
上海交通大学学报(医学版) ›› 2022, Vol. 42 ›› Issue (12): 1712-1719.doi: 10.3969/j.issn.1674-8115.2022.12.009
收稿日期:2022-07-15
接受日期:2022-12-15
出版日期:2022-12-28
发布日期:2022-12-28
通讯作者:
朱晓东,E-mail:xinhuaxiaodong@126.com。作者简介:魏逸凡(1994—),女,住院医师,硕士生;电子信箱:weiyifan1994s@163.com。
WEI Yifan( ), ZHU Yueniu, KONG Xiangmei, XU Yaya, ZHU Xiaodong(
), ZHU Yueniu, KONG Xiangmei, XU Yaya, ZHU Xiaodong( )
)
Received:2022-07-15
Accepted:2022-12-15
Online:2022-12-28
Published:2022-12-28
Contact:
ZHU Xiaodong,E-mail:xinhuaxiaodong@126.com.摘要:
目的·探讨同步间歇指令通气(synchronized intermittent mandatory ventilation,SIMV)模式下机械通气早期小儿膈肌的形态与功能变化状况。方法·纳入2020年10月—2021年12月收治于上海交通大学医学院附属新华医院小儿急危重症医学科(Pediatric Intensive Care Unit,PICU)并接受机械通气治疗满96 h的患儿,通过床旁超声连续测量膈肌的相关数据,分析接受机械通气治疗后3个不同时间点(0、48、96 h)膈肌相关变化。各时间点间皮下脂肪厚度、皮下脂肪萎缩率、膈肌厚度、膈肌移动度比较均采用Kruskal-Wallis H检验,其中膈肌厚度进一步采用Bonferroni法校正显著性水平进行事后两两比较;各时间点膈肌收缩速度、膈肌增厚率、膈肌萎缩率比较均采用单因素方差分析。结果·纳入46例测量数据完整的患儿,平均年龄2.94(1.35,7.00)岁,男女各23例。导致需要机械通气治疗的主要病因为肺炎(52.17%);观察期间呼吸机的参数选择与机体氧合状态亦无明显差异(均P>0.05)。机械通气早期(96 h内)有50%的患儿出现腹部皮下脂肪的萎缩,36.96%患儿营养供给出现障碍(禁食与肠外营养支持),93.5%患儿接受糖皮质激素治疗,但3个时间点间腹部皮下脂肪的萎缩程度差异无统计学意义(均P>0.05)。床旁超声检测3个时间点的双侧膈肌厚度均发生明显萎缩(均P=0.000);机械通气48 h后右侧膈肌萎缩率为4.27%±7.36%,左侧膈肌萎缩率为3.88%±6.85%;机械通气96 h后右侧膈肌萎缩率为7.69%±7.74%,左侧膈肌萎缩率为7.55%±7.69%;双侧膈肌的萎缩率在机械通气最初的48 h内比48~96 h内更高(P=0.000)。3个时间点膈肌的功能相关指标(膈肌移动度、膈肌收缩速率、膈肌增厚率)比较,差异均无统计学意义。结论·床旁膈肌超声可以用来监测机械通气儿童的膈肌萎缩程度。SIMV模式的机械通气早期(96 h内)可引起小儿膈肌的结构性萎缩,且以最初48 h更为显著。膈肌早期形态学变化尚未影响患儿膈肌功能。
中图分类号:
魏逸凡, 朱月钮, 孔祥莓, 许雅雅, 朱晓东. 早期机械通气对小儿膈肌形态与功能的影响[J]. 上海交通大学学报(医学版), 2022, 42(12): 1712-1719.
WEI Yifan, ZHU Yueniu, KONG Xiangmei, XU Yaya, ZHU Xiaodong. Effects of early mechanical ventilation on the morphology and function of the diaphragm in children[J]. Journal of Shanghai Jiao Tong University (Medical Science), 2022, 42(12): 1712-1719.
