cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up[J]. Ann Oncol, 2013, 24(Suppl 6): vi64-vi72. |
| [1] | 何嘉音, 陈思远, 施晴, 张慕晨, 易红梅, 董磊, 钱樱, 王黎, 程澍, 许彭鹏, 赵维莅. 肾上腺累及的弥漫性大B细胞淋巴瘤患者临床病理特征、基因突变谱及预后分析[J]. 上海交通大学学报(医学版), 2025, 45(9): 1194-1201. |
| [2] | 陈思远, 施晴, 付迪, 王黎, 程澍, 许彭鹏, 赵维莅. 肺受累弥漫大B细胞淋巴瘤临床病理特征、基因突变谱及预后分析[J]. 上海交通大学学报(医学版), 2025, 45(9): 1214-1220. |
| [3] | 江怡, 黄晨浩, 李祉良, 吴珺玮, 赵任, 张弢. 1例KRAS突变的结直肠癌患者术前接受化疗联合免疫治疗的效果报道[J]. 上海交通大学学报(医学版), 2025, 45(9): 1256-1260. |
| [4] | 严治, 吴星玥, 姚卫芹, 颜灵芝, 金松, 商京晶, 施晓兰, 吴德沛, 傅琤琤. 免疫不全麻痹在新诊断多发性骨髓瘤患者中的动态变化及预后意义[J]. 上海交通大学学报(医学版), 2025, 45(7): 807-814. |
| [5] | 隋成亮, 沈艳莹, 刘泽兵. 上皮样血管内皮瘤12例临床病理学分析[J]. 上海交通大学学报(医学版), 2025, 45(7): 892-899. |
| [6] | 李卓杭, 于新迪, 任婧雅, 沈佳, 董素贞, 王伟. 主动脉缩窄端侧吻合纠治术后的神经系统预后分析[J]. 上海交通大学学报(医学版), 2025, 45(6): 753-759. |
| [7] | 汤开然, 冯成领, 韩邦旻. 基于单细胞测序与转录组测序构建M2巨噬细胞基因相关的前列腺癌预后模型[J]. 上海交通大学学报(医学版), 2025, 45(5): 549-561. |
| [8] | 黄润语, 张春叶, 张颖, 赵峥岩, 杨扬, 吴岚. 原发口腔外周T细胞淋巴瘤非特指型的特点分析[J]. 上海交通大学学报(医学版), 2025, 45(5): 653-660. |
| [9] | 许天芸, 沈奕茗, 姜萌. 射血分数改善型心力衰竭的临床管理: 治疗与维持[J]. 上海交通大学学报(医学版), 2025, 45(4): 493-499. |
| [10] | 刘田恬, 赵奕琳, 宁菁菁, 张育才, 王春霞. 儿童脓毒症预后相关长链非编码RNA筛选及竞争性内源RNA网络的构建[J]. 上海交通大学学报(医学版), 2025, 45(3): 282-291. |
| [11] | 陈佳莹, 褚以忞, 彭海霞. 结直肠癌无进展生存时间预测模型及影响因素研究[J]. 上海交通大学学报(医学版), 2025, 45(3): 324-334. |
| [12] | 梁乐斌, 陈慧芳, 赖淑静, 顾靓, 苏冰. 基于空间ATAC-seq技术的Apcmin/+小鼠结肠肿瘤表观特征分析[J]. 上海交通大学学报(医学版), 2025, 45(10): 1261-1270. |
| [13] | 高雨燕, 李伟, 王书婷, 岸本鹏子, 张洳源. 戒毒人员精神病理症状与药物成瘾的关系及心理痛苦的中介作用[J]. 上海交通大学学报(医学版), 2025, 45(1): 51-59. |
| [14] | 钱立恒, 温凯玲, 廖颖娜, 李书鑫, 聂惠贞. 分选链接蛋白1抑制结直肠癌细胞增殖和迁移的作用和机制研究[J]. 上海交通大学学报(医学版), 2024, 44(9): 1124-1135. |
| [15] | 王博恩, 陈思远, 施晴, 张慕晨, 易红梅, 董磊, 王黎, 程澍, 许彭鹏, 赵维莅. 肾脏累及的弥漫性大B细胞淋巴瘤患者临床病理特征[J]. 上海交通大学学报(医学版), 2024, 44(9): 1162-1168. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||