| Indicator | M(Q1, Q3)/n(%) |
|---|---|
| General data | |
| Age/year | 2.94 (1.35, 7.00) |
| Male/female/n(%) | 23 (50.00)/23 (50.00) |
| Height/cm | 97.50 (78.00, 115.00) |
| Weight/kg | 13.08 (10.00, 22.00) |
| BMI/(kg·m-2) | 15.94 (13.55, 17.85) |
| Baseline abdominal fat thickness/mm | 0.70 (0.57, 0.89) |
| Abdominal fat atrophy/n(%) | 23 (50.00) |
| Body surface area/m2 | 0.60 (0.43, 0.87) |
| Clinical score system | |
| PCIS | 88.00 (79.00, 94.00) |
| PRISM Ⅲ | 6.00 (3.00, 10.00) |
| Primary disease | |
| Respiratory diseases/n(%) | 10 (21.74) |
| Neurological diseases/n(%) | 20 (43.48) |
| Hematologic diseases/n(%) | 4 (8.70) |
| Digestive diseases/n(%) | 5 (10.87) |
| Musculoskeletal diseases/n(%) | 1 (2.17) |
| Urinary diseases/n(%) | 1 (2.17) |
| Endocrine diseases/n(%) | 5 (10.87) |
| Etiology | |
| Pneumonia/n(%) | 24 (52.17) |
| CNS lesions/n(%) | 16 (34.78) |
| Septic pyemia/n(%) | 6 (13.04) |
| Complication | |
| MODS/n(%) | 6 (13.04) |
| Treatment | |
| Glucocorticoid/n(%) | 43 (93.50) |
| Parenteral nutrition/n(%) | 7 (15.22) |
| Fasting/n(%) | 10 (21.74) |
| Surgical interventions/n(%) | 26 (56.52) |
| Prognosis | |
| Weaning failure/n(%) | 18 (39.13) |
| Mortality in PICU/n(%) | 10 (21.74) |
| Duration of mechanical ventilation/d | 8.00 (7.00, 12.00) |
| Hospitalization days in PICU/d | 20.00 (11.00, 31.00) |
表1 46例患儿的基本资料
Tab 1 Main clinical characteristics of 46 children
| Indicator | M(Q1, Q3)/n(%) |
|---|---|
| General data | |
| Age/year | 2.94 (1.35, 7.00) |
| Male/female/n(%) | 23 (50.00)/23 (50.00) |
| Height/cm | 97.50 (78.00, 115.00) |
| Weight/kg | 13.08 (10.00, 22.00) |
| BMI/(kg·m-2) | 15.94 (13.55, 17.85) |
| Baseline abdominal fat thickness/mm | 0.70 (0.57, 0.89) |
| Abdominal fat atrophy/n(%) | 23 (50.00) |
| Body surface area/m2 | 0.60 (0.43, 0.87) |
| Clinical score system | |
| PCIS | 88.00 (79.00, 94.00) |
| PRISM Ⅲ | 6.00 (3.00, 10.00) |
| Primary disease | |
| Respiratory diseases/n(%) | 10 (21.74) |
| Neurological diseases/n(%) | 20 (43.48) |
| Hematologic diseases/n(%) | 4 (8.70) |
| Digestive diseases/n(%) | 5 (10.87) |
| Musculoskeletal diseases/n(%) | 1 (2.17) |
| Urinary diseases/n(%) | 1 (2.17) |
| Endocrine diseases/n(%) | 5 (10.87) |
| Etiology | |
| Pneumonia/n(%) | 24 (52.17) |
| CNS lesions/n(%) | 16 (34.78) |
| Septic pyemia/n(%) | 6 (13.04) |
| Complication | |
| MODS/n(%) | 6 (13.04) |
| Treatment | |
| Glucocorticoid/n(%) | 43 (93.50) |
| Parenteral nutrition/n(%) | 7 (15.22) |
| Fasting/n(%) | 10 (21.74) |
| Surgical interventions/n(%) | 26 (56.52) |
| Prognosis | |
| Weaning failure/n(%) | 18 (39.13) |
| Mortality in PICU/n(%) | 10 (21.74) |
| Duration of mechanical ventilation/d | 8.00 (7.00, 12.00) |
| Hospitalization days in PICU/d | 20.00 (11.00, 31.00) |
| Indicator | MV | H value | P value | ||
|---|---|---|---|---|---|
| 0 h | 48 h | 96 h | |||
| Oxygenation status | |||||
| SaO2/% | 97.80 (95.2, 99.40) | 97.00 (91.63, 99.23) | 97.50 (89.80, 99.23) | 0.73 | 0.70 |
| OI/mmHg | 349.55±166.03 | 305.97±159.04 | 321.24±161.00 | 0.90 | 0.41 |
| PaCO2/mmHg | 42.32±8.60 | 44.44±10.85 | 43.23±8.37 | 0.60 | 0.55 |
| Ventilator parameter | |||||
| Ppeak/cmH2O | 17.61±4.43 | 16.72±4.04 | 16.04±3.83 | 1.46 | 0.24 |
| Pmean/cmH2O | 8.83±3.48 | 8.26±3.28 | 7.49±2.60 | 1.78 | 0.17 |
| PEEP/cmH2O | 4.57±1.91 | 4.46±1.72 | 4.04±1.45 | 0.89 | 0.42 |
| FiO2/% | 36.76±11.43 | 35.07±10.63 | 34.40±10.12 | 0.39 | 0.68 |
| MVe/(L·min-1) | 3.38±1.83 | 3.21±1.64 | 3.03±1.48 | 0.42 | 0.66 |
| TV/(mL·kg-1) | 7.54±3.31 | 7.44±2.89 | 7.04±2.85 | 2.50 | 0.09 |
表2 PICU患儿机械通气后多个时间点的机体氧合状态及呼吸机参数设定比较
Tab 2 Comparison of the oxygenation status of children in PICU and the ventilator parameter settings at multiple time points after mechanical ventilation
| Indicator | MV | H value | P value | ||
|---|---|---|---|---|---|
| 0 h | 48 h | 96 h | |||
| Oxygenation status | |||||
| SaO2/% | 97.80 (95.2, 99.40) | 97.00 (91.63, 99.23) | 97.50 (89.80, 99.23) | 0.73 | 0.70 |
| OI/mmHg | 349.55±166.03 | 305.97±159.04 | 321.24±161.00 | 0.90 | 0.41 |
| PaCO2/mmHg | 42.32±8.60 | 44.44±10.85 | 43.23±8.37 | 0.60 | 0.55 |
| Ventilator parameter | |||||
| Ppeak/cmH2O | 17.61±4.43 | 16.72±4.04 | 16.04±3.83 | 1.46 | 0.24 |
| Pmean/cmH2O | 8.83±3.48 | 8.26±3.28 | 7.49±2.60 | 1.78 | 0.17 |
| PEEP/cmH2O | 4.57±1.91 | 4.46±1.72 | 4.04±1.45 | 0.89 | 0.42 |
| FiO2/% | 36.76±11.43 | 35.07±10.63 | 34.40±10.12 | 0.39 | 0.68 |
| MVe/(L·min-1) | 3.38±1.83 | 3.21±1.64 | 3.03±1.48 | 0.42 | 0.66 |
| TV/(mL·kg-1) | 7.54±3.31 | 7.44±2.89 | 7.04±2.85 | 2.50 | 0.09 |
| Indicator | MV | H value | P value | ||
|---|---|---|---|---|---|
| 0 h | 48 h | 96 h | |||
| Thickness /cm | 0.69 (0.56, 0.90) | 0.74 (0.57, 0.89) | 0.70 (0.56, 0.91) | 1.06 | 0.59 |
| Atrophy rate /% | 0 (0, 0) | -1.30 (-8.80, 5.77) | 0 (-6.92, 7.81) | 1.06 | 0.59 |
表3 PICU患儿机械通气96 h期间的腹部皮下脂肪比较
Tab 3 Comparison of the abdominal subcutaneous fat of children in PICU during 96 h of mechanical ventilation
| Indicator | MV | H value | P value | ||
|---|---|---|---|---|---|
| 0 h | 48 h | 96 h | |||
| Thickness /cm | 0.69 (0.56, 0.90) | 0.74 (0.57, 0.89) | 0.70 (0.56, 0.91) | 1.06 | 0.59 |
| Atrophy rate /% | 0 (0, 0) | -1.30 (-8.80, 5.77) | 0 (-6.92, 7.81) | 1.06 | 0.59 |
| Indicator | Position | MV | H value | P value | ||
|---|---|---|---|---|---|---|
| 0 h | 48 h | 96 h | ||||
| Diaphragmatic thickness/mm | R-I | 2.82±0.73 | 2.68±0.70 | 2.57±0.65 | 38.68 | 0.000 |
| R-E | 2.47±0.66 | 2.36±0.64 | 2.26±0.58 | 43.92 | 0.000 | |
| L-I | 2.58±0.71 | 2.46±0.70 | 2.35±0.67 | 37.19 | 0.000 | |
| L-E | 2.25±0.62 | 2.16±0.60 | 2.08±0.59 | 44.38 | 0.000 | |
| DE/mm | R | 6.20 (4.09, 8.60) | 5.85 (3.79, 7.72) | 6.09 (4.96, 7.89) | 2.48 | 0.290 |
| L | 5.60 (3.95, 7.25) | 6.15 (4.23, 9.40) | 5.75 (4.10, 8.86) | 4.19 | 0.120 | |
| DCV/(mm·s-1) | R | 6.59±3.61 | 5.35±2.83 | 6.79±4.09 | 4.74 | 0.090 |
| L | 6.28±3.73 | 6.16±3.43 | 6.42±3.49 | 1.65 | 0.440 | |
| DTF/% | R | 14.28±4.98 | 13.85±5.52 | 13.43±5.02 | 0.54 | 0.760 |
| L | 14.75±5.70 | 13.64±4.44 | 13.37±4.77 | 0.84 | 0.660 | |
| DAR/% | R | ‒ | 4.27±7.36 | 7.69±7.74 | 43.92 | 0.000 |
| L | ‒ | 3.88±6.85 | 7.55±7.69 | 37.19 | 0.000 | |
表4 PICU患儿机械通气早期的膈肌床旁超声数据比较
Tab 4 Comparison of the diaphragmatic bedside ultrasound data of children in PICU during early-stage mechanical ventilation
| Indicator | Position | MV | H value | P value | ||
|---|---|---|---|---|---|---|
| 0 h | 48 h | 96 h | ||||
| Diaphragmatic thickness/mm | R-I | 2.82±0.73 | 2.68±0.70 | 2.57±0.65 | 38.68 | 0.000 |
| R-E | 2.47±0.66 | 2.36±0.64 | 2.26±0.58 | 43.92 | 0.000 | |
| L-I | 2.58±0.71 | 2.46±0.70 | 2.35±0.67 | 37.19 | 0.000 | |
| L-E | 2.25±0.62 | 2.16±0.60 | 2.08±0.59 | 44.38 | 0.000 | |
| DE/mm | R | 6.20 (4.09, 8.60) | 5.85 (3.79, 7.72) | 6.09 (4.96, 7.89) | 2.48 | 0.290 |
| L | 5.60 (3.95, 7.25) | 6.15 (4.23, 9.40) | 5.75 (4.10, 8.86) | 4.19 | 0.120 | |
| DCV/(mm·s-1) | R | 6.59±3.61 | 5.35±2.83 | 6.79±4.09 | 4.74 | 0.090 |
| L | 6.28±3.73 | 6.16±3.43 | 6.42±3.49 | 1.65 | 0.440 | |
| DTF/% | R | 14.28±4.98 | 13.85±5.52 | 13.43±5.02 | 0.54 | 0.760 |
| L | 14.75±5.70 | 13.64±4.44 | 13.37±4.77 | 0.84 | 0.660 | |
| DAR/% | R | ‒ | 4.27±7.36 | 7.69±7.74 | 43.92 | 0.000 |
| L | ‒ | 3.88±6.85 | 7.55±7.69 | 37.19 | 0.000 | |
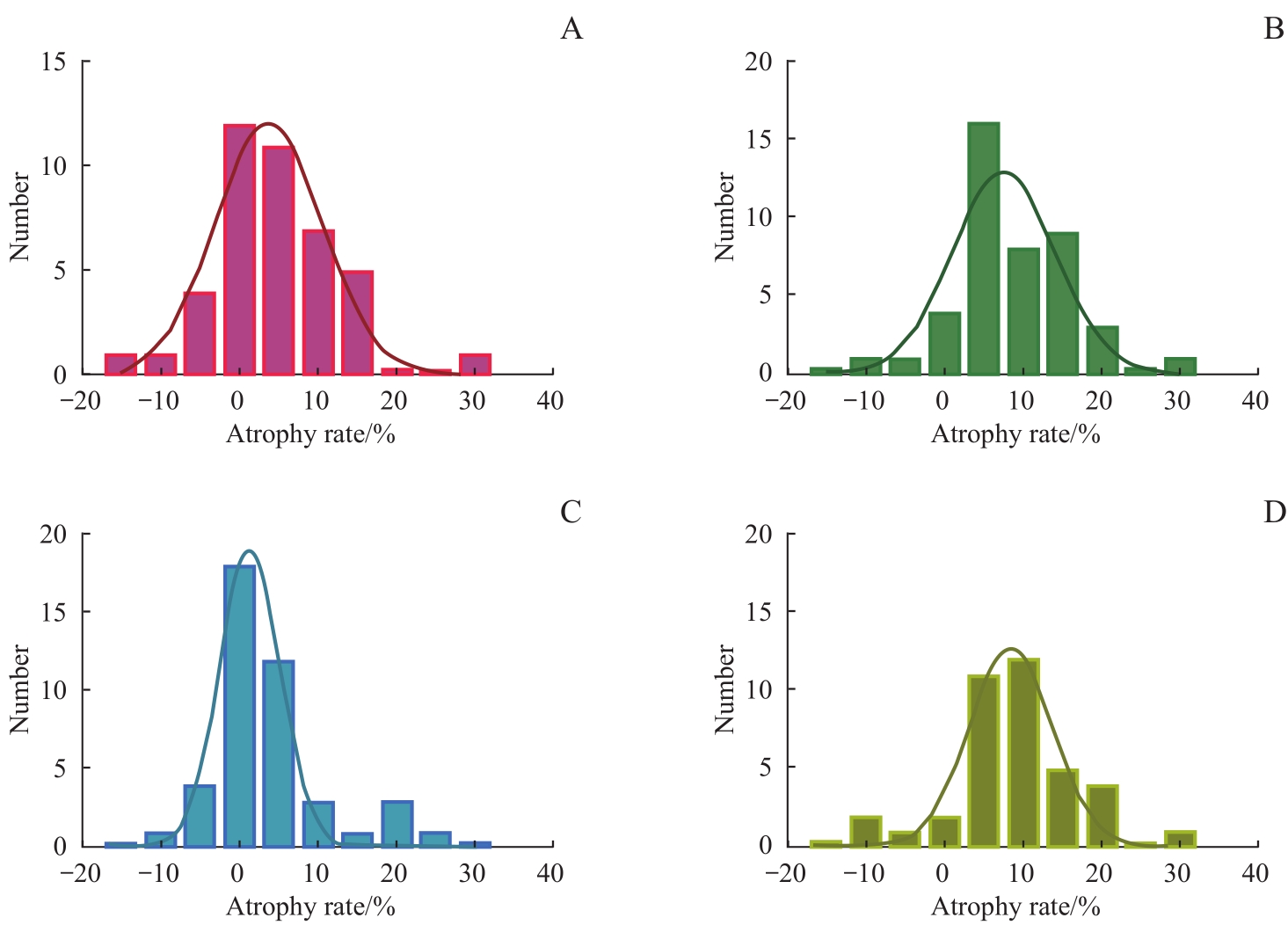
图1 机械通气48 h、96 h后膈肌萎缩率频数分布Note: A. Frequency distribution of atrophy rate of right diaphragm after 48 h of mechanical ventilation. B. Frequency distribution of atrophy rate of right diaphragm after 96 h of mechanical ventilation. C. Frequency distribution of atrophy rate of left diaphragm after 48 h of mechanical ventilation.D. Frequency distribution of atrophy rate of left diaphragm after 96 h of mechanical ventilation.
Fig1 Distribution of diaphragm atrophy rate after 48 h and 96 h of mechanical ventilation
| 1 | TOBIN M J, LAGHI F, JUBRAN A. Narrative review: ventilator-induced respiratory muscle weakness[J]. Ann Intern Med, 2010, 153(4): 240-245. |
| 2 | DE JONGHE B, BASTUJI-GARIN S, DURAND M C, et al. Respiratory weakness is associated with limb weakness and delayed weaning in critical illness[J]. Crit Care Med, 2007, 35(9): 2007-2015. |
| 3 | DEMOULE A, MOLINARI N, JUNG B, et al. Patterns of diaphragm function in critically ill patients receiving prolonged mechanical ventilation: a prospective longitudinal study[J]. Ann Inten Care, 2016, 6(1): 75. |
| 4 | BÉDUNEAU G, PHAM T, SCHORTGEN F, et al. Epidemiology of weaning outcome according to a new definition. the WIND study[J]. Am J Respir Crit Care Med, 2017, 195(6): 772-783. |
| 5 | DRES M, DUBÉ B P, MAYAUX J, et al. Coexistence and impact of limb muscle and diaphragm weakness at time of liberation from mechanical ventilation in medical intensive care unit patients[J]. Am J Respir Crit Care Med, 2017, 195(1): 57-66. |
| 6 | KIM W Y, SUH H J, HONG S B, et al. Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation[J]. Crit Care Med, 2011, 39(12): 2627-2630. |
| 7 | GOLIGHER E C, DRES M, FAN E, et al. Mechanical ventilation-induced diaphragm atrophy strongly impacts clinical outcomes[J]. Am J Respir Crit Care Med, 2018, 197(2): 204-213. |
| 8 | DAMUTH E, MITCHELL J A, BARTOCK J L, et al. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and meta-analysis[J]. Lancet Respir Med, 2015, 3(7): 544-553. |
| 9 | GROSU H B, LEE Y I, LEE J, et al. Diaphragm muscle thinning in patients who are mechanically ventilated[J]. Chest, 2012, 142(6): 1455-1460. |
| 10 | LEVINE S, NGUYEN T, TAYLOR N, et al. Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans[J]. N Engl J Med, 2008, 358(13): 1327-1335. |
| 11 | POWERS S K, SHANELY R A, COOMBES J S, et al. Mechanical ventilation results in progressive contractile dysfunction in the diaphragm[J]. J Appl Physiol (1985), 2002, 92(5): 1851-1858. |
| 12 | JABER S, PETROF B J, JUNG B, et al. Rapidly progressive diaphragmatic weakness and injury during mechanical ventilation in humans[J]. Am J Respir Crit Care Med, 2011, 183(3): 364-371. |
| 13 | SHANELY R A, ZERGEROGLU M A, LENNON SL, et al. Mechanical ventilation-induced diaphragmatic atrophy is associated with oxidative injury and increased proteolytic activity[J]. Am J Respir Crit Care Med, 2002, 166(10): 1369-1374. |
| 14 | GOLIGHER E C, FAN E, HERRIDGE M S, et al. Evolution of diaphragm thickness during mechanical ventilation. impact of inspiratory effort[J]. Am J Respir Crit Care Med, 2015, 192(9): 1080-1088. |
| 15 | OROZCO-LEVI M, LLORETA J, MINGUELLA J, et al. Injury of the human diaphragm associated with exertion and chronic obstructive pulmonary disease[J]. Am J Respir Crit Care Med, 2001, 164(9): 1734-1739. |
| 16 | GOLIGHER E C, LAGHI F, DETSKY M E, et al. Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity[J]. Intensive Care Med, 2015, 41(4): 642-649. |
| 17 | FAYSSOIL A, BEHIN A, OGNA A, et al. Diaphragm: pathophysiology and ultrasound imaging in neuromuscular disorders[J]. J Neuromuscul Dis, 2018, 5(1): 1-10. |
| 18 | FARIAS J A, FRUTOS F, ESTEBAN A, et al. What is the daily practice of mechanical ventilation in pediatric intensive care units? A multicenter study[J]. Intensive Care Med, 2004, 30(5): 918-925. |
| 19 | TAKAZAKURA R, TAKAHASHI M, NITTA N, et al. Diaphragmatic motion in the sitting and supine positions: healthy subject study using a vertically open magnetic resonance system[J]. J Magn Reson Imaging, 2004, 19(5): 605-609. |
| 20 | YAMAGUTI W P, PAULIN E, SHIBAO S, et al. Ultrasound evaluation of diaphragmatic mobility in different postures in healthy subjects[J]. J Bras Pneumol, 2007, 33(4): 407-413. |
| 21 | VIVIER E, MEKONTSO DESSAP A, DIMASSI S, et al. Diaphragm ultrasonography to estimate the work of breathing during non-invasive ventilation[J]. Intensive Care Med, 2012, 38(5): 796-803. |
| 22 | MATAMIS D, SOILEMEZI E, TSAGOURIAS M, et al. Sonographic evaluation of the diaphragm in critically ill patients. Technique and clinical applications[J]. Intensive Care Med, 2013, 39(5): 801-810. |
| 23 | MCCOOL F D, CONOMOS P, BENDITT J O, et al. Maximal inspiratory pressures and dimensions of the diaphragm[J]. Am J Respir Crit Care Med, 1997, 155(4): 1329-1334. |
| 24 | COHN D, BENDITT J O, EVELOFF S, et al. Diaphragm thickening during inspiration[J]. J Appl Physiol (1985), 1997, 83(1): 291-296. |
| 25 | LIU Y Y, LI L F. Ventilator-induced diaphragm dysfunction in critical illness[J]. Exp Biol Med (Maywood), 2018, 243(17/18): 1329-1337. |
| 26 | POWERS S K, WIGGS M P, SOLLANEK K J, et al. Ventilator-induced diaphragm dysfunction: cause and effect[J]. Am J Physiol Regul Integr Comp Physiol, 2013, 305(5): R464-R477. |
| 27 | POWERS S K, KAVAZIS A N, LEVINE S. Prolonged mechanical ventilation alters diaphragmatic structure and function[J]. Crit Care Med, 2009, 37(10 Suppl): S347-S353. |
| 28 | SCHEPENS T, VERBRUGGHE W, DAMS K, et al. The course of diaphragm atrophy in ventilated patients assessed with ultrasound: a longitudinal cohort study[J]. Crit Care, 2015, 19: 422. |
| 29 | IJLAND M M, LEMSON J, VAN DER HOEVEN J G, et al. The impact of critical illness on the expiratory muscles and the diaphragm assessed by ultrasound in mechanical ventilated children[J]. Ann Intensive Care, 2020, 10(1): 115. |
| 30 | GLAU C L, CONLON T W, HIMEBAUCH A S, et al. Progressive diaphragm atrophy in pediatric acute respiratory failure[J]. Pediatr Crit Care Med, 2018, 19(5): 406-411. |
| 31 | JOHNSON R W, NG K W P, DIETZ A R, et al. Muscle atrophy in mechanically-ventilated critically ill children[J]. PLoS One, 2018, 13(12): e0207720. |
| 32 | LEE E P, HSIA S H, HSIAO H F, et al. Evaluation of diaphragmatic function in mechanically ventilated children: an ultrasound study[J]. PLoS One, 2017, 12(8): e0183560. |
| 33 | GRASSI A, FERLICCA D, LUPIERI E, et al. Assisted mechanical ventilation promotes recovery of diaphragmatic thickness in critically ill patients: a prospective observational study[J]. Crit Care, 2020, 24: 85. |
| 34 | ZAMBON M, BECCARIA P, MATSUNO J, et al. Mechanical ventilation and diaphragmatic atrophy in critically ill patients: an ultrasound study[J]. Crit Care Med, 2016, 44(7): 1347-1352. |
| 35 | POWERS S K, DECRAMER M, GAYAN-RAMIREZ G, et al. Pressure support ventilation attenuates ventilator-induced protein modifications in the diaphragm[J]. Crit Care, 2008, 12(6): 191. |
| 36 | DEVOTO G, GALLO F, MARCHELLO C, et al. Prealbumin serum concentrations as a useful tool in the assessment of malnutrition in hospitalized patients[J]. Clin Chem, 2006, 52(12): 2281-2285. |
| 37 | JIANG J R. Ultrasonographic evaluation of liver/spleen movements and extubation outcome[J]. Chest, 2004, 126(1): 179-185. |
| 38 | SUMMERHILL E M, EL-SAMEED Y A, GLIDDEN T J, et al. Monitoring recovery from diaphragm paralysis with ultrasound[J]. Chest, 2008, 133(3): 737-743. |
| 39 | DININO E, GARTMAN E J, SETHI J M, et al. Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation[J]. Thorax, 2014, 69(5): 423-427. |
| 40 | FARGHALY S, HASAN A A. Diaphragm ultrasound as a new method to predict extubation outcome in mechanically ventilated patients[J]. Aust Crit Care, 2017, 30(1): 37-43. |
| 41 | GOTTESMAN E, MCCOOL F D. Ultrasound evaluation of the paralyzed diaphragm[J]. Am J Respir Crit Care Med, 1997, 155(5): 1570-1574. |
| 42 | ZAMBON M, GRECO M, BOCCHINO S, et al. Assessment of diaphragmatic dysfunction in the critically ill patient with ultrasound: a systematic review[J]. Intensive Care Med, 2017, 43(1): 29-38. |
| 43 | NEWTH C J L, VENKATARAMAN S, WILLSON D F, et al. Weaning and extubation readiness in pediatric patients[J]. Pediatr Crit Care Med, 2009, 10(1): 1-11. |
| 44 | DOORDUIN J, VAN HEES H W H, VAN DER HOEVEN J G, et al. Monitoring of the respiratory muscles in the critically ill[J]. Am J Respir Crit Care Med, 2013, 187(1): 20-27. |
| 45 | CATTAPAN S E, LAGHI F, TOBIN M J. Can diaphragmatic contractility be assessed by airway twitch pressure in mechanically ventilated patients? [J]. Thorax, 2003, 58(1): 58-62. |
| [1] | 超声引导儿童神经阻滞中国专家共识(2025版)编写组. 超声引导儿童神经阻滞中国专家共识(2025版)[J]. 上海交通大学学报(医学版), 2025, 45(9): 1079-1098. |
| [2] | 王治琪, 王莹. 儿童炎症性肠病相关贫血的诊治研究进展[J]. 上海交通大学学报(医学版), 2025, 45(9): 1232-1238. |
| [3] | 蒋婕, 张泓, 伦赫远, 潘芬, 于方圆, 何平. 儿童肺炎克雷伯菌感染分子流行病学特征[J]. 上海交通大学学报(医学版), 2025, 45(8): 1027-1034. |
| [4] | 梁书源, 叶宝英, 程蔚蔚. 超声指标和血液指标预测胎儿生长受限的研究现状[J]. 上海交通大学学报(医学版), 2025, 45(8): 1059-1065. |
| [5] | 何晨, 颜斯蕾, 周维涛, 凌勇, 于宁宁, 蒋鲲, 钱莉玲. 囊性纤维化合并变应性支气管肺曲菌病的临床分析及文献整合研究[J]. 上海交通大学学报(医学版), 2025, 45(8): 1066-1073. |
| [6] | 陆晔峰, 高磊青, 倪晓筱, 富晶晶. 儿童肝移植术后早期血糖及血脂的多时间点监测与影响因素分析[J]. 上海交通大学学报(医学版), 2025, 45(4): 443-451. |
| [7] | 刘田恬, 赵奕琳, 宁菁菁, 张育才, 王春霞. 儿童脓毒症预后相关长链非编码RNA筛选及竞争性内源RNA网络的构建[J]. 上海交通大学学报(医学版), 2025, 45(3): 282-291. |
| [8] | 张兰兰, 韩旭, 李牛, 王剑, 李淑元. 无创产前检测对17p12区域拷贝数变异的检测效能[J]. 上海交通大学学报(医学版), 2025, 45(3): 310-316. |
| [9] | 刘楚萱, 左佳鑫, 熊屏. 基于超声评分参数及临床指标的列线图鉴别原发性干燥综合征与IgG4相关唾液腺炎[J]. 上海交通大学学报(医学版), 2025, 45(3): 373-380. |
| [10] | 沈浩亮, 袁恺豪, 余磊, 阳娜娜, 王逸平, 赵宏胜, 郭凤梅, 孙晨靓. 膈肌联合肋间肌超声对脓毒症机械通气患者脱机评估的价值[J]. 上海交通大学学报(医学版), 2025, 45(2): 186-193. |
| [11] | 马瑞琳, 刘雨, 徐桂香, 史昊然, 崔俭俭, 杨泽俊, 毛艳, 赵茵. 子痫前期大鼠模型子宫动脉、脐动脉、大脑中动脉超声多普勒参数与胎盘血管病理及妊娠结局的关系[J]. 上海交通大学学报(医学版), 2024, 44(5): 543-551. |
| [12] | 刘美伶, 周亚兵, 王晓强. 儿童神经纤维瘤病1型颅内肿瘤性病变的治疗进展[J]. 上海交通大学学报(医学版), 2024, 44(3): 399-406. |
| [13] | 姜允丽, 李爱求, 肖艳赏, 李田田, 胡亚晨, 张潇潇, 吴蓓蓉. 基于EMS管理模式的延续性护理在学龄前喘息性疾病儿童中的应用观察[J]. 上海交通大学学报(医学版), 2024, 44(2): 228-236. |
| [14] | 胡灿芳, 钟传钰, 曹立. 神经调控技术在帕金森病治疗中的应用研究进展[J]. 上海交通大学学报(医学版), 2024, 44(2): 258-263. |
| [15] | 黄勤, 黄缨, 李文. 输卵管复合妊娠的超声检查时间探讨[J]. 上海交通大学学报(医学版), 2024, 44(12): 1545-1551. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||